Abstract
Objective
We sought to explore the beliefs regarding palliative care team utilization, as well as increase consultation and awareness of the palliative care team’s role in the NICU.
Study design
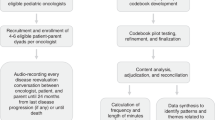
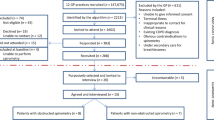
The study design in this Level 4 NICU included observational time series with multiple planned sequential interventions. Medical chart review was conducted to determine eligibility, and statistical process control charts were used to show performance over time.
Results
Prior to implementation of the triggers, 26% received consultation, which increased to 46% after implementation. There was an increase in level of understanding, knowledge of team’s role, and improved utilization. The time until initial consultation decreased from ~1.5 months to 1 week.
Conclusions
We observed a 20% increase in consultations. Key interventions included continual education, reminders, and clear postage of the trigger list. Written guidelines increase awareness of a palliative care team’s role within a NICU, and provider satisfaction.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout

Similar content being viewed by others
References
MacDorman MF, Gregory EC. Fetal and perinatal mortality: United States, 2013. Natl Vital Stat Rep. 2015;64(8):1–24.
American Academy of Pediatrics. Committee on Bioethics and Committee on Hospital Care. Palliative care for children. Pediatrics. 2000;106:351–7.
American Academy of Pediatrics. Section on Hospice and Palliative Medicine and Committee on Hospital Care. Pediatric palliative care and hospice care commitments, guidelines, and recommendations. Pediatrics. 2013; 132(5): 966–2.
Brosig CL, Pierucci RL, Kupst MJ, Leuthner SR. Infant end-of-life care: the parents’ perspective. J Perinatol. 2007;27(8):510–6.
Cortezzo DE, Sanders MR, Brownell E, Moss K. Neonatologists’ perspectives of palliative and end-of-life care in neonatal intensive care units. J Perinatol. 2013;33(9):731–5.
Cortezzo DE, Sanders MR, Brownell EA, Moss K. End-of-life care in the neonatal intensive care unit: experiences of staff and parents. Am J Perinatol. 2015;32(8):713–24.
Keele L, Keenan HT, Sheetz J, Bratton SL. Differences in characteristics of dying children who receive and do not receive palliative care. Pediatr. 2013;132(1):72–8.
Leuthner SR, Pierucci R. Experience with neonatal palliative care consultation at the Medical College of Wisconsin—Children’s Hospital of Wisconsin. J Palliat Med. 2001;4(1):39–47.
Pierucci RL, Kirby RS, Leuthner SR. End-of-life care for neonates and infants: the experience and effects of a palliative care consultation service. Pediatr. 2001;108(3):653–60.
Samsel C, Lechner BE. End-of-life care in a regional level IV neonatal intensive care unit after implementation of a palliative care initiative. J Perinatol. 2015;35(3):223–28.
Younge N, Smith PB, Goldberg RN, Brandon DH, Simmons C, Cotten CM, et al. Impact of a palliative care program on end-of-life care in a neonatal intensive care unit. J Perinatol. 2013;35(3):218–22.
Rogers S, Babgi A, Gomez C. Educational interventions in end-of-life care: part I: an educational intervention responding to the moral distress of NICU nurses provided by an ethics consultation team. Adv Neonatal Care. 2008;8(1):56–65.
Zargham-Boroujeni A, Zoafa A, Marofi M, Badiee Z. Compilation of the neonatal palliative care clinical guideline in neonatal intensive care unit. Iran J Nurs Midwifery Res. 2015;20(3):309–14.
VandenBerg KA. Individualized developmental care for high-risk newborns in the NICU: A practice guideline. Early Hum Dev. 2007;83(7):433–42.
Caitlin A, Carter B. Creation of a neonatal end-of-life palliative care protocol. J Perinatol. 2002;22(3):184–95.
Nelson JE, Curtis JR, Mulkerin C, Campbell M, Lustbader DR, Mosenthal AC, et al. Choosing and using screening criteria for palliative care consultation in the ICU: a report from the improving palliative care in the ICU (IPAL-ICU) advisory board. Crit Care Med. 2013;41(10):2318–27.
Bradley CT, Brasel KJ. Developing guidelines that identify patient who would benefit from palliative care services in the surgical intensive care unit. Crit Care Med. 2009;37(3):946–50.
Creutzfeldt CJ, Wunsch H, Curtis JR, Hua M. Prevalence and outcomes of patients meeting palliative care consultation triggers in neurological intensive care units. Neurocrit Care. 2015;23(1):14–21.
Hua MS, Li G, Blinderman CD, Wunsch H. Estimate of the need for palliative care consultation across United States intensive care units using a trigger-based model. Am J Respir Crit Care Med. 2014;189(4):428–36.
Boss R, Nelson J, Weissman D, Campbell M, Curtis R, Frontera J, et al. Integrating palliative care into the PICU: a report from the Improving Palliative Care in the ICU advisory board. Pediatr Crit Care Med. 2014;15(8):762–7.
Carter BS, Bhatia J. Comfort/palliative care guidelines for neonatal practice: development and implementation in an academic medical center. J Perinatol. 2001;21(5):279–83.
Bidegain M, Younge N. Comfort care vs palliative care: is there a difference in neonates? Neoreviews. 2015;16(6):e333–9.
Caeymaex L, Speranza M, Vasilescu C, Danan C, Bourrat MM, Garel M, et al. Living with a crucial decision: a qualitative study of parental narratives three years after the loss of their newborn in the NICU. PLoS One. 2011;6(12):e28633.
Verhagen AA, de Vos M, Dorscheidt J, Engels B, Hubben JH, Sauer PJ. Conflicts about end-of-life decisions in NICUs in the Netherlands. Pediatr. 2009;124(1):e112–9.
Nelson JE, Bassett R, Boss RD, Brasel KJ, Campbell ML, Cortez TB, et al. Models for structuring a clinical initiative to enhance palliative care in the intensive care unit: a report from the IPAL-ICU Project (Improving Palliative Care in the ICU). Crit Care Med. 2010;38(9):1765–72.
Kain V, Gardner G, Yates P. Neonatal palliative care attitude scale: development of an instrument to measure the barriers to and facilitators of palliative care in neonatal nursing. Pediatr. 2009;123(2):e207–13.
Mendel TR. The use of neonatal palliative care: Reducing moral distress in NICU nurses. J Neonatal Nurs. 2014;20(6):290–3.
Kilcullen M, Ireland S. Palliative care in the neonatal unit: neonatal nursing staff perceptions of facilitators and barriers in a regional tertiary nursery. BMC Palliat Care. 2017;16(1):32 https://doi.org/10.1186/s12904-017-0202-3
Lam V, Kain N, Joynt C, van Manen MA. A descriptive report of end-of-life care practices occurring in two neonatal intensive care units. Palliat Med. 2016;30(10):971–8.
Gilmour D, Davies MW, Herbert AR. Adequacy of palliative care in a single tertiary neonatal unit. J Paediatr Child Health. 2017;53(2):136–44.
Acknowledgements
We acknowledge the Department of Neonatal and Perinatal Medicine at St. Christopher’s Hospital for Children, including all fellows and faculty, all the nursing staff and nurse practioners in the NICU, and the members of the CORE Palliative Care team.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Electronic supplementary material
Rights and permissions
About this article
Cite this article
Nguyen, L.T., Cooperberg, D.B. & Spear, M.L. Introduction of triggers for palliative care consultation improves utilization and satisfaction within a level four NICU. J Perinatol 38, 574–579 (2018). https://doi.org/10.1038/s41372-018-0067-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41372-018-0067-1
This article is cited by
-
Neonatal palliative care: perception differences between providers
Journal of Perinatology (2020)