Abstract
Objective
Preterm infants are at higher risk of developing hypothermia and complications from cold stress, resulting in high mortality and short-term morbidity. Our objective is to evaluate the association between admission temperatures of extremely low-gestational age neonates (ELGAN) (<29 weeks’) and adverse short-term neurodevelopmental outcomes.
Study design
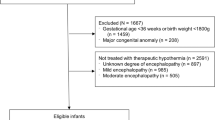
In this retrospective study, we included ELGAN admitted to NICUs across Canada between April 2009 and September 2011, who underwent neurodevelopmental assessment at 18–21 months’ corrected age.
Results
Of 2739 infants with a complete data set identified during the study period, 968 (35.3%) had admission temperatures ≤36.4 °C (hypothermia group), 1489 (54.5%) had temperature of 36.5–37.2 °C (normothermia group), and 282 (10.3%) had hyperthermia (≥37.3 °C). Their mean birth weight was 823 ± 230 g, 944 ± 227 g and 927 ± 223 g, respectively (p < 0.01). More than 50% of infants born at 23–24 weeks were in the hypothermic group compared to 28.5–36.1% at higher gestational ages. We found 39.5% of infants in the hypothermic group had primary composite outcome of death or severe neurodevelopmental impairment (sNDI). Multivariate logistic regression revealed an increased adjusted odd of primary composite outcome (OR = 1.32; 95% CI = [1.05, 1.66]) in the hypothermic group, compared to infants with normothermia on admission.
Conclusions
In our cohort of ELGAN, hypothermia on admission was associated with increased risk of death or sNDI.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout

Similar content being viewed by others
References
Wilson E, Maier RF, Norman M, Misselwitz B, Howell EA, Zeitlin J, et al. Admission hypothermia in very preterm infants and neonatal mortality and morbidity. J Pediatr. 2016;175:61–7, e64.
Miller SS, Lee HC, Gould JB. Hypothermia in very low birth weight infants: distribution, risk factors and outcomes. J Perinatol. 2011;31(Suppl 1):S49–56.
Lyu Y, Shah PS, Ye XY, Warre R, Piedboeuf B, Deshpandey A, et al. Association between admission temperature and mortality and major morbidity in preterm infants born at fewer than 33 weeks’ gestation. JAMA Pediatr. 2015;169:e150277.
Synnes A, Luu TM, Moddemann D, Church P, Lee D, Vincer M, et al. Determinants of developmental outcomes in a very preterm Canadian cohort. Arch Dis Child Fetal Neonatal Ed. 2017;102:F235–F243.
Canadian Neonatal Follow-Up Network. 18‐Month corrected age assessment manual (Version 5). http://www.cnfun.ca/LinkClick.aspx?fileticket=d4p7mZoXWDU%3d&tabid=68. Accessed 4 November, 2016.
Canadian Neonatal Network. Abstractor’s manual. http://www.canadianneonatalnetwork.org/Portal/LinkClick.aspx?fileticket=U4anCYsSN20%3D&tabid=69.Accessed4 November, 2016.
Shah PS, Seidlitz W, Chan P, Yeh S, Musrap N, Lee SK, et al. Internal audit of the Canadian Neonatal Network data collection system. Am J Perinatol. 2017;34:1241–9.
Kramer MS, Platt RW, Wen SW, Joseph KS, Allen A, Abrahamowicz M, et al. A new and improved population-based Canadian reference for birth weight for gestational age. Pediatrics. 2001;108:E35.
Bell MJ, Ternberg JL, Feigin RD, Keating JP, Marshall R, Barton L, et al. Neonatal necrotizing enterocolitis. Therapeutic decisions based upon clinical staging. Ann Surg. 1978;187:1–7.
Neu J, Walker WA. Necrotizing enterocolitis. N Engl J Med. 2011;364:255–64.
Baraldi E, Filippone M. Chronic lung disease after premature birth. N Engl J Med. 2007;357:1946–55.
Jasani B, Nanavati R, Kabra N. Mechanisms and management of retinopathy of prematurity. N Engl J Med. 2013;368:1161–2.
Papile LA, Burstein J, Burstein R, Koffler H. Incidence and evolution of subependymal and intraventricular hemorrhage: a study of infants with birth weights less than 1,500 gm. J Pediatr. 1978;92:529–34.
Rosenbaum P, Paneth N, Leviton A, Goldstein M, Bax M, Damiano D, et al. A report: the definition and classification of cerebral palsy April 2006. Dev Med Child Neurol Suppl. 2007;109:8–14.
Laptook AR, Watkinson M. Temperature management in the delivery room. Semin Fetal Neonatal Med. 2008;13:383–91.
Laptook AR, Salhab W, Bhaskar B, Neonatal Research Network. Admission temperature of low birth weight infants: predictors and associated morbidities. Pediatrics. 2007;119:e643–9.
Costeloe K, Hennessy E, Gibson AT, Marlow N, Wilkinson AR. The EPICure study: outcomes to discharge from hospital for infants born at the threshold of viability. Pediatrics. 2000;106:659–71.
Yu VY, Joseph R, Bajuk B, Orgill A, Astbury J. Perinatal risk factors for necrotizing enterocolitis. Arch Dis Child. 1984;59:430–4.
Weiner G. Textbook of Neonatal Resuscitation, 7th edn. American Academy of Pediatrics and American Heart Association. 2016. American Academy of Pediatrics: Itasca, Illinois, United States
Lee HC, Ho QT, Rhine WD. A quality improvement project to improve admission temperatures in very low birth weight infants. J Perinatol. 2008;28:754–8.
Vento M, Cheung PY, Aguar M. The first golden minutes of the extremely-low-gestational-age neonate: a gentle approach. Neonatology. 2009;95:286–98.
Vohra S, Frent G, Campbell V, Abbott M, Whyte R. Effect of polyethylene occlusive skin wrapping on heat loss in very low birth weight infants at delivery: a randomized trial. J Pediatr. 1999;134:547–51.
Singh A, Duckett J, Newton T, Watkinson M. Improving neonatal unit admission temperatures in preterm babies: exothermic mattresses, polythene bags or a traditional approach? J Perinatol. 2010;30:45–9.
McCarthy LK, O’Donnell CP. Warming preterm infants in the delivery room: polyethylene bags, exothermic mattresses or both? Acta Paediatr. 2011;100:1534–7.
Trevisanuto D, Doglioni N, Cavallin F, Parotto M, Micaglio M, Zanardo V. Heat loss prevention in very preterm infants in delivery rooms: a prospective, randomized, controlled trial of polyethylene caps. J Pediatr. 2010;156:914–7, e911.
Gandy GM, Adamsons K Jr., Cunningham N, Silverman WA, James LS. Thermal environment and acid-base homeostasis in human infants during the first few hours of life. J Clin Invest. 1964;43:751–8.
Mukerji A, Shah V, Shah PS. Periventricular/intraventricular hemorrhage and neurodevelopmental outcomes: a meta-analysis. Pediatrics. 2015;136:1132–43.
Anderson PJ, Doyle LW. Neurodevelopmental outcome of bronchopulmonary dysplasia. Semin Perinatol. 2006;30:227–32.
Schulzke SM, Deshpande GC, Patole SK. Neurodevelopmental outcomes of very low-birth-weight infants with necrotizing enterocolitis: a systematic review of observational studies. Arch Pediatr Adolesc Med. 2007;161:583–90.
Acknowledgements
We gratefully acknowledge all site investigators and data abstractors of the Canadian Neonatal Network. We also extend our thanks to staff at the Maternal-Infant Care Research Centre at Mount Sinai Hospital, Toronto, ON, for providing organizational, statistical and editorial support for this project. Specifically, we extend our thanks to Junmin Yang, for statistical support.
Funding
Organizational support was provided by the Maternal-Infant Care Research Centre (MiCare) at Mount Sinai Hospital in Toronto, ON, Canada. MiCare is supported by a team grant from the Canadian Institutes of Health Research (CIHR, FRN87518) and in-kind support from Mount Sinai Hospital. Dr Shah holds an Applied Research Chair in Reproductive and Child Health Services and Policy Research awarded by the CIHR (APR-126340). The funding agencies had no role in the design and conduct of the study; collection, analysis and interpretation of the data; the writing of the report; and the decision to submit the manuscript for publication. This work was supported by the Canadian Neonatal Network (CNN) Coordinating Centre, which is based at the Maternal-Infant Care Research Centre (MiCare) at Mount Sinai Hospital in Toronto, Ontario, Canada. The CNN and MiCare are supported by team grant funding from the Canadian Institutes of Health Research (FRN87518, PBN150642). Dr Shah holds an applied research chair in Reproductive and Child Health Services and Policy Research awarded by the Canadian Institutes of Health Research (APR-126340).
Author contributions
The first draft of this manuscript was written by JYT. All authors take responsibility for the reported findings and have participated in the concept and design, analysis and interpretation of data, drafting or revising, and approval of this manuscript as submitted. No honorarium, grant or other form of payment was given to anyone to write the manuscript.
Author information
Authors and Affiliations
Consortia
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Group Information: Investigators of the Canadian Neonatal Network and Canadian Neonatal Follow-Up Network are listed in the online supplement (Appendix; online).
Electronic supplementary material
Rights and permissions
About this article
Cite this article
Ting, J.Y., Synnes, A., Lee, S.K. et al. Association of admission temperature and death or adverse neurodevelopmental outcomes in extremely low-gestational age neonates. J Perinatol 38, 844–849 (2018). https://doi.org/10.1038/s41372-018-0099-6
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41372-018-0099-6
This article is cited by
-
Temperature probe placement in very preterm infants during delivery room stabilization: an open-label randomized trial
Pediatric Research (2024)
-
Medical Management Considerations of Premature Infants with Congenital Heart Disease
Current Treatment Options in Pediatrics (2024)
-
Admission temperature of very low birth weight infants and outcomes at three years old
Scientific Reports (2022)
-
Outcomes of neonatal hypothermia among very low birth weight infants: a Meta-analysis
Maternal Health, Neonatology and Perinatology (2021)
-
Body temperature instability and respiratory morbidity in the very low birth weight infant: a multiple case, intensive longitudinal study
BMC Pediatrics (2020)