Abstract
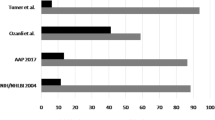
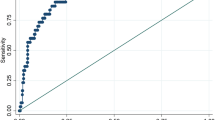
The 2017 American Academy of Pediatrics (AAP) guideline for assessing “elevated blood pressure (BP) (90th BP percentile)” and “high BP (95th BP percentile)” includes a large number of BP cut-offs based on sex, age and height, which makes it cumbersome to use in clinical practice. We developed and evaluated the performance of a simple table based on a child’s height only to assess elevated and high BP in children compared to the reference AAP guideline based on sex, age and height. Data came from 6816 children aged 8–12 years from the U.S. National Health and Nutrition Examination Survey (NHANES) 1999–2016 and 3145 participants aged 5–12 years from NHANES III (1988–1994). Compared to the reference AAP guideline, the simple table had high values of AUC (0.96/0.91), sensitivity (92.7%/83.2%), specificity (99.0%/99.4%), PPV (92.6%/89.3%), NPV (99.0%/99.0%), and Kappa coefficient (0.92/0.85) for screening elevated/high BP when applied to NHANES, and values were similarly high when applied to NHANES III. These findings show that the simple table based on height only performed nearly as well as the reference 2017 AAP guideline based on sex, age and height for assessing elevated and high BP in U.S. children. This simple table may be a useful screening tool to assess high BP in children aged 5–12 years, particularly in a context of mass screening programs.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 digital issues and online access to articles
$119.00 per year
only $9.92 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout
Similar content being viewed by others
References
Kit BK, Kuklina E, Carroll MD, Ostchega Y, Freedman DS, Ogden CL. Prevalence of and trends in dyslipidemia and blood pressure among US children and adolescents, 1999–2012. JAMA Pediatr. 2015;169:272–9.
Noubiap JJ, Essouma M, Bigna JJ, Jingi AM, Aminde LN, Nansseu JR. Prevalence of elevated blood pressure in children and adolescents in Africa: a systematic review and meta-analysis. Lancet. Public Health. 2017;2:E375–86.
Xi B, Bovet P, Hong YM, Zong X, Chiolero A, Kim HS, et al. Recent blood pressure trends in adolescents from China, Korea, Seychelles and the United States of America, 1997–2012. J Hypertens. 2016;34:1948–58.
Sun SS, Grave GD, Siervogel RM, Pickoff AA, Arslanian SS, Daniels SR. Systolic blood pressure in childhood predicts hypertension and metabolic syndrome later in life. Pediatrics. 2007;119:237–46.
Juhola J, Magnussen CG, Berenson GS, Venn A, Burns TL, Sabin MA, et al. Combined effects of child and adult elevated blood pressure on subclinical atherosclerosis: the International Childhood Cardiovascular Cohort Consortium. Circulation. 2013;128:217–24.
Sundstrom J, Neovius M, Tynelius P, Rasmussen F. Association of blood pressure in late adolescence with subsequent mortality: cohort study of Swedish male conscripts. BMJ. 2011;342:d643.
Flynn JT, Kaelber DC, Baker-Smith CM, Blowey D, Carroll AE, Daniels SR, et al. Clinical practice guideline for screening and management of high blood pressure in children and adolescents. Pediatrics. 2017;140:e20171904.
National High Blood Pressure Education Program Working Group on High Blood Pressure in Children and Adolescents. The fourth report on the diagnosis, evaluation, and treatment of high blood pressure in children and adolescents. Pediatrics. 2004;114:555–76.
Bijlsma MW, Blufpand HN, Kaspers GJ, Bokenkamp A. Why pediatricians fail to diagnose hypertension: a multicenter survey. J Pediatr. 2014;164:e7.
Ma C, Kelishadi R, Hong YM, Bovet P, Khadilkar A, Nawarycz T, et al. Performance of eleven simplified methods for the identification of elevated blood pressure in children and adolescents. Hypertension. 2016;68:614–20.
Zhang YY, Yang L, Hou Y, Zhao M, Bovet P, Xi B Performance of the simplified AAP table to screen elevated blood pressure in children. JAMA Pediatr. 2018. https://doi.org/10.1001/jamapediatrics.2018.1923.
Chiolero A, Paradis G, Simonetti GD, Bovet P. Absolute height-specific thresholds to identify elevated blood pressure in children. J Hypertens. 2013;31:1170–4.
McQuillan GM, McLean JE, Chiappa M, Corporation H, Lukacs SL. National Health and Nutrition Examination Survey Biospecimen Program: NHANES III (1988-1994) and NHANES 1999-2014. Vital Health Stat. 2015;2:1–14.
Kuczmarski RJ, Ogden CL, Grummer-Strawn LM, Flegal KM, Guo SS, Wei R. et al.CDC growth charts: United States. Adv Data.2000;8:1–27.
Yang L, Hou Y, Zhao M, Bovet P, Xi B Simplified blood pressure tables based on different height percentiles for screening elevated blood pressure in children. J Hypertens. 2018. https://doi.org/10.1097/HJH.0000000000001880.
Lu Q, Ma CM, Yin FZ, Liu BW, Lou DH, Liu XL. How to simplify the diagnostic criteria of hypertension in adolescents. J Hum Hypertens. 2011;25:159–63.
Yin X, Liu Q, Bovet P, Ma C, Xi B. Performance of blood pressure-to-height ratio as a screening tool for elevated blood pressure in pediatric population: a systematic meta-analysis. J Hum Hypertens. 2016;30:697–702.
Acknowledgements
We thank the National Center for Health Statistic of Centers for Disease Control and Prevention for sharing NAHNES data.
Funding
This work was supported by the National Natural Science Foundation of China (81673195). The sponsors had no role in the study design, survey process, data analysis, and manuscript preparation.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Rights and permissions
About this article
Cite this article
Zhang, Y., Yang, L., Hou, Y. et al. A simple table based on height to assess elevated and high blood pressure in children. J Hum Hypertens 33, 248–254 (2019). https://doi.org/10.1038/s41371-018-0128-0
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41371-018-0128-0