Abstract
Objective
To evaluate the association between early (within 10 d) pRBC transfusion and the development of severe ROP.
Study design and Methods
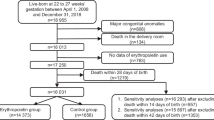
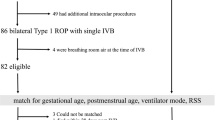
This was a single-center retrospective study. Inclusion criteria were preterm infants born ≤32 weeks gestation or weighing ≤1500 g. Severe ROP was defined as infants requiring retinal laser ablation or bevacizumab injection. Logistic regression was used to identify the association between transfusions and severe ROP.
Results
A total of 1635 infants were included in the final analysis. The severe ROP incidence was 8% (126/1635). Ninety-one percent (115/126) of infants who developed severe ROP received a pRBC transfusion in the first 10 d. Early transfusion was associated with severe ROP; adjusted odds ratio of 3.8 (95% CI: 1.8−8.1).
Conclusion
pRBC transfusions in the first 10 days of life are associated with an almost four-fold increased risk of severe ROP, independent of gestational age at birth or bronchopulmonary dysplasia (BPD) status.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout


Similar content being viewed by others
References
Chen J, Smith LE. Retinopathy of prematurity. Angiogenesis. 2007;10:133–40.
Sears JE, Pietz J, Sonnie C, Dolcini D, Hoppe G. A change in oxygen supplementation can decrease the incidence of retinopathy of prematurity. Ophthalmology. 2009;116:513–8.
Saugstad OD, Sejersted Y, Solberg R, Wollen EJ, Bjoras M. Oxygenation of the newborn: a molecular approach. Neonatology. 2012;101:315–25.
Lucey JF, Dangman B. A reexamination of the role of oxygen in retrolental fibroplasia. Pediatrics. 1984;73:82–96.
Gunn TR, Easdown J, Outerbridge EW, Aranda JV. Risk factors in retrolental fibroplasia. Pediatrics. 1980;65:1096–100.
Sacks LM, Schaffer DB, Anday EK, Peckham GJ, Delivoria-Papadopoulos M. Retrolental fibroplasia and blood transfusion in very low-birth-weight infants. Pediatrics. 1981;68:770–4.
Shohat M, Reisner SH, Krikler R, Nissenkorn I, Yassur Y, Ben-Sira I. Retinopathy of prematurity: incidence and risk factors. Pediatrics. 1983;72:159–63.
Seiberth V, Linderkamp O. Risk factors in retinopathy of prematurity. a multivariate statistical analysis. Ophthalmologica. 2000;214:131–5.
Slidsborg C, Jensen A, Forman JL, Rasmussen S, Bangsgaard R, Fledelius HC, et al. Neonatal Risk Factors for Treatment-Demanding Retinopathy of Prematurity: A Danish National Study. Ophthalmology. 2016;123:796–803.
Good WV. Early Treatment for Retinopathy of Prematurity Cooperative G. Final results of the Early Treatment for Retinopathy of Prematurity (ETROP) randomized trial. Trans Am Ophthalmol Soc. 2004;102:233–48. discussion48-50
Shennan AT, Dunn MS, Ohlsson A, Lennox K, Hoskins EM. Abnormal pulmonary outcomes in premature infants: prediction from oxygen requirement in the neonatal period. Pediatrics. 1988;82:527–32.
Bell MJ, Ternberg JL, Feigin RD, Keating JP, Marshall R, Barton L, et al. Neonatal necrotizing enterocolitis. Therapeutic decisions based upon clinical staging. Ann Surg. 1978;187:1–7.
Fierson WM. American Academy of Pediatrics Section on O, American Academy of O, American Association for Pediatric O, Strabismus, American Association of Certified O. Screening examination of premature infants for retinopathy of prematurity. Pediatrics. 2013;131:189–95.
International Committee for the Classification of Retinopathy of P.. The International Classification of Retinopathy of Prematurity revisited. Arch Ophthalmol. 2005;123:991–9.
Akkoyun I, Oto S, Yilmaz G, Gurakan B, Tarcan A, Anuk D, et al. Risk factors in the development of mild and severe retinopathy of prematurity. J AAPOS. 2006;10:449–53.
Dani C, Reali MF, Bertini G, Martelli E, Pezzati M, Rubaltelli FF. The role of blood transfusions and iron intake on retinopathy of prematurity. Early Hum Dev. 2001;62:57–63.
Brooks SE, Marcus DM, Gillis D, Pirie E, Johnson MH, Bhatia J. The effect of blood transfusion protocol on retinopathy of prematurity: A prospective, randomized study. Pediatrics. 1999;104(3 Pt 1):514–8.
Kirpalani H, Whyte RK, Andersen C, Asztalos EV, Heddle N, Blajchman MA, et al. The Premature Infants in Need of Transfusion (PINT) study: a randomized, controlled trial of a restrictive (low) versus liberal (high) transfusion threshold for extremely low birth weight infants. J Pediatr. 2006;149:301–7.
Bell EF, Strauss RG, Widness JA, Mahoney LT, Mock DM, Seward VJ, et al. Randomized trial of liberal versus restrictive guidelines for red blood cell transfusion in preterm infants. Pediatrics. 2005;115:1685–91.
Stutchfield CJ, Jain A, Odd D, Williams C, Markham R. Foetal haemoglobin, blood transfusion, and retinopathy of prematurity in very preterm infants: a pilot prospective cohort study. Eye (Lond). 2017;31:1451–5.
De Halleux V, Truttmann A, Gagnon C, Bard H. The effect of blood transfusion on the hemoglobin oxygen dissociation curve of very early preterm infants during the first week of life. Semin Perinatol. 2002;26:411–5.
Venancio JP, Santos AM, Guinsburg R, Peres Cde A, Shinzato AR, Lora MI. Strict guideline reduces the need for RBC transfusions in premature infants. J Trop Pediatr. 2007;53:78–82.
Widness JA, Madan A, Grindeanu LA, Zimmerman MB, Wong DK, Stevenson DK. Reduction in red blood cell transfusions among preterm infants: results of a randomized trial with an in-line blood gas and chemistry monitor. Pediatrics. 2005;115:1299–306.
Gill AB, Weindling AM. Randomised controlled trial of plasma protein fraction versus dopamine in hypotensive very low birthweight infants. Arch Dis Child. 1993;69:284–7. 3 Spec No
Jeschke MG, Chinkes DL, Finnerty CC, Przkora R, Pereira CT, Herndon DN. Blood transfusions are associated with increased risk for development of sepsis in severely burned pediatric patients. Crit Care Med. 2007;35:579–83.
Lacroix J, Hebert PC, Hutchison JS, Hume HA, Tucci M, Ducruet T, et al. Transfusion strategies for patients in pediatric intensive care units. N Engl J Med. 2007;356:1609–19.
Wyckoff MH, Aziz K, Escobedo MB, Kapadia VS, Kattwinkel J, Perlman JM, et al. Part 13: Neonatal Resuscitation: 2015 American Heart Association Guidelines Update for Cardiopulmonary Resuscitation and Emergency Cardiovascular Care (Reprint). Pediatrics. 2015;136(Suppl 2):S196–218.
Wyckoff MH, Perlman JM, Laptook AR. Use of volume expansion during delivery room resuscitation in near-term and term infants. Pediatrics. 2005;115:950–5.
Patel RM, Knezevic A, Shenvi N, Hinkes M, Keene S, Roback JD, et al. Association of Red Blood Cell Transfusion, Anemia, and Necrotizing Enterocolitis in Very Low-Birth-Weight Infants. JAMA. 2016;315:889–97.
Girelli G, Antoncecchi S, Casadei AM, Del Vecchio A, Isernia P, Motta M, et al. Recommendations for transfusion therapy in neonatology. Blood Transfus. 2015;13:484–97.
Wang D, Sun J, Solomon SB, Klein HG, Natanson C. Transfusion of older stored blood and risk of death: a meta-analysis. Transfusion. 2012;52:1184–95.
Funding source
This work was supported by the following grants: 1. Washington University Institute of Clinical and Translational Sciences KL2 Training Program (NIH/NCATS KL2 TR000450 [to ZV]). 2. The Barnes-Jewish Hospital Foundation and the Washington University Institute of Clinical and Translational Sciences Clinical and Translational Funding Program (NIH/NCATS UL1 TR000448). 3. Washington University in St. Louis Center for Biomedical Informatics, Clinical Investigation Data Exploration Repository (NIH/NCATS UL1 TR000448).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Rights and permissions
About this article
Cite this article
Lust, C., Vesoulis, Z., Jackups, R. et al. Early red cell transfusion is associated with development of severe retinopathy of prematurity. J Perinatol 39, 393–400 (2019). https://doi.org/10.1038/s41372-018-0274-9
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41372-018-0274-9
This article is cited by
-
Retrospective cohort study of neonatal blood transfusion in China
BMC Pediatrics (2023)
-
Can cord blood sampling delay the first packed red blood cell transfusion?
Journal of Perinatology (2021)
-
Anemia of prematurity: how low is too low?
Journal of Perinatology (2021)
-
Predictors and ocular outcomes of rescue treatment in preterm infants with treated retinopathy of prematurity—a retrospective study
Eye (2021)
-
Effects of blood sampling stewardship and erythropoietin administration in extremely low birth weight infants—a quality improvement non-controlled before-and-after retrospective study
European Journal of Pediatrics (2021)