Abstract
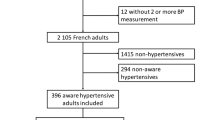
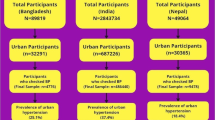
Large differences in blood pressure (BP) control rates have been observed between sub-Saharan African migrant populations in Europe compared to their counterparts living in Africa. Our main objective was to investigate whether inter-geographical differences in BP control rates can be explained by differences in medication non-adherence. Additionally, we studied the prevalence of medication non-adherence and associations between medication non-adherence, socio-demographic-related, clinical/treatment-related, lifestyle factors, and experienced stress on the one hand and BP control on the other hand. We used data from the multi-center RODAM (Research on Obesity and Diabetes Among African Migrants) study, from Ghanaians receiving antihypertensive therapy and residing in three European countries versus non-migrants residing in rural and urban Ghana (n = 1303). Bivariate and multivariate logistic regression analyses stratified by sex were applied. We found inter-geographical differences in BP control rates among Ghanaian males but not among females. Ghanaian males residing in Amsterdam and Berlin had not only the lowest BP control rates but also the lowest rates of medication non-adherence. Inter-geographical differences in BP control rates among males became therefore more pronounced after adjustment for medication adherence. Medication non-adherence was significantly and independently associated with suboptimal BP control in males and females. Other factors associated with suboptimal BP control in females were a higher number of prescribed antihypertensives, higher fasting glucose levels, and pregnancy-induced diabetes. When adjusted for medication non-adherence and socio-demographic-, clinical/treatment-, lifestyle-, and stress-related factors, inter-geographical differences in BP control in males disappeared, except for Berlin. In conclusion, the observed inter-geographical differences in BP control rates in Ghanaian males cannot be explained by differences in medication non-adherence.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 digital issues and online access to articles
$119.00 per year
only $9.92 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout

Similar content being viewed by others
References
Lim SS, Vos T, Flaxman AD, Danaei G, Shibuya K, Adair-Rohani H, et al. A comparative risk assessment of burden of disease and injury attributable to 67 risk factors and risk factor clusters in 21 regions, 1990–2010: a systematic analysis for the Global Burden of Disease Study 2010. lancet. 2013;380:2224–60.
Agyemang C, Addo J, Bhopal R, de Graft Aikins A, Stronks K. Cardiovascular disease, diabetes and established risk factors among populations of sub-Saharan African descent in Europe: a literature review. Glob Health. 2009;5:7
Addo J, Smeeth L, Leon DA. Hypertension in Sub-Saharan Africa: a systematic review. Hypertension. 2007;50:1012–8.
Mancia G, Fagard R, Narkiewicz K, Redon J, Zanchetti A, Böhm M, et al. 2013 ESH/ESC guidelines for the management of arterial hypertension: the Task Force for the Management of Arterial Hypertension of the European Society of Hypertension (ESH) and of the European Society of Cardiology (ESC). Blood Press. 2013;22:193–278.
Cushman WC. The burden of uncontrolled hypertension: morbidity and mortality associated with disease progression. J Clin Hypertens. 2003;5:14–22.
Agyemang C, Kieft S, Snijder MB, Beune EJ, van den Born B-J, Brewster LM, et al. Hypertension control in a large multi-ethnic cohort in Amsterdam, The Netherlands: the HELIUS study. Int J Cardiol. 2015;183:180–9.
Agyemang C, Nyaaba G, Beune E, Meeks K, Owusu-Dabo E, Addo J, et al. Variations in hypertension awareness, treatment, and control among Ghanaian migrants living in Amsterdam, Berlin, London, and nonmigrant Ghanaians living in rural and urban Ghana–the RODAM study. J Hypertens. 2018;36:169–77.
Calhoun DA, Jones D, Textor S, Goff DC, Murphy TP, Toto RD, et al. Resistant hypertension: diagnosis, evaluation, and treatment a scientific statement from the American Heart Association Professional Education Committee of the Council for High Blood Pressure Research. Hypertension. 2008;51:1403–19.
Chobanian AV, Bakris GL, Black HR, Cushman WC, Green LA, Izzo JL Jr., et al. The seventh report of the joint national committee on prevention, detection, evaluation, and treatment of high blood pressure: the JNC 7 report. JAMA. 2003;289:2560–71.
Liu M-Y, Li N, Li WA, Khan H. Association between psychosocial stress and hypertension: a systematic review and meta-analysis. Neurol Res. 2017;39:573–80.
Mennini F, Marcellusi A, von der Schulenburg JG, Gray A, Lévy P, Sciattella P, et al. Cost of poor adherence to anti-hypertensive therapy in five European countries. Eur J Health Econ. 2015;16:65–72.
Boima V, Ademola AD, Odusola AO, Agyekum F, Nwafor CE, Cole H, et al. Factors associated with medication nonadherence among hypertensives in Ghana and Nigeria. Int J Hypertens. 2015;2015:205716.
Kretchy IA, Owusu-Daaku FT, Danquah S. Locus of control and anti-hypertensive medication adherence in Ghana. Pan Afr Med J. 2014;17 Suppl 1:13.
Nielsen JØ, Shrestha A, Neupane D, Kallestrup P. Non-adherence to anti-hypertensive medication in low-and middle-income countries: a systematic review and meta-analysis of 92443 subjects. J Hum Hypertens. 2017;31:14–21.
Agyemang C, Beune E, Meeks K, Owusu-Dabo E, Agyei-Baffour P, Aikins Ad-G, et al. Rationale and cross-sectional study design of the Research on Obesity and type 2 Diabetes among African Migrants: the RODAM study. BMJ Open. 2015;4:e004877.
World Health Organization (WHO). Diagnosis of diabetes mellitus and intermediate hyperglycemia: report of a WHO/IDF consultation. Geneva, World Health Organization 2006.
World Health Organization (WHO). Anatomical Therapeutic Chemical (ATC) classification system: guidelines for ATC classification and DDD assignment. Oslo: WHO Collaborating Centre for Drug Statistics Methodology; 2013.
James PA, Oparil S, Carter BL, Cushman WC, Dennison-Himmelfarb C, Handler J, et al. 2014 evidence-based guideline for the management of high blood pressure in adults: report from the panel members appointed to the Eighth Joint National Committee (JNC 8). JAMA. 2014;311:507–20.
Nieuwkerk PT, Nierman MC, Vissers MN, Locadia M, Greggers-Peusch P, Knape LP, et al. Intervention to improve adherence to lipid-lowering medication and lipid-levels in patients with an increased cardiovascular risk. Am J Cardiol. 2012;110:666–72.
World Health Organization (WHO). WHO STEPS surveillance manual: the WHO STEPwise approach to chronic disease risk factor surveillance. Geneva, World Health Organization 2005.
Kaaks R, Riboli E. Validation and calibration of dietary intake measurements in the EPIC project: methodological considerations. European Prospective Investigation into Cancer and Nutrition. Int J Epidemiol. 1997;26(suppl 1):S15.
Frank LK, Kröger J, Schulze MB, Bedu-Addo G, Mockenhaupt FP, Danquah I. Dietary patterns in urban Ghana and risk of type 2 diabetes. Br J Nutr. 2014;112:89–98.
Williams DR, Yu Y, Jackson JS, Anderson NB. Racial differences in physical and mental health: socio-economic status, stress and discrimination. J Health Psychol. 1997;2:335–51.
Brugha TS, Cragg D. The list of threatening experiences: the reliability and validity of a brief life events questionnaire. Acta Psychiatr Scand. 1990;82:77–81.
Suurmeijer TP, Doeglas DM, Briancon S, Krijnen WP, Krol B, Sanderman R, et al. The measurement of social support in the ‘European Research on Incapacitating Diseases and Social Support’: the development of the Social Support Questionnaire for Transactions (SSQT). Soc Sci Med. 1995;40:1221–9.
Yusuf S, Hawken S, Ôunpuu S, Dans T, Avezum A, Lanas F, et al. Effect of potentially modifiable risk factors associated with myocardial infarction in 52 countries (the INTERHEART study): case-control study. lancet. 2004;364:937–52.
Pereira M, Lunet N, Azevedo A, Barros H. Differences in prevalence, awareness, treatment and control of hypertension between developing and developed countries. J Hypertens. 2009;27:963–75.
Altman D. Comparing groups—categorical data. Pract Stat Med Res. 1991;1:261–5.
van der Laan D, Elders P, Boons C, Beckeringh J, Nijpels G, Hugtenburg J. Factors associated with antihypertensive medication non-adherence: a systematic review. J Hum Hypertens. 2017;31:687.
Beune EJ, van Charante EPM, Beem L, Mohrs J, Agyemang CO, Ogedegbe G, et al. Culturally adapted hypertension education (CAHE) to improve blood pressure control and treatment adherence in patients of African origin with uncontrolled hypertension: cluster-randomized trial. PLoS ONE 2014;9:e90103.
Meinema JG, van Dijk N, Beune EJ, Jaarsma DA, van Weert HC, Haafkens JA. Determinants of adherence to treatment in hypertensive patients of African descent and the role of culturally appropriate education. PLoS ONE 2015;10:e0133560.
Majernick TG, Zacker C, Madden NA, Belletti DA, Arcona S. Correlates of hypertension control in a primary care setting. Am J Hypertens. 2004;17:915–20.
Roberts R. Hypertension in women with gestational diabetes. Diabetes Care. 1998;21:B27.
Beune EJ, Haafkens JA, Agyemang C, Schuster JS, Willems DL. How Ghanaian, African-Surinamese and Dutch patients perceive and manage antihypertensive drug treatment: a qualitative study. J Hypertens. 2008;26:648–56.
Osterberg L, Blaschke T. Adherence to medication. N Engl J Med. 2005;353:487–97.
Stirratt MJ, Dunbar-Jacob J, Crane HM, Simoni JM, Czajkowski S, Hilliard ME, et al. Self-report measures of medication adherence behavior: recommendations on optimal use. Transl Behav Med. 2015;5:470–82.
Elam G, McMunn A, Nazroo J. Feasibility study for health surveys among black African people living in England: Final Report–implications for the Health Survey for England. London: Department of Health; 2001.
Acknowledgements
The authors are very grateful to the advisory board members for their valuable support in shaping the methods, to the research assistants, interviewers and other staff of the five research locations who have taken part in gathering the data, and, most of all, to the Ghanaian volunteers participating in this project. We gratefully acknowledge Lizzy Brewster for her critical feedback on the manuscript and Jan van Straalen from the Academic Medical Centre for his valuable support with standardization of the laboratory procedures.
Funding
This work was supported by the European Commission under the Framework Programme (Grant Number: 278901).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Rights and permissions
About this article
Cite this article
Beune, E., Nieuwkerk, P., Stronks, K. et al. Medication non-adherence and blood pressure control among hypertensive migrant and non-migrant populations of sub-Saharan African origin: the RODAM study. J Hum Hypertens 33, 131–148 (2019). https://doi.org/10.1038/s41371-018-0120-8
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41371-018-0120-8