Abstract
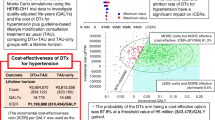
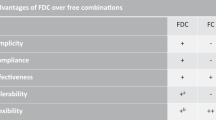
Hypertension guidelines recommend initiating treatment with single pill combination (SPC) antihypertensive medications, but SPCs are used by only one-third of treated hypertensive US adults. This analysis estimated the cost-effectiveness of initial treatment with SPC dual antihypertensive medications compared with usual care monotherapy in hypertensive US adults.
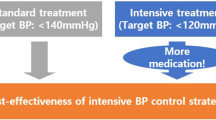
The validated BP Control Model-Cardiovascular Disease (CVD) Policy Model simulated initial SPC dual therapy (two half-standard doses in a single pill) compared with initial usual care monotherapy (half-standard dose when baseline systolic BP < 20 mmHg above goal and one standard dose when ≥20 mmHg above goal). Secondary analyses examined equivalent dose monotherapy (one standard dose) and equivalent dose dual therapy as separate pills (two half-standard doses). The primary outcomes were direct healthcare costs, quality-adjusted life-years (QALYs), and incremental cost-effectiveness ratio (ICER) over 10 years from a US healthcare sector perspective.
At 10 years, initial dual drug SPC was projected to yield 0.028 (95%UI 0.008 to 0.051) more QALYs at no greater cost ($73, 95%UI -$1 983 to $1 629) than usual care monotherapy. In secondary analysis, SPC dual therapy was cost-effective vs. equivalent dose monotherapy (ICER $8 000/QALY gained) and equivalent dose dual therapy as separate pills (ICER $57 000/QALY gained). At average drug prices, initiating antihypertensive treatment with SPC dual therapy is more effective at no greater cost than usual care initial monotherapy and has the potential to improve BP control rates and reduce the burden of CVD in the US.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 digital issues and online access to articles
$119.00 per year
only $9.92 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout



Similar content being viewed by others
Data availability
Supplemental methods, tables, and figures can be found in the supplemental material. Additional data and code are available from the corresponding author on reasonable request.
References
Muntner P, Hardy ST, Fine LJ, Jaeger BC, Wozniak G, Levitan EB, et al. Trends in blood pressure control among US adults with hypertension, 1999-2000 to 2017-2018. JAMA. 2020;324:1190–1200. https://doi.org/10.1001/jama.2020.14545.
U.S. Department of Health and Human Services. The Surgeon General’s Call to Action to Control Hypertension. Washington, DC: U.S. Department of Health and Human Services, Office of the Surgeon General; 2020.
Parati G, Kjeldsen S, Coca A, Cushman WC, Wang J. Adherence to single-pill versus free-equivalent combination therapy in hypertension: a systematic review and meta-analysis. Hypertension. 2021;77:692–705. https://doi.org/10.1161/HYPERTENSIONAHA.120.15781.
Chow CK, Atkins ER, Hillis GS, Nelson MR, Reid CM, Schlaich MP, et al. Initial treatment with a single pill containing quadruple combination of quarter doses of blood pressure medicines versus standard dose monotherapy in patients with hypertension (QUARTET): a phase 3, randomised, double-blind, active-controlled trial. Lancet. 2021;398:1043–52. https://doi.org/10.1016/S0140-6736(21)01922-X.
Law MR, Wald NJ, Morris JK, Jordan RE. Value of low dose combination treatment with blood pressure lowering drugs: analysis of 354 randomised trials. BMJ. 2003;326:1427–0. https://doi.org/10.1136/bmj.326.7404.1427.
Wald DS, Law M, Morris JK, Bestwick JP, Wald NJ. Combination therapy versus monotherapy in reducing blood pressure: meta-analysis on 11,000 participants from 42 trials. Am J Med. 2009;122:290–300. https://doi.org/10.1016/j.amjmed.2008.09.038.
Derington CG, King JB, Herrick JS, Shimbo D, Kronish IM, Saseen JJ, et al. Trends in antihypertensive medication monotherapy and combination use among US adults, National Health and Nutrition Examination Survey 2005–2016. Hypertension. 2020;75:973–81. https://doi.org/10.1161/HYPERTENSIONAHA.119.14360.
Whelton PK, Carey RM, Aronow WS, Casey DE Jr, Collins KJ, Dennison Himmelfarb C, et al. 2017 ACC/AHA/AAPA/ABC/ACPM/AGS/APhA/ASH/ASPC/NMA/PCNA guideline for the prevention, detection, evaluation, and management of high blood pressure in adults: a report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. Hypertension. 2018;71:e13–e115. https://doi.org/10.1161/HYP.0000000000000065.
Williams B, Mancia G, Spiering W, Agabiti Rosei E, Azizi M, Burnier M, et al. 2018 ESC/ESH guidelines for the management of arterial hypertension: the Task Force for the Management of Arterial Hypertension of the European Society of Cardiology (ESC) and the European Society of Hypertension (ESH). Eur Heart J. 2018;39:3021–104. https://doi.org/10.1093/eurheartj/ehy339.
Derington CG, Cohen JB, Bress AP. Restoring the upward trend in blood pressure control rates in the United States: a focus on fixed-dose combinations. J Hum Hypertens. 2020;34:617–23. https://doi.org/10.1038/s41371-020-0340-6.
Rabbani A, Alexander GC. Out-of-pocket and total costs of fixed-dose combination antihypertensives and their components. Am J Hypertens. 2008;21:509–13.
Fontil V, Bibbins-Domingo K, Kazi DS, Sidney S, Coxson PG, Khanna R, et al. Simulating strategies for improving control of hypertension among patients with usual source of care in the United States: The Blood Pressure Control Model. J Gen Intern Med. 2015;30:1147–55. https://doi.org/10.1007/s11606-015-3231-8.
Bryant KB, Moran AE, Kazi DS, Zhang Y, Penko J, Ruiz-Negrón N, et al. Cost-effectiveness of hypertension treatment by pharmacists in Black barbershops. Circulation. 2021;143:2384–94. https://doi.org/10.1161/CIRCULATIONAHA.120.051683.
Bellows BK, Ruiz-Negrón N, Bibbins-Domingo K, King JB, Pletcher MJ, Moran AE, et al. Clinic-based strategies to reach United States Million Hearts 2022 blood pressure control goals. Circ Cardiovasc Qual Outcomes. 2019;12:e005624 https://doi.org/10.1161/CIRCOUTCOMES.118.005624.
Kohli-Lynch CN, Bellows BK, Thanassoulis G, Zhang Y, Pletcher MJ, Vittinghoff E, et al. Cost-effectiveness of low-density lipoprotein cholesterol level–guided statin treatment in patients with borderline cardiovascular risk. JAMA Cardiol. 2019;4:969 https://doi.org/10.1001/jamacardio.2019.2851.
Kohli-Lynch CN, Bellows BK, Zhang Y, Spring B, Kazi DS, Pletcher MJ, et al. Cost-effectiveness of lipid-lowering treatments in young adults. J Am Coll Cardiol. 2021;78:1954–64. https://doi.org/10.1016/j.jacc.2021.08.065.
Zeki Al Hazzouri A, Vittinghoff E, Zhang Y, Pletcher MJ, Moran AE, Bibbins-Domingo K, et al. Use of a pooled cohort to impute cardiovascular disease risk factors across the adult life course. Int J Epidemiol. 2019;48:1004–13. https://doi.org/10.1093/ije/dyy264.
Oelsner EC, Balte PP, Cassano PA, Couper D, Enright PL, Folsom AR, et al. Harmonization of respiratory data from 9 US population-based cohorts: the NHLBI Pooled Cohorts Study. Am J Epidemiol. 2018;187:2265–78. https://doi.org/10.1093/aje/kwy139.
Law M, Wald N, Morris J. Lowering blood pressure to prevent myocardial infarction and stroke: a new preventive strategy. Health Technol Assess. 2003;7:1–94. https://doi.org/10.3310/hta7310.
Law MR, Morris JK, Wald NJ. Use of blood pressure lowering drugs in the prevention of cardiovascular disease: meta-analysis of 147 randomised trials in the context of expectations from prospective epidemiological studies. BMJ. 2009;338:b1665 https://doi.org/10.1136/bmj.b1665.
Lowy A, Munk VC, Ong SH, Burnier M, Vrijens B, Tousset EP, et al. Effects on blood pressure and cardiovascular risk of variations in patients’ adherence to prescribed antihypertensive drugs: role of duration of drug action. Int J Clin Pr. 2011;65:41–53. https://doi.org/10.1111/j.1742-1241.2010.02569.x.
Bryant KB, Sheppard JP, Ruiz-Negrón N, Kronish IM, Fontil V, King JB, et al. Impact of self-monitoring of blood pressure on processes of hypertension care and long-term blood pressure control. J Am Heart Assoc. 2020;9:e016174 https://doi.org/10.1161/JAHA.120.016174.
Claxton AJ, Cramer J, Pierce C. A systematic review of the associations between dose regimens and medication compliance. Clin Ther. 2001;23:1296–310. https://doi.org/10.1016/s0149-2918(01)80109-0.
Vrijens B, Vincze G, Kristanto P, Urquhart J, Burnier M. Adherence to prescribed antihypertensive drug treatments: longitudinal study of electronically compiled dosing histories. BMJ. 2008;336:1114–7. https://doi.org/10.1136/bmj.39553.670231.25.
Levy J, Rosenberg M, Vanness D. A Transparent and consistent approach to assess US outpatient drug costs for use in cost-effectiveness analyses. Value Health. 2018;21:677–84. https://doi.org/10.1016/j.jval.2017.06.013.
Ettehad D, Emdin CA, Kiran A, Anderson SG, Callender T, Emberson J, et al. Blood pressure lowering for prevention of cardiovascular disease and death: a systematic review and meta-analysis. Lancet. 2016;387:957–67. https://doi.org/10.1016/S0140-6736(15)01225-8.
Price Indexes for Personal Consumption Expenditures by Type of Product. Bureau of Economic Analysis, U.S. Department of Commerce, 2019. Accessed August 12, 2021. https://apps.bea.gov/iTable/iTable.cfm?reqid=19&step=2#reqid=19&step=2&isuri=1&1921=underlying.
Anderson JL, Heidenreich PA, Barnett PG, Creager MA, Fonarow GC, Gibbons RJ, et al. ACC/AHA statement on cost/value methodology in clinical practice guidelines and performance measures: a report of the American College of Cardiology/American Heart Association Task Force on Performance Measures and Task Force on Practice Guidelines. J Am Coll Cardiol. 2014;63:2304–22. https://doi.org/10.1016/j.jacc.2014.03.016.
Salam A, Kanukula R, Atkins E, Wang X, Islam S, Kishore SP, et al. Efficacy and safety of dual combination therapy of blood pressure-lowering drugs as initial treatment for hypertension: a systematic review and meta-analysis of randomized controlled trials. J Hypertens. 2019;37:1768–74. https://doi.org/10.1097/HJH.0000000000002096.
Husereau D, Drummond M, Augustovski F, de Bekker-Grob E, Briggs AH, Carswell C, et al. Consolidated Health Economic Evaluation Reporting Standards 2022 (CHEERS 2022) statement: updated reporting guidance for health economic evaluations. Value Health. 2022;25:3–9. https://doi.org/10.1016/j.jval.2021.11.1351.
Wang X, Chen H, Essien E, Wu J, Serna O, Paranjpe R, et al. Cost-effectiveness analysis of antihypertensive triple combination therapy among patients enrolled in a Medicare advantage plan. Expert Rev Pharmacoecon Outcomes Res. 2021;21:829–836. https://doi.org/10.1080/14737167.2020.1800457.
Lin JK, Moran AE, Bibbins-Domingo K, Falase B, Pedroza Tobias A, Mandke CN, et al. Cost-effectiveness of a fixed-dose combination pill for secondary prevention of cardiovascular disease in China, India, Mexico, Nigeria, and South Africa: a modelling study. Lancet Glob Health. 2019;7:e1346–e1358. https://doi.org/10.1016/S2214-109X(19)30339-0.
Stafylas P, Kourlaba G, Hatzikou M, Georgiopoulos D, Sarafidis P, Maniadakis N. Economic evaluation of a single-pill triple antihypertensive therapy with valsartan, amlodipine, and hydrochlorothiazide against its dual components. Cost Eff Resour Alloc. 2015;13:10 https://doi.org/10.1186/s12962-015-0036-x.
Glasziou PP, Clarke P, Alexander J, Rajmokan M, Beller E, Woodward M, et al. Cost-effectiveness of lowering blood pressure with a fixed combination of perindopril and indapamide in type 2 diabetes mellitus: an ADVANCE trial-based analysis. Med J Aust. 2010;193:320–4. https://doi.org/10.5694/j.1326-5377.2010.tb03941.x.
Lung T, Jan S, Asita de Silva H, Guggilla R, Maulik PK, Naik N, et al. Fixed-combination, low-dose, triple-pill antihypertensive medication versus usual care in patients with mild-to-moderate hypertension in Sri Lanka: a within-trial and modelled economic evaluation of the TRIUMPH trial. Lancet Glob Health. 2019;7:e1359–e1366. https://doi.org/10.1016/S2214-109X(19)30343-2.
Jaffe MG, Lee GA, Young JD, Sidney S, Go AS. Improved blood pressure control associated with a large-scale hypertension program. JAMA. 2013;310:699–705. https://doi.org/10.1001/jama.2013.108769.
Fletcher RD, Amdur RL, Kolodner R, McManus C, Jones R, Faselis C, et al. Blood pressure control among US veterans: a large multiyear analysis of blood pressure data from the Veterans Administration health data repository. Circulation. 2012;125:2462–8. https://doi.org/10.1161/CIRCULATIONAHA.111.029983.
Funding
AEM was supported by R01HL130500, YZ by R01HL158790, VF by K23HL136899, and BKB by K01HL140170, all from the National Heart, Lung, and Blood Institute (NHLBI) (Bethesda, MD). The funders had no role in the design and conduct of the study; collection, management, analysis, and interpretation of the data; preparation, review, approval of the article; or decision to submit the article for publication.
Author information
Authors and Affiliations
Contributions
ASB and BKB had full access to all data in the study and take responsibility for the integrity of the data and the accuracy of the data analysis. Detailed author contributions are below. Concept and design: ASB, AEM, and BKB. Acquisition, analysis, or interpretation of data: All authors. Drafting of the article: ASB, AEM, and BKB. Critical revision of the article for important intellectual content: All authors. Approved the final version of the article: All authors. Statistical analysis: ASB, YZ, and BKB. Obtaining funding: AEM and BKB. Administrative, technical, or material support: BKB. Study supervision: BKB.
Corresponding author
Ethics declarations
Competing interests
CGD reports research funds to her institution from Amarin Pharma, Inc. AR is employed by The George Institute for Global Health (TGI) and Imperial College London. He is seconded part-time to George Medicines Pty Ltd (GM), which is partly owned by George Health Enterprises (GHE), the social enterprise arm of TGI. TGI holds patents for ultra-low-dose fixed-dose combination products for the treatment of hypertension and diabetes, and AR is listed as one of the inventors (US 10,369,15; US 10,799,487; US 10,322,117; US 11,033,544). GHE and GM have received funding from public and private investors to conduct the research required for regulatory approval of cardiovascular combination products. AR does not have a financial interest in these patent applications or investments.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Bryan, A.S., Moran, A.E., Mobley, C.M. et al. Cost-effectiveness analysis of initial treatment with single-pill combination antihypertensive medications. J Hum Hypertens 37, 985–992 (2023). https://doi.org/10.1038/s41371-023-00811-3
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41371-023-00811-3