Abstract
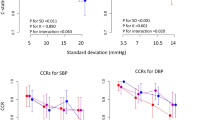
Hypertension is a major cardiovascular risk factor. To address the disease adequately, most clinicians rely on home blood pressure monitoring (HBPM). However, the impact of unrecorded BP values on the precision and diagnostic performance of BP schedules is unknown. We obtained 103 HBP patients schedules from a previous study. Then, readings were randomly removed from each schedule in order to create new incomplete schedules using a resampling technique. We obtained 10,000 new incomplete schedules. For each number of randomly removed readings, the percentages of incomplete schedules outside a systolic/diastolic blood pressure (SBP/DBP) range of 5/3 mmHg were calculated from the same complete patient’s schedule. The sensitivity and specificity of incomplete HBPM schedules regarding BP control were also assessed. One hundred three HBPM schedules were analyzed. Mean patients’ age was 67.9 ± 9.9 years. In non-diabetic patients, the mean BP of complete schedules’ means was 131.9 ± 12.4/75.5 ± 10.5. In diabetic patients, the mean BP of complete schedules’ means was 135.5 ± 14.0/73.4 ± 8.2 mmHg. When schedules were composed of 14 and 21 random measures, differences over 5 mmHg were seen in 2.6% and 0.1% of non-diabetic patients’ schedule and 3.7% and 0.1% of diabetic patients’ schedule, respectively. At 21 measurements, sensitivity and specificity were approximately 95% and 98% in non-diabetic patients and 90% and 99% in non-diabetic patients, respectively. HBPM precision and diagnostic performance improve rapidly with accumulation of readings. Incomplete schedules composed of 21 readings can provide an almost perfect diagnostic tool compared with the complete schedule reference.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 digital issues and online access to articles
$119.00 per year
only $9.92 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout


Similar content being viewed by others
References
Padwal RS, Bienek A, McAlister FA, Campbell NR. Outcomes research task force of the Canadian Hypertension Education Program. Epidemiology of Hypertension in Canada: an update. Can J Cardiol. 2016;32:687–94.
Kannel WB. Blood pressure as a cardiovascular risk factor: prevention and treatment. J Am Med Assoc. 1996;275:1571–6.
Joffres M, Falaschetti E, Gillespie C, Robitaille C, Loustalot F, Poulter N, et al. Hypertension prevalence, awareness, treatment and control in national surveys from England, the USA and Canada, and correlation with stroke and ischaemic heart disease mortality: a cross-sectional study. Br Med J Open. 2013;3:e003423.
Ettehad D, Emdin CA, Kiran A, Anderson SG, Callender T, Emberson J, et al. Blood pressure lowering for prevention of cardiovascular disease and death: a systematic review and meta-analysis. Lancet. 2015;387:957–67.
Cloutier L, Daskalopoulou SS, Padwal RS, Lamarre-Cliche M, Bolli P, McLean D, et al. A new algorithm for the diagnosis of hypertension in Canada. Can J Cardiol. 2015;31:620–30.
Leung AA, Nerenberg K, Daskalopoulou SS, McBrien K, Zarnke KB, Dasgupta K, et al. Hypertension Canada’s 2016 Canadian Hypertension Education Program Guidelines for blood pressure measurement, diagnosis, assessment of risk, prevention, and treatment of hypertension. Can J Cardiol. 2016;32:569–88.
Niiranen TJ, Hänninen M-R, Johansson J, Reunanen A, Jula AM. Home-measured blood pressure is a stronger predictor of cardiovascular risk than office blood pressure: the Finn-Home study. Hypertension. 2010;55:1346–51.
Ohkubo T, Imai Y, Tsuji I, Nagai K, Kato J, Kikuchi N, et al. Home blood pressure measurement has a stronger predictive power for mortality than does screening blood pressure measurement: a population-based observation in Ohasama, Japan. J Hypertens. 1998;16:971–5.
Stergiou GS, Baibas NM, Kalogeropoulos PG. Cardiovascular risk prediction based on home blood pressure measurement: the Didima study. J Hypertens. 2007;25:1590–6.
Bobrie G, Chatellier G, Genes N, Clerson P, Vaur L, Vaisse B, et al. Cardiovascular prognosis of “masked hypertension” detected by blood pressure self-measurement in elderly treated hypertensive patients. J Am Med Assoc. 2004;291:1342–9.
Sega R, Facchetti R, Bombelli M, Cesana G, Corrao G, Grassi G, et al. Prognostic value of ambulatory and home blood pressures compared with office blood pressure in the general population: follow-up results from the Pressioni Arteriose Monitorate e Loro Associazioni (PAMELA) study. Circulation. 2005;111:1777–83.
Ohkubo T, Asayama K, Kikuya M, Metoki H, Hoshi H, Hashimoto J, et al. How many times should blood pressure be measured at home for better prediction of stroke risk? Ten-year follow-up results from the Ohasama study. J Hypertens. 2004;22:1099–104.
Bancej CM, Campbell N, McKay DW, Nichol M, Walker RL, Kaczorowski J. Home blood pressure monitoring among Canadian adults with hypertension: results from the 2009 Survey on Living with Chronic Diseases in Canada. Can J Cardiol. 2010;26:e152–7.
Nordmann A, Frach B, Walker T, Martina B, Battegay E. Reliability of patients measuring blood pressure at home: prospective observational study. Br Med J. 1999;319:1172–1172.
O’Brien E, Parati G, Stergiou G, Asmar R, Beilin L, Bilo G, et al. European Society of Hypertension position paper on ambulatory blood pressure monitoring. J Hypertens. 2013;31:1731–68.
Chatellier G, Day M, Bobrie G, Menard J. Feasibility study of N-of-1 trials with blood pressure self-monitoring in hypertension. Hypertension. 1995;25:294–301.
Stergiou GS, Nasothimiou EG, Kalogeropoulos PG, Pantazis N, Baibas NM. The optimal home blood pressure monitoring schedule based on the Didima outcome study. J Hum Hypertens. 2010;24:158–64.
Niiranen TJ, Asayama K, Thijs L, Johansson JK, Hara A, Hozawa A, et al. Optimal number of days for home blood pressure measurement. Am J Hypertens. 2015;28:595–603.
Parati G, Stergiou GS, Asmar R, Bilo G, de Leeuw P, Imai Y, et al. European Society of Hypertension practice guidelines for home blood pressure monitoring. J Hum Hypertens. 2010;24:779–85.
Imai Y, Kario K, Shimada K, Kawano Y, Hasebe N, Matsuura H, et al. The Japanese Society of Hypertension Guidelines for self-monitoring of blood pressure at home (second edition). Hypertens Res. 2012;35:777–95.
National Institute of Health and Clinical Excellence. Hypertension: clinical management of primary hypertension in adults. In. London: NICE: NICE clinical guideline 127, 2011.
Mengden T, Hernandez Medina RM, Beltran B, Alvarez E, Kraft K, Vetter H. Reliability of reporting self-measured blood pressure values by hypertensive patients. Am J Hypertens. 1998;11:1413–7.
Milot JP, Birnbaum L, Larochelle P, Wistaff R, Laskine M, Van Nguyen P, et al. Unreliability of home blood pressure measurement and the effect of a patient-oriented intervention. Can J Cardiol. 2015;31:658–63.
Myers MG, Stergiou GS. Reporting bias: Achilles’ heel of home blood pressure monitoring. J Am Soc Hypertens. 2014;8:350–7.
Kallioinen N, Hill A, Horswill MS, Ward HE, Watson MO. Sources of inaccuracy in the measurement of adult patients’ resting blood pressure in clinical settings: a systematic review. J Hypertens. 2017;35:421–41.
Acknowledgements
This study would not have been possible without the precious statistical work of Mr. Louis Coupal, biostatistician at the Centre Hospitalier de l’Université de Montréal (CHUM). We are indebted to Hélène L’Archevêque and Martine Gauthier for their precious collaboration to this project. FR holds a scholarship from la Société québécoise d’hypertension artérielle.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Rights and permissions
About this article
Cite this article
Rinfret, F., Ouattara, F., Cloutier, L. et al. The impact of unrecorded readings on the precision and diagnostic performance of home blood pressure monitoring: a statistical study. J Hum Hypertens 32, 197–202 (2018). https://doi.org/10.1038/s41371-018-0040-7
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41371-018-0040-7
This article is cited by
-
Number and timing of ambulatory blood pressure monitoring measurements
Hypertension Research (2021)