Abstract
Objective:
To characterize clinical outcomes of infants born after previable rupture of membranes (pROM, < 23 weeks gestation and latency period ≥ 2 weeks) in relation to refractory hypoxic respiratory failure (rHRF).
Study Design:
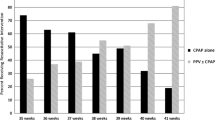
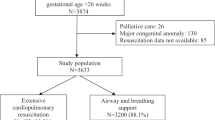
pROM neonates categorized as rHRF (FiO2 > 0.6 for ≥ 2 h) and treated (high frequency ventilation + inhaled nitric oxide) were compared with no rHRF group. Primary outcome was survival until discharge. Factors associated with rHRF and mortality were identified.
Result:
Overall, mortality and disability rates were 28% and 22%, respectively. Treated rHRF group (n = 32) had longer period of ROM, mortality was (31% vs. 14%; p = 0.20), with similar survival-without-disability (54% vs. 47%; p = 0.67). Higher gestational age at birth [1.57 (1.03,2.39)] and cesarean delivery [12.6 (1.22,125)] were associated with increased survival.
Conclusion:
Birth after pROM is associated with high rates of adverse outcomes, independent of latency period. Following treatment, rHRF infants may have similar long-term outcomes as those without rHRF.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout

Similar content being viewed by others
References
Dewan H, Morris JM. A systematic review of pregnancy outcome following preterm premature rupture of membranes at a previable gestational age. Aust N Z J Obstet Gynaecol. 2001;41:389–94.
Waters TP, Mercer BM. The management of preterm premature rupture of the membranes near the limit of fetal viability. Am J Obstet Gynecol. 2009;201:230–40.
Geary C, Whitsett J. Inhaled nitric oxide for oligohydramnios-induced pulmonary hypoplasia: a report of two cases and review of the literature. J Perinatol. 2002;22:82–5.
Williams O, Hutchings G, Debieve F, Debauche C. Contemporary neonatal outcome following rupture of membranes prior to 25 weeks with prolonged oligohydramnios. Early Hum Dev. 2009;85:273–7.
Williams O, Hutchings G, Hubinont C, Debauche C, Greenough A. Pulmonary effects of prolonged oligohydramnios following mid-trimester rupture of the membranes--antenatal and postnatal management. Neonatology. 2012;101:83–90.
de Waal K, Kluckow M. Prolonged rupture of membranes and pulmonary hypoplasia in very preterm infants: pathophysiology and guided treatment. J Pediatr. 2015;166:1113–20.
Shah DM, Kluckow M. Early functional echocardiogram and inhaled nitric oxide: usefulness in managing neonates born following extreme preterm premature rupture of membranes (PPROM). J Paediatr Child Health. 2011;47:340–5.
Lindner W, Pohlandt F, Grab D, Flock F. Acute respiratory failure and short-term outcome after premature rupture of the membranes and oligohydramnios before 20 weeks of gestation. J Pediatr. 2002;140:177–82.
Everest NJ, Jacobs SE, Davis PG, Begg L, Rogerson S. Outcomes following prolonged preterm premature rupture of the membranes. Arch Dis Child Fetal Neonatal Ed. 2008;93:F207–11.
Kibel M, Asztalos E, Barrett J, Dunn MS, Tward C, Pittini A, et al. Outcomes of pregnancies complicated by preterm premature rupture of membranes between 20 and 24 weeks of gestation. Obstet Gynecol. 2016;128:313–20.
Lee JY, Ahn TG, Jun JK. Short-term and long-term postnatal outcomes of expectant management after previable preterm premature rupture of membranes with and without persistent oligohydramnios. Obstet Gynecol. 2015;126:947–53.
Acaia B, Crovetto F, Ossola MW, Nozza S, Baffero GM, Somigliana E, et al. Predictive factors for neonatal survival in women with periviable preterm rupture of the membranes. J Matern Fetal Neonatal Med. 2013;26:1628–34.
Walker MW, Picklesimer AH, Clark RH, Spitzer AR, Garite TJ. Impact of duration of rupture of membranes on outcomes of premature infants. J Perinatol. 2014;34:669–72.
Williams O, Michel B, Hutchings G, Debauche C, Hubinont C. Two-year neonatal outcome following PPROM prior to 25 weeks with a prolonged period of oligohydramnios. Early Hum Dev. 2012;88:657–61.
Park GY, Park WS, Yoo HS, Ahn SY, Sung SI, Kim SS, et al. Short-term outcomes comparison between preterm infants with and without acute hypoxic respiratory failure attributable to presumed pulmonary hypoplasia after prolonged preterm premature rupture of membranes before 25 gestational weeks. J Matern Fetal Neonatal Med. 2018;31:1–8.
Blott M, Greenough A. Neonatal outcome after prolonged rupture of the membranes starting in the second trimester. Arch Dis Child. 1988;63:1146–50. 10Spec No
Winn HN, Chen M, Amon E, Leet TL, Shumway JB, Mostello D. Neonatal pulmonary hypoplasia and perinatal mortality in patients with midtrimester rupture of amniotic membranes--a critical analysis. Am J Obstet Gynecol. 2000;182:1638–44.
Grisaru-Granovsky S, Eitan R, Kaplan M, Samueloff A. Expectant management of midtrimester premature rupture of membranes: a plea for limits. J Perinatol. 2003;23:235–9.
Aikio O, Metsola J, Vuolteenaho R, Perhomaa M, Hallman M. Transient defect in nitric oxide generation after rupture of fetal membranes and responsiveness to inhaled nitric oxide in very preterm infants with hypoxic respiratory failure. J Pediatr. 2012;161:397–403 e1.
Chock VY, Van Meurs KP, Hintz SR, Ehrenkranz RA, Lemons JA, Kendrick DE, et al. Inhaled nitric oxide for preterm premature rupture of membranes, oligohydramnios, and pulmonary hypoplasia. Am J Perinatol. 2009;26:317–22.
The Canadian Congenital Diaphragmatic Hernia Collaborative. Diagnosis and management of congenital diaphragmatic hernia: a clinical practice guideline. CMAJ. 2018;190:E103–E112.
Alfirevic Z, Milan SJ, Livio S Caesarean section versus vaginal delivery for preterm birth in singletons. Cochrane Database Syst Rev. 2012:CD000078.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Rights and permissions
About this article
Cite this article
Baczynski, M., Ginty, S., Weisz, D. et al. Outcomes of hypoxic respiratory failure at birth associated with previable rupture of membranes. J Perinatol 38, 1087–1092 (2018). https://doi.org/10.1038/s41372-018-0131-x
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41372-018-0131-x
This article is cited by
-
Clinical burden associated with therapies for cardio-pulmonary critical decompensation in preterm neonates across Canadian neonatal intensive care units
European Journal of Pediatrics (2022)