Abstract
Objective
To evaluate the impact of first trimester fasting glucose (FTFG) level on perinatal outcome.
Study design
A retrospective cohort study of singleton deliveries. Maternal and neonatal outcome were compared between two groups—women with FTFG < 95 mg/dl and FTFG ≥ 95 mg/dl. Women with pre-gestational diabetes were excluded.
Results
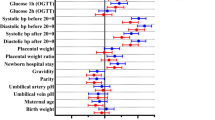
Five thousand and thirty women met inclusion criteria. Of whom, 4644 (92.3%) had FTFG < 95 mg/dl and 386 (7.7%) had FTFG ≥ 95 mg/dl. Women with FTFG ≥ 95 mg/dl had higher rates of gestational hypertension (2.33 vs. 0.7%) and gestational diabetes (9.07 vs. 2.86%), p < 0.05 for both. Moreover, they had higher rates of cesarean delivery and arrest of descent, p < 0.05. Composite diabetes outcome was significantly higher among women with FTFG ≥ 95 mg/dl (8 vs. 3%, p = 0.002).
After adjusting for potential confounders, composite diabetes outcome (aOR = 1.942 95% CI 1.265–2.981, p = 0.002) and gestational hypertension (aOR = 2.827 95% CI 1.295–6.175, p = 0.009) remained significantly higher in the FTFG ≥ 95 mg/dl group.
Conclusion
FTFG ≥ 95 mg/dl is an independent risk factor for adverse perinatal outcome including gestational hypertension and diabetes-related complications.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout

Similar content being viewed by others
References
Al Wattar BH, Tamilselvan K, Khan R, Kelso A, Sinha A, Pirie AM, et al. 2. Classification and diagnosis of diabetes. Diabetes Care. 2017;40:S11–24.
Paglia MJ, Coustan DR. Committee opinion No. 504. Obstet Gynecol. 2011;118:751–3.
Jacobson JD, Cousins L. A population-based study of maternal and perinatal outcome in patients with gestational diabetes. Am J Obstet Gynecol. 1989;161:981–6.
Vignoles P, Gire C, Mancini J, Bretelle F, Boubli L, Janky E, et al. Gestational diabetes: a strong independent risk factor for severe neonatal respiratory failure after 34 weeks. Arch Gynecol Obstet. 2011;284:1099–104.
Naylor CD, Sermer M, Chen E, Sykora K. Cesarean delivery in relation to birth weight and gestational glucose tolerance: pathophysiology or practice style? Toronto Trihospital Gestational Diabetes Investigators. JAMA. 1996;275:1165–70.
Roeckner JT, Sanchez-Ramos L, Jijon-Knupp R, Kaunitz AM. Single abnormal value on 3-hour oral glucose tolerance test during pregnancy is associated with adverse maternal and neonatal outcomes: a systematic review and metaanalysis. Am J Obstet Gynecol. 2016;215:287–97.
Dollberg S, Haklai Z, Mimouni FB, Gorfein I, Gordon ES. Birthweight standards in the live-born population in Israel. Isr Med Assoc J. 2005;7:311–4.
Barquiel B, Herranz L, Grande C, Castro-Dufourny I, llaro M, Parra P, et al. Body weight, weight gain and hyperglycaemia are associated with hypertensive disorders of pregnancy in women with gestational diabetes. Diabetes Metab. 2014;40:204–10.
Nerenberg K, Daskalopoulou SS, Dasgupta K. Gestational diabetes and hypertensive disorders of pregnancy as vascular risk signals: an overview and grading of the evidence. Can J Cardiol. 2014;30:765–73.
Metzger BE, Lowe LP, Dyer AR, Trimble ER, Chaovarindr U, Coustan DR, et al. Hyperglycemia and adverse pregnancy outcomes. N Engl J Med. 2008;358:1991–2002.
Ethridge JK, Catalano PM, Waters TP. Perinatal outcomes associated with the diagnosis of gestational diabetes made by the international association of the diabetes and pregnancy study groups criteria. Obstet Gynecol. 2014;124:571–8.
Boulet SL, Alexander GR, Salihu HM, Pass M. Macrosomic births in the United States: determinants, outcomes, and proposed grades of risk. Am J Obstet Gynecol. 2003;188:1372–8.
Chavkin U, Wainstock T, Sheiner E, Sergienko R, Walfisch A. Perinatal outcome of pregnancies complicates with extreme birth weights at term. J Matern Neonatal Med. 2017;19:1–15.
Bateman BT, Berman MF, Riley LE, Leffert LR. The epidemiology of postpartum hemorrhage in a large, nationwide sample of deliveries. Anesth Analg. 2010;110:1368–73.
Conway DL, Langer O. Elective delivery of infants with macrosomia in diabetic women: reduced shoulder dystocia versus increased cesarean deliveries. Am J Obstet Gynecol. 1998;178:922–5.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Both affiliated to the Sackler Faculty of Medicine, Tel-Aviv University, Tel -Aviv, Israel
Rights and permissions
About this article
Cite this article
Salman, L., Arbib, N., Borovich, A. et al. The impact of first trimester fasting glucose level on adverse perinatal outcome. J Perinatol 38, 451–455 (2018). https://doi.org/10.1038/s41372-018-0045-7
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41372-018-0045-7