Abstract
Background
There is a paucity of data comparing 30-day morbidity and mortality of sleeve gastrectomy (SG), Roux-en-Y gastric bypass (RYGB), and one anastomosis gastric bypass (OAGB). This study aimed to compare the 30-day safety of SG, RYGB, and OAGB in propensity score-matched cohorts.
Materials and methods
This analysis utilised data collected from the GENEVA study which was a multicentre observational cohort study of bariatric and metabolic surgery (BMS) in 185 centres across 42 countries between 01/05/2022 and 31/10/2020 during the Coronavirus Disease-2019 (COVID-19) pandemic. 30-day complications were categorised according to the Clavien–Dindo classification. Patients receiving SG, RYGB, or OAGB were propensity-matched according to baseline characteristics and 30-day complications were compared between groups.
Results
In total, 6770 patients (SG 3983; OAGB 702; RYGB 2085) were included in this analysis. Prior to matching, RYGB was associated with highest 30-day complication rate (SG 5.8%; OAGB 7.5%; RYGB 8.0% (p = 0.006)). On multivariate regression modelling, Insulin-dependent type 2 diabetes mellitus and hypercholesterolaemia were associated with increased 30-day complications. Being a non-smoker was associated with reduced complication rates. When compared to SG as a reference category, RYGB, but not OAGB, was associated with an increased rate of 30-day complications. A total of 702 pairs of SG and OAGB were propensity score-matched. The complication rate in the SG group was 7.3% (n = 51) as compared to 7.5% (n = 53) in the OAGB group (p = 0.68). Similarly, 2085 pairs of SG and RYGB were propensity score-matched. The complication rate in the SG group was 6.1% (n = 127) as compared to 7.9% (n = 166) in the RYGB group (p = 0.09). And, 702 pairs of OAGB and RYGB were matched. The complication rate in both groups was the same at 7.5 % (n = 53; p = 0.07).
Conclusions
This global study found no significant difference in the 30-day morbidity and mortality of SG, RYGB, and OAGB in propensity score-matched cohorts.
Similar content being viewed by others
Introduction
Sleeve gastrectomy (SG), Roux-en-Y gastric bypass (RYGB), and one anastomosis gastric bypass (OAGB) are the three commonest bariatric procedures worldwide [1]. There is currently no randomised controlled trial (RCT) comparing these three procedures in the scientific literature. There are several RCTs comparing two of these three procedures [2, 3] but they were not powered to evaluate differences in morbidity or mortality.
30-day morbidity and mortality is a recognised outcome measure for the evaluation of surgical safety and has been used in surgical literature for several decades [4]. There are large studies comparing 30-day morbidity and mortality of RYGB and SG. Alizadeh et al. [5] reported from an analysis of Metabolic and Bariatric Surgery Accreditation and Quality Improvement Program (MBSAQIP) data in the United States that RYGB was associated with higher 30-day morbidity (4.4% vs 2.3%; adjusted odds ratio (AOR) 0.53; p < 0.01) and 30-day mortality (0.2% vs 0.1%; AOR 0.58; p = 0.07) in comparison with SG. However, there is no large data in the scientific literature comparing 30-day morbidity and mortality of SG and OAGB or RYGB and OAGB.
Notwithstanding the lack of such large data, these direct database comparisons are often flawed due to significant differences in the baseline population. Propensity score matching is a valid tool for comparing non-randomised populations by matching them for confounding variables [6]. To the best of our knowledge, there is only one published study comparing 30-day morbidity and mortality of SG and RYGB [7]; and one comparing RYGB and OAGB [8] in propensity score-matched populations. Both of these studies emanate from the MBSAQIP database. In their study, Kapur et al. [7] found lower adverse events with SG in comparison with RYGB. However, the study by Docimo et al. [8] comparing the 30-day morbidity of OAGB and RYGB had too few patients to be meaningful. It is probably because the MBSAQIP database is not likely to have large numbers of OAGB, a procedure not endorsed by the American Society for Metabolic and Bariatric Surgery.
Global 30-day outcomes after bariatric surgEry duriNg thE COVID-19 pAndemic (GENEVA) study [9] is a large, multinational, observational study evaluating 30-day morbidity and mortality of bariatric and metabolic surgery (BMS) during the Coronavirus Disease-2019 (COVID-19) pandemic. The global reach of the study, a large number of patients, and significant numbers of OAGB procedures submitted to this study present a unique opportunity to compare 30-day morbidity and mortality of SG, OAGB, and RYGB in propensity score-matched cohorts.
Methods
Study design and population
The GENEVA study is an international, multicentre, observational cohort study of BMS performed between 1/05/2020 and 31/10/2020 [9]. The current study included all consecutive patients who underwent a primary SG or RYGB or OAGB during this period. Detailed methods have been published previously [9,10,11]. Data collection included patients’ demographics, details of surgery performed, and in-hospital as well as 30-day morbidity and mortality. Complications were categorised using the Clavien–Dindo (CD) Classification system for reporting surgical complications [12].
Statistical methods
Only patients with a complete data entry were included in the analysis. Continuous data were presented as median and interquartile range. Frequencies were used to summarise categorical variables. To examine differences between the three individual procedure types, the Fisher’s exact test was used for categorical variables and Kruskal–Wallis analysis of variance testing for continuous variables.
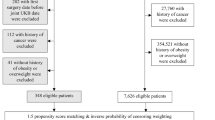
Propensity score matching was completed in a step-wise fashion. Pairwise propensity matching was performed to robustly assess the quality of matching. Standardized mean difference (SMD) was used statistic to examine the balance of covariate distribution between treatment groups. Patients were matched using the following features: sex, Type 2 diabetes mellitus (T2DM) status (No diabetes; diet controlled; oral hypoglycaemics; insulin therapy), hypertension, hypercholesterolaemia, obstructive sleep apnoea, smoking status, age, and baseline body mass index (BMI).
The patients were matched against individuals that had other surgeries using the “nearest” method which utilises a greedy search to match each sample with their nearest neighbour. The distance was calculated using the Mahalanobis distance, which estimates the distribution closest for each point [13]. This procedure was performed in R (R Core Team 2021) using the Matchlt package [14, 15]. The outcome variable was the presence of a complication at 30-days follow-up.
Multivariate analysis was performed to strengthen the resulting statistics from univariate analysis, correcting the influence of each variable on the outcome measured. Multivariate models were created using all the variables used for propensity score matching plus ethnicity (white ethnicity vs other ethnic groups), presence of any co-morbidity, and other unspecified co-morbidity (other than those listed above). Patients were then analysed using a generalised linear model in R (R Core Team 2021) [14].
Results
A total of 470 surgeons from 179 centres in 42 countries submitted data on 7092 adult patients who underwent primary BMS between 1st May 2020 and 31st October 2020 at the participating centres. Of these, complete 30-day morbidity and mortality data were available for 7084 (99.88%) by the 10th of December 2020.
Basic demographics
Of the 7084 patients, 300 patients underwent other procedures and were excluded. A further 14 patients were excluded due to missing values. Complete data were available for a total of 6,770 patients who underwent a primary SG or RYGB or OAGB (SG n = 3983; RYGB n = 2085, OAGB n = 702). Demographic details for all the patients, who underwent any of these three primary procedures are included in Table 1. There were multiple significant differences in baseline demographics between the three groups as detailed in Table 1. RYGB patients were significantly older than patients in the other two cohorts while patients receiving OAGB were more likely to suffer from co-morbidities (Table 1). Patients undergoing SG had the lowest rate of each of these co-morbidities as detailed in Table 1.
30-day morbidity and mortality in the full cohort (unmatched; Table 2)
The overall complication rate was 6.7% (452/6770) (Table 2). RYGB patients had the highest rate of any complication during the 30-day follow-up (8.0% with RYGB vs 7.5% for OAGB and 5.8% for SG (p = 0.006)). There were seven post-operative mortalities (0.1%) (4 with SG, 3 with OAGB, and nil with RYGB; p = 0.016; Fisher’s exact test).
Multivariate analysis of unmatched cohort (Table 3)
On multivariate regression modelling, insulin-dependent T2DM (OR 1.047; 95% CI 1.011–1.083), and hypercholesterolaemia (OR 1.024; 95% CI 1.009–1.040) (Table 3 and Fig. 1) were associated with increased 30-day complications. Being a non-smoker was associated with reduced complication rates (OR 0.984; 95% CI 0.971–0.998). When compared to SG as the reference category, RYGB, but not OAGB, was associated with an increased rate of 30-day complications (OR 1.018; 95% CI 1.005–1.032 for RYGB and OR 1.009; 95% CI 0.989–1.030 for OAGB).
30-day morbidity and mortality in the propensity score-matched cohort (Tables 4–6)
SG vs OAGB
In total, 702 pairs were matched with a reduction in SMDs for all matched variables (8/8) (Table 4). The overall complication rate in the SG group was 51 (7.3%) as compared to 53 (7.5%) in the OAGB group (Table 7). The difference was not significant (p = 0.68).
SG vs RYGB
In total, 2085 pairs were matched with a reduction in SMDs for seven of the eight matched variables (Table 5). The overall complication rate in the SG group was 127 (6.1%) as compared to 166 (7.9%) in the RYGB group (Table 7). The difference was not significant (p = 0.09).
OAGB vs RYGB
In total, 702 pairs were matched with a reduction in SMDs in four of the eight matched variables (4/8) (Table 6). The overall complication rate in both the groups was the same 53 (7.5%; p = 0.07; Table 7).
Discussion
This study shows that there is no significant difference in 30-day morbidity and mortality of SG, RYGB, and OAGB in propensity score-matched cohorts from a large, global dataset collected during the COVID-19 pandemic. Though RYGB was associated with higher 30-day morbidity in comparison with reference SG (OR 1.018; 95% CI 1.005–1.032) in the unmatched cohort on multivariate analysis, the difference disappeared after propensity score matching (p = 0.09). In comparison, OAGB was not associated with higher 30-day morbidity in comparison with SG on either multivariate analysis (OR 1.009; 95% CI 0.989–1.030) or propensity score-matched comparison (p = 0.68).
RCTs comparing different bariatric procedures often have weight loss [2] or diabetes control [16] as their endpoints. Some [16] do not even clearly report 30-day morbidity and mortality with different bariatric procedures let alone classifying surgical complications adequately according to the widely used and accepted CD Classification [12]. We cannot, therefore, derive any scientifically valid conclusions regarding complication rates of different procedures from these RCTs.
Outside of RCTs, perceptions regarding relative safety and efficacy of different procedures for different patient groups may introduce potential bias. For example, in this study, we found 33.0% of patients undergoing OAGB were suffering from T2DM compared to 23.0% undergoing RYGB and 16.0% undergoing SG in the unmatched cohorts. This selection bias may be partly accounted for by fact that the randomised studies have shown superior (non-significant as they were not powered to evaluate these) outcomes in terms of diabetes improvement with OAGB in comparison with RYGB [2] and with RYGB in comparison with SG [17]. This is important because T2DM is known to be associated with complications after bariatric surgery [18, 19] and in our study, Insulin-dependent T2DM was independently associated with 30-day morbidity on multivariate analysis of the unmatched cohort.
Similarly, in the unmatched cohort, hypercholesterolaemia was present in 19.0% of patients undergoing SG in comparison with 32.0% of those undergoing OAGB and 23.0% of those undergoing RYGB. However, after matching, in the analysis of SG and OAGB, the hypercholesterolaemia rates in the two groups were the same at 32.0 and 23.0% in the analysis of SG and RYGB. This is also important because hypercholesterolaemia was independently associated with 30-day morbidity on multivariate analysis of the unmatched data and differences in hypercholesterolaemia rates in the unmatched cohort may well have accounted for some of the observed differences in 30-day morbidity. Others [20] have also found dyslipidaemia to be a predictor of complication after bariatric surgery.
Standardised mean differences in age, BMI, sex, smoking status, hypertension rates all reduced after matching for both the matched comparisons involving SG in this study. Given that all of these characteristics are known to be associated with increased morbidity after bariatric surgery [21,22,23,24,25,26,27,28,29], differences in these baseline characteristics may have been in part responsible for why the observed difference in morbidity between SG and RYGB or OAGB disappeared after matching. At the same time, and probably because of the fewer number of bypass procedures in the GENEVA database, matching failed to reduce SMDs for age, sex, smoking status, and hypertension in the comparison between OAGB and RYGB in this study. This may partly account for the observed lack of difference in 30-day morbidity between the two procedures. Future studies on this topic need to be mindful of this.
There is no published study comparing the 30-day morbidity of SG with that of OAGB in propensity score-matched cohorts. This may be due to continued reservations [30] amongst some surgeons about OAGB. Furthermore, and as mentioned above in the Introduction section, there is only one propensity score-matched study [8] in the scientific literature comparing the 30-day safety of OAGB with that of any other procedure (RYGB in this case) and that study only had 279 pairs of OAGB and RYGB. One could argue this is not a large enough sample to study differences in morbidity.
There is only one study [7] in the published literature comparing the 30-day morbidity of SG with that of RYGB. Interestingly that study showed lower complication rates with SG in contrast to our findings. It is however worth noting that these authors do not report standardised mean difference in propensity score-matched populations and given the large numbers matched, it was inevitable that their matching was not perfect with significant difference between the matched populations with regards to important confounding variables such as age, BMI, smoking, insulin-dependent T2DM, etc.
This study represents the first large propensity-matched comparison of 30-day morbidity and mortality of SG, RYGB, and OAGB. This data was collected from a large worldwide collaborative study of real-world bariatric surgical practice. Data completion rates were extremely high with 30-day follow data available for 97.9% of patients across the entire cohort and this represents a significant strength of this study.
Non-randomised design and self-reported complication rates are two major weaknesses of this study. However, it is not easy to randomise to different procedures with 30-day morbidity as an endpoint and anonymous data collection strategy used in this study may have diminished the desire to under-report complications. Another weakness of this study is that differences in complication rates, though statistically not significant, maybe clinically relevant. Indeed, larger studies may even find statistical significance.
Conclusion
The present analysis shows that there is no significant difference in 30-day morbidity and mortality of SG, OAGB, and RYGB in propensity-matched cohorts.
References
Angrisani L, Santonicola A, Iovino P, Ramos A, Shikora S, Kow L. Bariatric surgery survey 2018: similarities and disparities among the 5 IFSO chapters. Obes Surg.2021;31:1937–48. https://doi.org/10.1007/s11695-020-05207-7.
Robert M, Espalieu P, Pelascini E, Caiazzo R, Sterkers A, Khamphommala L, et al. Efficacy and safety of one anastomosis gastric bypass versus Roux-en-Y gastric bypass for obesity (YOMEGA): a multicentre, randomised, open-label, non-inferiority trial. Lancet. 2019;393:1299–309. https://doi.org/10.1016/s0140-6736(19)30475-1.
Salminen P, Helmiö M, Ovaska J, Juuti A, Leivonen M, Peromaa-Haavisto P, et al. Effect of laparoscopic sleeve gastrectomy vs laparoscopic Roux-en-Y gastric bypass on weight loss at 5 years among patients with morbid obesity: the SLEEVEPASS randomized clinical trial. JAMA. 2018;319:241–54. https://doi.org/10.1001/jama.2017.20313.
Okike N, Payne WS, Neufeld DM, Bernatz PE, Pairolero PC, Sanderson DR. Esophagomyotomy versus forceful dilation for achalasia of the esophagus: results in 899 patients. Ann Thorac Surg. 1979;28:119–25. https://doi.org/10.1016/s0003-4975(10)63767-8.
Alizadeh RF, Li S, Gambhir S, Hinojosa MW, Smith BR, Stamos MJ, et al. Laparoscopic sleeve gastrectomy or laparoscopic gastric bypass for patients with metabolic syndrome: an MBSAQIP analysis. Am Surg. 2019;85:1108–12.
Robins JM, Mark SD, Newey WK. Estimating exposure effects by modelling the expectation of exposure conditional on confounders. Biometrics. 1992;48:479–95.
Kapur A, Thodiyil P. Primary laparoscopic sleeve gastrectomy versus gastric bypass: a propensity-matched comparison of 30-day outcomes. Surg Obes Relat Dis. 2021;17:1369–82. https://doi.org/10.1016/j.soard.2021.01.022.
Docimo S, Yang J, Zhang X, Pryor A, Spaniolas K. One anastomosis gastric bypass versus Roux-en-Y gastric bypass: a 30-day follow-up review. Surg Endosc. 2021. https://doi.org/10.1007/s00464-021-08309-0.
Singhal R, Tahrani AA, Ludwig C, Mahawar K. Global 30-day outcomes after bariatric surgery during the COVID-19 pandemic (GENEVA): an international cohort study. Lancet Diabetes Endocrinol. 2021;9:7–9. https://doi.org/10.1016/s2213-8587(20)30375-2.
Singhal R, Ludwig C, Rudge G, Gkoutos GV, Tahrani A, Mahawar K, et al. 30-day morbidity and mortality of bariatric surgery during the COVID-19 pandemic: a multinational cohort study of 7704 patients from 42 countries. Obes Surg. 2021:1–17. https://doi.org/10.1007/s11695-021-05493-9.
Singhal R, Wiggins T, Super J, Alqahtani A, Nadler EP, Ludwig C, et al. 30-day morbidity and mortality of bariatric metabolic surgery in adolescence during the COVID-19 pandemic—the GENEVA study. Pediatr Obes. 2021:e12832. https://doi.org/10.1111/ijpo.12832.
Dindo D, Demartines N, Clavien PA. Classification of surgical complications: a new proposal with evaluation in a cohort of 6336 patients and results of a survey. Ann Surg. 2004;240:205–13. https://doi.org/10.1097/01.sla.0000133083.54934.ae.
Chandra, M. On the generalized distance in statistics. In: Proceedings of the National Institute of Science, India. 2021. Available from: https://www.scienceopen.com/document?vid=a553c5c9-9837-4568-9f20-91a3f1ca1879.
R Core Team. R: A language and environment for statistical computing. R Foundation for Statistical Computing, Vienna, Austria. 2019. https://www.R-project.org/.
Stuart EA, King G, Imai K, Ho D. MatchIt: Nonparametric Preprocessing for Parametric Causal Inference. J Stat Softw. 2011;42:28. https://doi.org/10.18637/jss.v042.i08.
Schauer PR, Kashyap SR, Wolski K, Brethauer SA, Kirwan JP, Pothier CE, et al. Bariatric surgery versus intensive medical therapy in obese patients with diabetes. N Engl J Med. 2012;366:1567–76. https://doi.org/10.1056/NEJMoa1200225.
Sharples AJ, Mahawar K. Systematic review and meta-analysis of randomised controlled trials comparing long-term outcomes of Roux-En-Y gastric bypass and sleeve gastrectomy. Obes Surg. 2020;30:664–72. https://doi.org/10.1007/s11695-019-04235-2.
Buchwald H, Estok R, Fahrbach K, Banel D, Sledge I. Trends in mortality in bariatric surgery: a systematic review and meta-analysis. Surgery. 2007;142:621–35.
Keidar A. Bariatric surgery for type 2 diabetes reversal: the risks. Diabetes Care. 2011;34:S361–S266.
Coblijn UK, Karres J, de Raaff CAL, de Castro SMM, Lagarde SM, van Tets WF, et al. Predicting postoperative complications after bariatric surgery: the Bariatric Surgery Index for Complications, BASIC. Surg Endosc. 2017;31:4438–45. https://doi.org/10.1007/s00464-017-5494-0.
Nickel F, de la Garza JR, Werthmann FS, Benner L, Tapking C, Karadza E, et al. Predictors of risk and success of obesity surgery. Obes Facts. 2019;12:427–39. https://doi.org/10.1159/000496939.
Qin C, Luo B, Aggarwal A, De Oliveira G, Kim JY. Advanced age as an independent predictor of perioperative risk after laparoscopic sleeve gastrectomy (LSG). Obes Surg. 2015;25:406–12. https://doi.org/10.1007/s11695-014-1462-0.
Mocanu V, Dang JT, Switzer N, Madsen K, Birch DW, Karmali S. Sex and race predict adverse outcomes following bariatric surgery: an MBSAQIP analysis. Obes Surg. 2020;30:1093–101. https://doi.org/10.1007/s11695-020-04395-6.
Husain F, Jeong IH, Spight D, Wolfe B, Mattar SG. Risk factors for early postoperative complications after bariatric surgery. Ann Surg Treat Res. 2018;95:100–10. https://doi.org/10.4174/astr.2018.95.2.100.
Vanw MR, Smulders FJ, Luyer MD, Vanm G, Vanhimbeeck FJ, Nienhuijs SW. Predictors for the occurrence of major complications after primary Roux-en-Y gastric bypass surgery. Minerva Chir. 2016;71:286–92.
Dayer-Jankechova A, Fournier P, Allemann P, Suter M. Complications after laparoscopic Roux-en-Y gastric bypass in 1573 consecutive patients: are there predictors? Obes Surg. 2016;26:12–20. https://doi.org/10.1007/s11695-015-1752-1.
Abraham CR, Werter CR, Ata A, Hazimeh YM, Shah US, Bhakta A, et al. Predictors of hospital readmission after bariatric surgery. J Am Coll Surg. 2015;221:220–7. https://doi.org/10.1016/j.jamcollsurg.2015.02.018.
Janik MR, Aryaie AH. The effect of smoking on bariatric surgical 30-day outcomes: propensity-score-matched analysis of the MBSAQIP. Surg Endosc. 2021;35:3905–14. https://doi.org/10.1007/s00464-020-07838-4.
Falvo A, Vacharathit V, Kuhn JE, Fluck M, Cunningham RM, Petrick AT, et al. Comparison of short-term outcomes following Roux-en-Y gastric bypass in male and female patients using the MBSAQIP database. Surg Obes Relat Dis. 2020;16:1236–41. https://doi.org/10.1016/j.soard.2020.04.045.
Parikh M, Eisenberg D, Johnson J, El-Chaar M. American Society for Metabolic and Bariatric Surgery review of the literature on one-anastomosis gastric bypass. Surg Obes Relat Dis. 2018;14:1088–92. https://doi.org/10.1016/j.soard.2018.04.017.
Funding
This study is funded by Bariatric Unit, University Hospital Birmingham NHS Foundation Trust.
Author information
Authors and Affiliations
Consortia
Contributions
Conceptualisation: RS and KM. Data curation: RS, TW, and JS. Data analysis: VRC, GVG, and CL. Tables and figures: RS, VRC, and CL. Manuscript writing and proof reading: all authors.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
A full list of author affiliations appears at the end of the paper.
Supplementary information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Singhal, R., Cardoso, V.R., Wiggins, T. et al. 30-day morbidity and mortality of sleeve gastrectomy, Roux-en-Y gastric bypass and one anastomosis gastric bypass: a propensity score-matched analysis of the GENEVA data. Int J Obes 46, 750–757 (2022). https://doi.org/10.1038/s41366-021-01048-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41366-021-01048-1
This article is cited by
-
Effect of different bariatric surgery methods on metabolic syndrome in patients with severe obesity
Updates in Surgery (2024)
-
Jejunal stenosis as a sequela after laparoscopic sleeve gastrectomy for morbid obesity: a case series
Updates in Surgery (2024)
-
A Prospective Multicenter Standard of Care Study of Outpatient Laparoscopic Sleeve Gastrectomy
Obesity Surgery (2024)
-
Experience of Robotic Complex Revisional Bariatric Surgery in a High-Volume Center
Obesity Surgery (2023)
-
Comparison of Single Versus Double Anastomosis Bariatric Metabolic Surgery in Obesity: a Systematic Review and Meta-analysis
Obesity Surgery (2023)