Abstract
Objective
Our objective is to develop risk prediction models for moderate/severe bronchopulmonary dysplasia (BPD) and BPD and/or death in very-low-birth-weight infants (VLBWI) at birth, 3, 7, and 14 postnatal days.
Study design
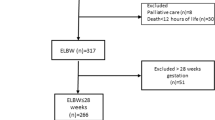
It is a multicenter study including 16,407 infants weighing 500–1500 g (2001–2015) from the Neocosur Network. BPD was defined as oxygen dependency at 36 weeks. Variables were selected using forward logistic regression models. Predictive values were evaluated using the ROC curve.
Results
In total, 2580 (15.7%) presented BPD and 6121 (37.3%) BPD/death. The AUC values for the BPD models were 0.788, 0.818, 0.827, and 0.894 respectively. For BPD/death, the AUC values were 0.860, 0.869, 0.867, and 0.906. BW and gestational age had higher contribution at birth; at later ages, the length of oxygen therapy and ventilation had the highest contribution. All AUC values were statistically significant when compared with a neutral value of 0.5 (p-value < 0.001).
Conclusions
We developed high predictive power models for moderate/severe BPD and BPD/death at four postnatal ages.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout


Similar content being viewed by others
References
Steinhorn R, Davis JM, Göpel W, Jobe A, Abman S, Laughon M, et al. Chronic pulmonary insufficiency of prematurity: developing optimal endpoints for drug development. J Pediatr. 2017;191:15–21.
Northway WH Jr, Rosan RC, Porter DY. Pulmonary disease following respiratory therapy of hyaline-membrane disease. Bronchopulmonary displasia. N Engl J Med. 1967;276:357–68.
Bancalari E, Abdenour GE, Feller R, Gannon J. Bronchopulmonary dysplasia: clinical presentation. J Pediatr. 1979;95(5 Pt 2):819–23.
Shennan A, Dunn MS, Ohlsson A, Lennox K, Hoskins EM. Abnormal pulmonary outcomes in premature infants: prediction from oxygen requirement in the neonatal period. Pediatrics 1988;82:527–32.
Jobe AH, Bancalari E. Bronchopulmonary dysplasia. Am J Respir Critic Care Med. 2001;163:1723–9.
Tapia JL, Agost D, Alegria A, Standen J, Escobar M, Grandi C, et al. Bronchopulmonary dysplasia: incidence, risk factors and resource utilization in a population of South American very low birth weight infants. J Pediatr. 2006;82:15–20.
Higgins R, Jobe AH, Koso-Thomas M, Bancalari E, Viscardi RM, Hartert TV, et al. Bronchopulmonary dysplasia: executive summary of a workshop. J Pediatr. 2018;197:300–8.
Klinger G, Sokolover N, Bokyo V, Sirota L, Lerner-Geva L, Reichman B. Israel neonatal network. perinatal risk factors for bronchopulmonary dysplasia in a national cohort of very-low-birthweight infants. Am J Obstet Gynecol. 2013;208:e1–9.
Horbar JD, Edwards EM, Greenberg LT, Morrow KA, Soll RF, Buus-Frank ME, Buzas JS. Variation in performance of neonatal intensive care units in the united states. JAMA Pediatr. 2017;171:e164396.
Isayama T, Lee SK, Mori R, Kusuda S, Fujimura M, Ye XY, Shah PS. Canadian neonatal network; neonatal research network of Japan. Comparison of mortality and morbidity of very low birth weight infants between Canada and Japan. Pediatrics. 2012;130:e957–65.
Fernández R, D’Apremont I, Domínguez A, Tapia JL. Red neonatal neocosur. Survival and morbidity of very low birth weight infant in a South American neonatal network. Arch Argent Pediatr. 2014;112:405–12.
Jain D, Bancalari E. Bronchopulmonary dysplasia: a clinical perspective. Brith Defects Res. 2014;100:134–44.
Gagliardi L, Rusconi F, Bellu R, Zanini R. Association of maternal hypertension and chorioamnionitis with preterm outcomes. Pediatrics. 2014;134:e154–e161.
Gagliardi L, Bellu R, Lista G, Zanini R. Do differences in delivery room intubation explain different rates of bronchopulmonary dysplasia between hospitals? Arch Dis Child Fetal Neonatal Ed. 2011;96:F30–F35.
Trembath A, Laughon MM. Predictors of bronchopulmonary dysplasia. Clin Perinatol. 2012;39:585–601.
Davidson L, Berkelhamer S. Bronchopulmonary dysplasia: chronic lung disease of infancy and long-term pulmonary outcomes. J Clin Med. 2017;6:4. https://doi.org/10.3390/jcm6010004.
Brener Dik PH, Niño Gualdron YM, Galletti MF, Cribioli CM, Mariani GL. Bronchopulmonary dysplasia: incidence and risk factors. Arch Argent Pediatr. 2017;115:476–82.
Baraldi E, Filippone M. Chronic lung disease after premature birth. N Engl J Med. 2017;357:1946–55.
Pakvasa MA, Saroha V, Patel RM. Optimizing caffeine use and risk of bronchopulmonary dysplasia in preterm infants: a systematic review, meta-analysis, and application of grading of recommendations assessment, development, and evaluation methodology. Clin Perinatol. 2018;45:273–91.
Yeh TF, Chen CM, Wu SY, Husan Z, Li TC, Hsieh WS, et al. Intratracheal administration of budesonide/surfactant to prevent bronchopulmonary dysplasia. Am J Respir Critic Care Med. 2016;193:86–95.
O’Reilly M, Thébaud B. The promise of stem cells in bronchopulmonary dysplasia. Semin Perinatol. 2013;37:79–84.
Bührer HS, Avoiding Endotraqueal C. Ventilation to prevent bronchopulmonary dysplasia: a meta-analysis. Pediatrics. 2013;132:e1351–e1360.
Core Team R. R: a language and environment for statistical computing. Vienna, Austria: R Foundation for Statistical Computing; 2018. https://www.R-project.org/.
Fenton TR, Kim JH. A systematic review and meta-analysis to revise the Fenton growth chart for preterm infants. BMC Pediatr. 2013;13:59.
Sahni R, Ammari A, Suri MS, Milisavljevic V, Ohira-Kist K, Wung JT, Polin R. Is the new definition of bronchopulmonary dysplasia more useful? J Perinatol. 2005;25:41–46.
Laughon MM, Langer JC, Bose CL, Smith PB, Ambalavanan N, Kennedy KA, et al. Prediction of bronchopulmonary dysplasia by postnatal age in extremely premature infants. Am J Respir Critic Care Med. 2011;183:1715–22.
Kim YD, Kim AE, Kim KS, Pi SY, Kang W. Scoring method for early prediction of neonatal chronic lung disease using modified respiratory parameters. J Korean Med Sci. 2005;20:397–401.
Bhering CA, Mochdece CC, Moreira ME, Rocco JR, Sant’Anna GM. Bronchopulmonary dysplasia prediction model for 7-day-old infants. J Pediatr. 2007;83:164–70.
Van Marter LJ, Allred EN, Pagano M, Sanocka U, Parad R, Moore M, et al. Do clinical markers of barotrauma and oxygen toxicity explain interhospital variation in rates of chronic lung disease? The Neonatology Committee for the Developmental Network. Pediatrics. 2000;105:1194–201.
Finer NN, Carlo WA, Walsh MC, Rich W, Gantz MG, Laptook AR, et al. Early CPAP versus surfactant in extremely preterm infants. N Engl J Med. 2010;362:1970–9.
Morley CJ, Davis PG, Doyle LW, Brion LP, Hascoet JM, Carlin JB. Nasal CPAP or intubation at birth for very preterm infants. N Engl J Med. 2008;358:700–8.
Foglia E, Jensen E, Kirpalani BM. State of the Art review: delivery room interventions to prevent bronchopulmonary dysplasia in extremely preterm infants. J Perinatol. 2017;371:171–117.
Poets CF, Lorenz L. Prevention of bronchopulmonary dysplasia in extremely low gestational age neonates: current evidence. Arch Dis Child Fetal Neonatal Ed. 2018;0:F1–F7.
Weiner G and Zaichkin J. Textbook of neonatal resuscitation, 7th ed. United States: American Academy of Pediatrics and American Heart Association. 2016.
Roberts D, Brown J, Medley N, Dalziel SR. Antenatal corticosteroids for accelerating fetal lung maturation for women at risk of preterm birth. Cochrane Database Syst Rev. 2017;3:CD004454 https://doi.org/10.1002/14651858.CD004454.pub3.
Gagliardi L, Bellù R, Rusconi F, Merazzi D, Mosca F, Network Neonatale Lombardo Study Group. ANS and risk of BPD: a lack of effect or a case of over-adjustment? Paediatr Perinat Epidemiol. 2007;21:347–53.
Wai K, Kohn MA, Ballard RA, Truog WE, Black DM, Asselin JM, et al. Early cumulative Supplemental oxygen predicts bronchopulmonary dysplasia in high risk extremely low gestational age newborns. J Pediatr. 2016;177:97–102.
Cuna A, LIu C, Govindarajan S, Queen M, Dai H, Truog W. Usefulness of an online risk estimator for bronchopulmonary dysplasia in predicting corticosteroid treatment in infants born preterm. J Pediatr. 2018;197:23–28.e2.
Ballard AR, Mallett LH, Pruszynki JE, Cantey JB. Chorioamnionitis and subsequent bronchopulmonary dysplasia in very-low-birth weight infants: a 25-year cohort. J Perinatol. 2016;36:1045–8.
Kubicka Z, Zahr E, Rousseau T, Feldman HA, Fiascone J. Quality improvement to reduce chronic lung disease rates in very low birth weight infants: high compliance with a respiratory care bundle in a small NICU. J Perinatol. 2018;38:285–92.
Nelin L, Bhandari V. How to decrease bronchopulmonary dysplasia in intensive care unit today and “tomorrow”. F1000. Research. 2017;6:539.
Acknowledgements
We are grateful to Dr Eduardo Bancalari for his critical review of this paper. We thank all the Neocosur centers that participated in this study.
Members from the NEOCOSUR Network: Argentina
Ana Pedraza, Guillermo Colantonio, Gaston Perez, Jorge Zapata, Fortunato Tomas (Clinica y Maternidad Suizo Argentina, Buenos Aires); Carlos Fustiñana, Silvia Fernandez, Gonzalo Mariani, Maria Paola Carrascal, Fernanda Galleti (Hospital Italiano de Buenos Aires); Jorge Tavosnaska, Liliana Roldan, Gladys Saa, Debora Sabatelli, María Laura Gendra, Maria Teresa Sepulveda, Maria Fernanda Buraschi, Graciela Basso (Hospital Juan Fernandez, Buenos Aires); Monica Rinaldi, Daniel Agost (Hospital Lagomaggiore, Mendoza); Claudio Solana, Elio Rojas, Ricardo Nieto, Javier Meritano (Maternidad Sarda, Buenos Aires); Nestor Vain, Lionel Cracco, Edith Martínez, Noemi Jacobi, María San Miguel (Sanatorio de la Trinidad, Buenos Aires). Chile: Paulina Toso, Daniela Masoli, Jorge Fabres, Alberto Estay, Jose L. Tapia, Alvaro Gonzalez, Mariela Quezada, Solange Rojas (Hospital Clinico Universidad Católica de Chile, Santiago); Jaime Burgos, Maria Eugenia Hübner, Rodrigo Ramirez (Hospital Clinico Universidad de Chile, Santiago); Jorge Leon del Pedregal, Lilia Campos, Aldo Bancalari, Ximena Giaconi, Sergio Treuer (Hospital Guillermo Grant, Concepcion); Jane Standen, Marisol Escobar, Daniela Sandino, Viviana Veas (Hospital Gustavo Fricke, Viña del Mar); Agustina Gonzalez, Claudia Avila (Hospital San Jose, Santiago); Marcela Díaz, Patricia Mena (Hospital Dr. Sotero del Rio, Santiago). Paraguay: Ramon Mir, Jose Lacarruba, Larissa Genes, Elizabeth Cespedes, Elvira Mendieta (Departamento de Hospital de Clinicas de Asunción, Asuncion). Perú: Veronica Webb, Margarita Llontop, Lili Chancafe, Sicilia Bellomo (Hospital Cayetano Heredia, Lima). Uruguay: Beatriz Ceruti, Daniel Borbonet, Sandra Gugliucci, Andrea Lanza, Florencia Rodrigo, Ricardo Tambasco, Micaela Murillo (Facultad de Medicina Servicio de Recién Nacidos Pereyra Rossell, Montevideo). Unidad Base de Datos: Pontificia Universidad Catolica (PUC), Santiago: Ivonne D’Apremont, Jose L Tapia, Mariela Quezada, Solange Rojas, Luis Villarroel, Angelica Dominguez, Guillermo Marshall. Gerencia Informatica PUC.
Funding
There was no external funding for this work.
Author information
Authors and Affiliations
Consortia
Contributions
All authors conceived the idea, analyzed the results, and contributed to the final paper. Dr Marshall performed the statistical analysis.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher’s note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Valenzuela-Stutman, D., Marshall, G., Tapia, J.L. et al. Bronchopulmonary dysplasia: risk prediction models for very-low- birth-weight infants. J Perinatol 39, 1275–1281 (2019). https://doi.org/10.1038/s41372-019-0430-x
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41372-019-0430-x
This article is cited by
-
Transforming neonatal care with artificial intelligence: challenges, ethical consideration, and opportunities
Journal of Perinatology (2024)
-
Bronchopulmonary dysplasia prediction models: a systematic review and meta-analysis with validation
Pediatric Research (2023)
-
Risk factors and machine learning prediction models for bronchopulmonary dysplasia severity in the Chinese population
World Journal of Pediatrics (2023)
-
Development of a new scoring method in the neurofunctional assessment of preterm infants
Scientific Reports (2022)
-
Lung ultrasound predicts the development of bronchopulmonary dysplasia: a prospective observational diagnostic accuracy study
European Journal of Pediatrics (2021)