Abstract
Objective
To evaluate the relationship between systolic (SBP), diastolic (DBP), mean (MBP) blood pressures and pulse pressure (PP), and left ventricular output (LVO), a surrogate of systemic blood flow.
Study design
This retrospective study included neonates who underwent targeted neonatal echocardiography (TNE) in 3-tertiary NICUs over 2 years. Associations between LVO and BP components were investigated. Analysis was adjusted for relevant covariates.
Result
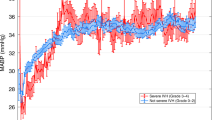
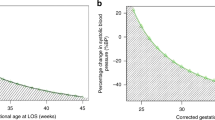
1060 studies from 485 neonates were included, with a mean GA of 28.4 ± 4.6 weeks and birth weight of 1234 ± 840 grams. LVO was associated positively with SBP and PP, and negatively with GA. PP demonstrated the highest predictive value for identifying infants with LVO < 150 ml/kg/min (area under the curve 0.75 [95% CI 0.68, 0.82]). MBP and DBP demonstrated no correlation with LVO.
Conclusion
BP parameters correlate poorly with LVO, irrespective of GA and underlying etiology. Narrow PP may be more reflective of low LVO than low SBP.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout

Similar content being viewed by others
References
De Boode W-P. Clinical monitoring of systemic hemodynamics in critically ill newborns. Early Hum Dev. 2010;86:137–41.
Ficial B, Finnemore AE, Cox DJ, Broadhouse KM, Price AN, Durighel G, et al. Validation study of the accuracy of echocardiographic measurements of systemic blood flow volume in newborn infants. J Am Soc Echocardiogr. 2013;26:1365–71.
Kluckow M. Low systemic blood flow and pathophysiology of the preterm transitional circulation. Early Hum Dev. 2005;81:429–37.
Cordero L, Timan C, Waters H, Sachs L. Mean arterial pressures during the first 24h of life in or =600-gram birth weight infants. J Perinatol. 2002;22:348–53.
Demarini S, Dollberg S, Hoath S, Ho M, Donovan E. Effects of antenatal corticosteroids on blood pressure in very low birth weight infants during the first 24h of life. J Perinatol. 1999;19:419–25.
Wu T-W, Azhibekov T, Seri I. Transitional hemodynamics in preterm neonates: clinical relevance. Pediatr Neonatol. 2016;57:7–18.
Laptook A, Jackson GL. Cold stress and hypoglycemia in the late preterm (“Near-Term”) infant: impact on nursery of admission. Semin Perinatol Elsevier. 2006;30:24–7.
Jain A, El-Khuffash AF, Kuipers BC, Connelly KA, McNamara PJ, Jankov RP, et al. Left ventricular function in healthy term neonates during the transitional period. J Pediatr. 2017;182:197–203.
Gill A, Weindling A. Echocardiographic assessment of cardiac function in shocked very low birthweight infants. Arch Dis Child. 1993;68:17–21.
Initiative NNN. Systolic blood pressure in babies of less than 32 weeks gestation in the first year of life. Northern Neonatal Nursing Initiative. Arch Dis Child Fetal Neonatal Ed.1999;80:F38–42.
Osborn D, Evans N, Kluckow M. Clinical detection of low upper body blood flow in very premature infants using blood pressure, capillary refill time, and central-peripheral temperature difference. Arch Dis Child Fetal Neonatal Ed. 2004;89:F168–73.
Groves aM, Kuschel Ca, Knight DB, Skinner JR. Relationship between blood pressure and blood flow in newborn preterm infants. Arch Dis Child Fetal Neonatal Ed [Internet]. 2008;93:F29–32. http://www.ncbi.nlm.nih.gov/pubmed/17475696
Fanaroff AA, Fanaroff JM. Short- and long-term consequences of hypotension in ELBW. Semin Perinatol. 2006;30:151–5.
Batton B, Li L, Newman N, Das A, Watterberg K, Yoder B, et al. Use of antihypotensive therapies in extremely preterm infants. Pediatrics. 2013;131:e1865–73.
Dempsey EM, Barrington KJ. Treating hypotension in the preterm infant: when and with what: a critical and systematic review. J Perinatol Nat Publ Group. 2007;27:469.
Rourke MO. Arterial stiffness, systolic blood pressure, and logical treatment of arterial hypertension. Hypertension. 1990;15:339–47.
Lyu Y, Xiang YY, Isayama T, Alvaro R, Nwaesei C, Barrington K, et al. Admission systolic blood pressure and outcomes in preterm infants of ≤26 weeks’ gestation. Am J Perinatol Thieme Med Publ. 2017;34:1271–8.
Costanzo LS. Physiology. 6th edn. pp 163–166 (Elsevier, Philadelphia, PA 2018).
Miall-Allen VM, De Vries LS, Whitelaw AG. Mean arterial blood pressure and neonatal cerebral lesions. Arch Dis Child. 1987;62:1068–9.
Mellander M, Sabel K, Caidahl K, Solymar L, Eriksson B. Doppler determination of cardiac output in infants and children: comparison with simultaneous thermodilution. Pediatr Cardiol. 1987;8:241–6.
Alverson D, Eldridge M, Johnson I, Aldrich M, Angelus P, Berman W. Noninvasive measurement of cardiac output in healthy preterm and term newborn infants. Am J Perinatol. 1984;1:148–51.
Acknowledgements
The authors would like to acknowledge Dr. Kin Fan Young Tai, staff neonatologist at Mount Sinai Hospital, for her intellectual contribution to the study analysis.
Funding
The authors have no relevant financial relationships to disclose.
Author contribution
Drs. Kharrat and Jain conceptualized and designed the study, designed the data collection instruments, carried out the data extraction, drafted the initial manuscript, and approved the final manuscript as submitted. Dr. Ibarra Rios reviewed the study protocol and contributed to its design, carried out data extraction, reviewed and revised the manuscript, and approved the final manuscript as submitted. Drs. Weisz, Giesinger, Groves, and McNamara reviewed the study protocol and contributed to its design, critically reviewed and revised the manuscript, and approved the final manuscript as submitted. Mr. Yang reviewed the study protocol and contributed to its design, performed the statistical analysis, and approved the final manuscript as submitted. Dr. Shah critically reviewed the study protocol and contributed to its design, reviewed the extracted data and statistical analysis, critically reviewed and revised the manuscript, and approved the final manuscript as submitted.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher’s note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Kharrat, A., Rios, D.I., Weisz, D.E. et al. The Relationship between blood pressure parameters and left ventricular output in neonates. J Perinatol 39, 619–625 (2019). https://doi.org/10.1038/s41372-019-0337-6
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41372-019-0337-6
This article is cited by
-
Hemodynamic evaluation in preterm infants using ultrasonic cardiac output monitor (USCOM)
European Journal of Pediatrics (2024)
-
Arterial pressure is not reflective of right ventricular function in neonates with hypoxic ischemic encephalopathy treated with therapeutic hypothermia
Journal of Perinatology (2023)
-
Hemodynamic dysfunction in neonatal sepsis
Pediatric Research (2022)
-
Blood pressure, organ dysfunction, and mortality in preterm neonates with late-onset sepsis
Pediatric Research (2022)
-
Fluid-Structure Interaction Model for Predicting Surgical Result of Total Anomalous Pulmonary Venous Connection and Estimating Pulmonary Venous Properties
Cardiovascular Engineering and Technology (2022)