Abstract
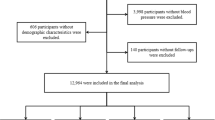
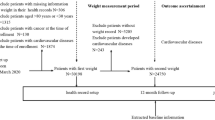
We aimed to determine the association between ideal cardiovascular health metrics (ICVHM) and the incidence of hypertension among Iranian adults. The study population included 5409 Iranian adults aged ≥20 years (2088 men) without hypertension (applying the 2017 American College of Cardiology (ACC)/American Heart Association (AHA) guideline) at baseline. The ICVHM was defined according to the AHA’s 2020 impact goals, excluding total cholesterol was replaced by non-HDL cholesterol (non-HDL-C). Multivariable Cox proportional hazards regression analysis was done to estimate the hazard ratios (HRs) for ICVHM both as continuous and categorical variables. During a median 8.5-year follow-up, 2972 new cases of hypertension were identified (men: 1,287). Non-HDL-C < 130 mg/dL in men [HR (95% CI): 0.75(0.65–0.86)] and fasting plasma glucose(FPG) < 100 mg/dL in women[HR (95% CI): 0.79(0.64–0.97)], and among both genders, being normal/overweigth status (compared to obese) and blood pressure <120/80 mmHg were associated with a lower risk for hypertension. Additionally, in both gender, a 1-point increase in the number of global ICVHM decreased the risk of hypertension by more than 10%, and having ≥5 vs. <2 ICVHM, were associated with a lower risk of hypertension by 30% (all p values < 0.05). Applying the JNC 7 guideline, the association between ICVHM, with incident hypertension, were generally similar. Having a higher number of ICVHM was associated with a lower risk of incident hypertension, using both 2017 ACC/AHA and JNC 7 guidelines, mostly attributable to keeping the ideal status of body mass index, non-HDL-C, and FPG.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 digital issues and online access to articles
$119.00 per year
only $9.92 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout

Similar content being viewed by others
Data availability
The data and code underlying this article will be shared on reasonable request to the corresponding author.
References
Zhou B, Carrillo-Larco RM, Danaei G, Riley LM, Paciorek CJ, Stevens GA, et al. Worldwide trends in hypertension prevalence and progress in treatment and control from 1990 to 2019: a pooled analysis of 1201 population-representative studies with 104 million participants. Lancet. 2021;398:957–80.
Organization WH Guideline for the pharmacological treatment of hypertension in adults. Geneva: World Health Organization. 2021.
Hunter PG, Chapman FA, Dhaun N. Hypertension: Current trends and future perspectives. Br J Clin Pharmacol. 2021;87:3721–36.
Zhou B, Perel P, Mensah GA, Ezzati M. Global epidemiology, health burden and effective interventions for elevated blood pressure and hypertension. Nat Rev Cardiol. 2021;18:785–802.
Oori MJ, Mohammadi F, Norozi K, Fallahi-Khoshknab M, Ebadi A, Gheshlagh RG. Prevalence of HTN in Iran: meta-analysis of published studies in 2004-2018. Curr Hypertens Rev. 2019;15:113–22.
Asgari S, Moazzeni SS, Azizi F, Abdi H, Khalili D, Hakemi MS, et al. Sex-specific incidence rates and risk factors for hypertension during 13 years of follow-up: The tehran lipid and glucose study. Glob Heart. 2020;15:29.
Chobanian AV, Bakris GL, Black HR, Cushman WC, Green LA, Izzo JL Jr, et al. The seventh report of the Joint National Committee on prevention, detection, evaluation, and treatment of high blood pressure: the JNC 7 report. Jama. 2003;289:2560–71.
Lloyd-Jones DM, Hong Y, Labarthe D, Mozaffarian D, Appel LJ, Van Horn L, et al. Defining and setting national goals for cardiovascular health promotion and disease reduction: the American Heart Association’s strategic Impact Goal through 2020 and beyond. Circulation. 2010;121:586–613.
Lloyd-Jones DM, Allen NB, Anderson CA, Black T, Brewer LC, Foraker RE, et al. Life’s Essential 8: updating and enhancing the American Heart Association’s construct of cardiovascular health: a presidential advisory from the American Heart Association. Circulation. 2022;146:e18–e43.
Rahmani F, Asgari S, Khalili D, Habibi Moeini AS, Tohidi M, Azizi F, et al. National trends in cardiovascular health metrics among Iranian adults using results of three cross-sectional STEPwise approaches to surveillance surveys. Sci Rep. 2021;11:1–11.
Dong Y, Hao G, Wang Z, Wang X, Chen Z, Zhang L. Ideal cardiovascular health status and risk of cardiovascular disease or all-cause mortality in chinese middle-aged population. Angiology. 2019;70:523–9.
Ramírez-Vélez R, Saavedra JM, Lobelo F, Celis-Morales CA, del Pozo-Cruz B, García-Hermoso A, editors. Ideal cardiovascular health and incident cardiovascular disease among adults: a systematic review and meta-analysis. Mayo Clinic Proceedings; 2018: Elsevier.
Booth JN III, Abdalla M, Tanner RM, Diaz KM, Bromfield SG, Tajeu GS, et al. Cardiovascular health and incident hypertension in blacks: JHS (The Jackson Heart Study). Hypertension. 2017;70:285–92.
Zhao HY, Liu XX, Wang AX, Wu YT, Zheng XM, Zhao XH, et al. Ideal cardiovascular health and incident hypertension: The longitudinal community-based Kailuan study. Medicine. 2016;95:e5415.
Plante TB, Koh I, Judd SE, Howard G, Howard VJ, Zakai NA, et al. Life’s simple 7 and incident hypertension: the REGARDS study. J Am Heart Assoc. 2020;9:e016482.
Suzuki Y, Kaneko H, Yano Y, Okada A, Itoh H, Matsuoka S, et al. Association of cardiovascular health metrics with risk of transition to hypertension in non-hypertensive young adults. Am J Hypertens. 2022;35:858–66.
Whelton PK, Carey RM, Aronow WS, Casey DE, Collins KJ, Dennison Himmelfarb C, et al. 2017 ACC/AHA/AAPA/ABC/ACPM/AGS/APhA/ASH/ASPC/NMA/PCNA guideline for the prevention, detection, evaluation, and management of high blood pressure in adults: a report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. J Am Coll Cardiol. 2018;71:e127–e248.
Azizi F, Ghanbarian A, Momenan AA, Hadaegh F, Mirmiran P, Hedayati M, et al. Prevention of non-communicable disease in a population in nutrition transition: Tehran Lipid and Glucose Study phase II. Trials. 2009;10:1–15.
Azizi F, Zadeh-Vakili A, Takyar M. Review of rationale, design, and initial findings: Tehran Lipid and Glucose Study. Int J Endocrinol Metab. 2018;16:e84777.
Organization WH MONICA Manual, Part III, Section 1: Population Survey Data Component. WHO Press Geneva, Switzerland; 1997.
Derakhshan A, Sardarinia M, Khalili D, Momenan AA, Azizi F, Hadaegh F. Sex specific incidence rates of type 2 diabetes and its risk factors over 9 years of follow-up: Tehran Lipid and Glucose Study. PloS One. 2014;9:e102563.
Momenan AA, Delshad M, Sarbazi N, Rezaei_Ghaleh N, Ghanbarian A, Azizi F. Reliability and validity of the Modifiable Activity Questionnaire (MAQ) in an Iranian urban adult population. Archives of Iranian medicine. 2012;15:279–82.
Mirmiran P, Esfahani FH, Mehrabi Y, Hedayati M, Azizi F. Reliability and relative validity of an FFQ for nutrients in the Tehran lipid and glucose study. Public health nutrition. 2010;13:654–62.
Fung TT, Chiuve SE, McCullough ML, Rexrode KM, Logroscino G, Hu FB. Adherence to a DASH-style diet and risk of coronary heart disease and stroke in women. Archives of internal medicine. 2008;168:713–20.
Joseph JJ, Bennett A, Tcheugui JBE, Effoe VS, Odei JB, Hidalgo B, et al. Ideal cardiovascular health, glycaemic status and incident type 2 diabetes mellitus: the REasons for Geographic and Racial Differences in Stroke (REGARDS) study. Diabetologia. 2019;62:426–37.
Sun D, Liu J, Xiao L, Liu Y, Wang Z, Li C, et al. Recent development of risk-prediction models for incident hypertension: An updated systematic review. PloS One. 2017;12:e0187240.
Roth GA, Huffman MD, Moran AE, Feigin V, Mensah GA, Naghavi M, et al. Global and regional patterns in cardiovascular mortality from 1990 to 2013. Circulation. 2015;132:1667–78.
Roth GA, Mensah GA, Johnson CO, Addolorato G, Ammirati E, Baddour LM, et al. Global burden of cardiovascular diseases and risk factors, 1990–2019: update from the GBD 2019 study. J Am Coll Cardiol. 2020;76:2982–3021.
Chichester S, Holmes TM, Hubbard J. Ideal body weight: a commentary. Clin Nutr ESPEN. 2021;46:246–50.
American Heart Association. Overweight and Obesity Statistics—2009 Update. Circulation 2009;119:e21–e181.
Flegal KM, Carroll MD, Ogden CL, Johnson CL. Prevalence and trends in obesity among US adults, 1999-2000. JAMA. 2002;288:1723–7.
Hall JE, do Carmo JM, da Silva AA, Wang Z, Hall ME. Obesity-induced hypertension: interaction of neurohumoral and renal mechanisms. Circ Res. 2015;116:991–1006.
Leggio M, Lombardi M, Caldarone E, Severi P, D’emidio S, Armeni M, et al. The relationship between obesity and hypertension: an updated comprehensive overview on vicious twins. Hypertens Res. 2017;40:947–63.
Diederichs C, Neuhauser H. The incidence of hypertension and its risk factors in the German adult population: results from the German National Health Interview and Examination Survey 1998 and the German Health Interview and Examination Survey for Adults 2008–2011. J Hypertens. 2017;35:250–8.
Robitaille C, Dai S, Waters C, Loukine L, Bancej C, Quach S, et al. Diagnosed hypertension in Canada: incidence, prevalence and associated mortality. CMAJ. 2012;184:E49–E56.
Mohammadi M, Mirzaei M. Population-attributable fraction of hypertension associated with obesity, abdominal obesity, and the joint effect of both in the central provinces of Iran. J Epidemiol Glob health. 2017;7:71–9.
Levin G, Kestenbaum B, Ida Chen Y-D, Jacobs DR Jr, Psaty BM, Rotter JI, et al. Glucose, insulin, and incident hypertension in the multi-ethnic study of atherosclerosis. Am J Epidemiol. 2010;172:1144–54.
Arshi B, Tohidi M, Derakhshan A, Asgari S, Azizi F, Hadaegh F. Sex-specific relations between fasting insulin, insulin resistance and incident hypertension: 8.9 years follow-up in a Middle-Eastern population. J Hum Hypertens. 2015;29:260–7.
Tatsumi Y, Ohkubo T. Hypertension with diabetes mellitus: significance from an epidemiological perspective for Japanese. Hypertens Res. 2017;40:795–806.
Asgari S, Masrouri S, Hosseinpour‐Niazi S, Moslehi N, Azizi F, Hadaegh F. Association of ideal cardiovascular health metrics and incident type 2 diabetes mellitus among an urban population of Iran: One decade follow up in the Tehran Lipid and Glucose Study. J Diabetes Investig. 2022;13:1711–22.
Agongo G, Raal F, Nonterah EA, Debpuur C, Oduro AR, Ramsay M, et al. Non-HDL-C and LDL-C/HDL-C are associated with self-reported cardiovascular disease in a rural West African population: Analysis of an array of lipid metrics in an AWI-Gen sub-study. Plos One. 2022;17:e0278375.
Ding C, Chen Y, Shi Y, Li M, Hu L, Zhou W, et al. Association between nontraditional lipid profiles and peripheral arterial disease in Chinese adults with hypertension. Lipids Health Dis. 2020;19:1–9.
Chen S, Cheng W. Relationship between lipid profiles and hypertension: a cross-sectional study of 62,957 Chinese adult males. Front Public Health. 2022;10:895499.
Xie H, Zhuang Q, Mu J, Sun J, Wei P, Zhao X, et al. The relationship between lipid risk score and new-onset hypertension in a prospective cohort study. Front Endocrinol. 2022;13:916951.
Otsuka T, Takada H, Nishiyama Y, Kodani E, Saiki Y, Kato K, et al. Dyslipidemia and the risk of developing hypertension in a working‐age male population. J Am Heart Assoc. 2016;5:e003053.
Sesso HD, Buring JE, Chown MJ, Ridker PM, Gaziano JM. A prospective study of plasma lipid levels and hypertension in women. Arch Intern Med. 2005;165:2420–7.
Lan R, Bulsara MK, Pant PD, Wallace HJ. Relationship between cigarette smoking and blood pressure in adults in Nepal: A population-based cross-sectional study. PLOS Glob Public Health. 2021;1:e0000045.
Kaplan RC, Baldoni PL, Strizich GM, Pérez-Stable EJ, Saccone NL, Peralta CA, et al. Current smoking raises risk of incident hypertension: Hispanic Community Health Study–Study of Latinos. Am J Hypertens. 2021;34:190–7.
Ebina T. Smoking and incident hypertension―importance of Cotinine-verified smoking status―. Circ J. 2018;82:1510–2.
Razmpoosh E, Moslehi N, Abdollahi S, Soltani S, Mirmiran P, Azizi F. The Mediterranean, DASH, and MIND diets and the incident of hypertension over a median follow-up of 7.4 years in the Tehran Lipid and Glucose Study. BMC Public Health. 2022;22:2374.
Folsom AR, Parker ED, Harnack LJ. Degree of concordance with DASH diet guidelines and incidence of hypertension and fatal cardiovascular disease. Am J Hypertens. 2007;20:225–32.
Bai G, Zhang J, Zhao C, Wang Y, Qi Y, Zhang B. Adherence to a healthy lifestyle and a DASH-style diet and risk of hypertension in Chinese individuals. Hypertens Res. 2017;40:196–202.
Hosseinpour-Niazi S, Hadaegh F, Mirmiran P, Daneshpour MS, Mahdavi M, Azizi F. Effect of legumes in energy reduced dietary approaches to stop hypertension (DASH) diet on blood pressure among overweight and obese type 2 diabetic patients: a randomized controlled trial. Diabetol Metab Syndr. 2022;14:72.
Author information
Authors and Affiliations
Contributions
SA, FR, and FH conceived and planned the study. FA cooperated in data gathering. SA conducted the analyses. SA, FR, and FH developed the first draft of the manuscript. All authors have read and approved the final manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethics approval
This study was approved by the Institutional Review Board (IRB) of the Research Institute for Endocrine Sciences (RIES), Shahid Beheshti University of Medical Sciences, Tehran, Iran, and all participants provided written informed consent.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Rahmani, F., Asgari, S., Azizi, F. et al. The association of ideal cardiovascular health metrics and incident hypertension among an urban population of Iran: a decade follow-up in Tehran Lipid and Glucose Study. J Hum Hypertens 38, 267–276 (2024). https://doi.org/10.1038/s41371-023-00881-3
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41371-023-00881-3