Abstract
Background
Elderly patients undergo bariatric surgery less frequently than younger patients. Short- and medium-term outcomes after bariatric surgery in the elderly population remain largely unknown. The objective of the present retrospective, registry-based cohort study was to compare short- and medium-term outcomes between patients <65 and ≥65 years undergoing bariatric surgery, hypothesizing similar outcomes between groups.
Methods
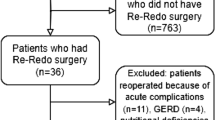
In this retrospective, registry-based cohort study, the Ontario Bariatric Registry was used to compare data of patients <65 and ≥65 years who underwent Roux-en-Y gastric bypass and sleeve gastrectomy between January 2010 and August 2019 in all accredited bariatric centers of excellence in Ontario, Canada. Primary outcomes were overall postoperative complications. Secondary outcomes included early (<30 days) complications, readmissions, reoperations, mortality, weight loss and comorbidities improvement at 1 and 3 year after surgery.
Results
Data of 22,981 patients <65 and 532 patients ≥65 years were analyzed. Overall postoperative complications were similar between patients <65 and ≥65 years (3388/22,981 [14.7%] vs. 73/532 [13.7%], p = 0.537). Early (<30 days) postoperative complications, readmissions, reoperations, and mortality rates were also similar between groups. Both groups had significant weight loss and comorbidities improvement at 1- and 3-year follow-up. Patients <65 years had superior weight loss (+3.5%, 95% CI: 1.6–5.4, p < 0.001) and higher rates of remission for diabetes mellitus (63.8% vs. 39.3%, p < 0.001), hypertension (37.9% vs. 14.5%, p < 0.001), dyslipidemia (28.2% vs. 9.5%, p < 0.001) and gastroesophageal reflux (65.1% vs. 24.0 %, p < 0.001) compared to patients ≥65 years at 3 year.
Conclusions
Patients <65 and ≥65 years had similar perioperative morbidity and mortality after bariatric surgery. Even though patients <65 years had overall better medium-term outcomes, bariatric surgery is safe and yields significant weight loss and comorbidities improvement in patients ≥65 years.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout
Similar content being viewed by others
References
NCD Risk Factor Collaboration (NCD-RisC). Worldwide trends in body-mass index, underweight, overweight, and obesity from 1975 to 2016: a pooled analysis of 2416 population-based measurement studies in 128·9 million children, adolescents, and adults. Lancet. 2017;390:2627–42.
The Organisation for Economic Co-operation and Development (OECD), Obesity Update 2017. Available at: http://www.oecd.org/health/obesity-update.htm. Accessed August 20, 2021.
Buchwald H. Consensus conference panel. Consensus conference statement bariatric surgery for morbid obesity: health implications for patients, health professionals, and third-party payers. Surg Obes Relat Dis. 2005;1:371–81.
Sjöström L, Narbro K, Sjöström CD, Karason K, Larsson B, Wedel H, et al. Effects of bariatric surgery on mortality in Swedish obese subjects. N Engl J Med. 2007;357:741–52.
English WJ, DeMaria EJ, Hutter MM, Kothari SN, Mattar SG, Brethauer SA, et al. American Society for Metabolic and Bariatric Surgery 2018 estimate of metabolic and bariatric procedures performed in the United States. Surg Obes Relat Dis. 2020;16:457–63.
Angrisani L, Santonicola A, Iovino P, Vitiello A, Higa K, Himpens J, et al. IFSO Worldwide Survey 2016: primary, endoluminal, and revisional procedures. Obes Surg. 2018;28:3783–94.
The World Bank Data, Population age 65 and above. Available at: https://data.worldbank.org/indicator/SP.POP.65UP.TO.ZS?name_desc=false. Accessed August 20, 2021.
Varela JE, Wilson SE, Nguyen NT. Outcomes of bariatric surgery in the elderly. Am Surg. 2006;72:865–9.
Koh CY, Inaba CS, Sujatha-Bhaskar S, Nguyen NT. Outcomes of laparoscopic bariatric surgery in the elderly population. Am Surg. 2018;84:1600–03.
Susmallian S, Barnea R, Weiss Y, Raziel A. Outcome of bariatric surgery in older patients. Surg Obes Relat Dis. 2018;14:1705–13.
Prasad J, Vogels E, Dove JT, Wood C, Petrick AT, Parker DM. Is age a real or perceived discriminator for bariatric surgery? A long-term analysis of bariatric surgery in the elderly. Surg Obes Relat Dis. 2019;15:725–31.
Vinan-Vega M, Diaz Vico T, Elli EF. Bariatric surgery in the elderly patient: safety and short-time outcome. a case match Analysis. Obes Surg. 2019;29:1007–11.
Kaplan U, Penner S, Farrokhyar F, Andruszkiewicz N, Breau R, Gmora S, et al. Bariatric surgery in the elderly is associated with similar surgical risks and significant long-term health benefits. Obes Surg. 2018;28:2165–70.
United Nations, Global issues: Ageing. Available at: https://www.un.org/en/sections/issues-depth/ageing/. Accessed August 20, 2021.
The Organisation for Economic Co-operation and Development (OECD), Pensions at a Glance 2019. Available at: https://www.oecd-ilibrary.org/fr/social-issues-migration-health/pensions-at-a-glance-2019_b6d3dcfc-en/. Accessed August 20, 2021.
Chung S, Domino ME, Stearns SC, Popkin BM. Retirement and physical activity: analyses by occupation and wealth. Am J Prev Med. 2009;36:422–8.
Chung S, Domino ME, Stearns SC. The effect of retirement on weight. J Gerontol B Psychol Sci Soc Sci. 2009;64:656–65.
Godard M. Gaining weight through retirement? Results from the SHARE survey. J Health Econ. 2016;;45:27–46.
Brethauer SA, Kim J, el Chaar M, Papasavas P, Eisenberg D, Rogers A, et al. Standardized outcomes reporting in metabolic and bariatric surgery. Surg Obes Relat Dis. 2015;11:489–506.
Ramirez A, Roy M, Hidalgo JE, Szomstein S, Rosenthal RJ. Outcomes of bariatric surgery in patients >70 years old. Surg Obes Relat Dis. 2012;8:458–62.
Loy JJ, Youn HA, Schwack B, Kurian MS, Fielding GA, Ren-Fielding CJ. Safety and efficacy of laparoscopic adjustable gastric banding in patients aged seventy and older. Surg Obes Relat Dis. 2014;10:284–9.
Wittgrove AC, Martinez T. Laparoscopic gastric bypass in patients 60 years and older: early postoperative morbidity and resolution of comorbidities. Obes Surg. 2009;19:1472–76.
Clough A, Layani L, Shah A, Wheatley L, Taylor C. Laparoscopic gastric banding in over 60s. Obes Surg. 2011;21:10–17.
The Ontario Ministry of Health and Long-Term Care, Ontario Health Insurance Plan (OHIP)—Physician Services— Schedule of Fees from July 2, 2021 (effective October 1, 2021). Available at https://www.health.gov.on.ca/en/pro/programs/ohip/sob/. Accessed October 23, 2021.
Zellmer JD, Mathiason MA, Kallies KJ, Kothari SN. Is laparoscopic sleeve gastrectomy a lower risk bariatric procedure compared with laparoscopic Roux-en-Y gastric bypass? A meta-analysis. Am J Surg. 2014;208:903–10.
Boza C, Gamboa C, Salinas J, Achurra P, Vega A, Pérez G. Laparoscopic Roux-en-Y gastric bypass versus laparoscopic sleeve gastrectomy: a case-control study and 3 years of follow-up. Surg Obes Relat Dis. 2012;8:243–9.
St-Onge MP, Gallagher D. Body composition changes with aging: the cause or the result of alterations in metabolic rate and macronutrient oxidation? Nutrition. 2010;26:152–5.
Reinders I, Visser M, Schaap L. Body weight and body composition in old age and their relationship with frailty. Curr Opin Clin Nutr Metab Care. 2017;20:11–15.
Villareal DT, Chode S, Parimi N, Sinacore DR, Hilton T, Armamento-Villareal R, et al. Weight loss, exercise, or both and physical function in obese older adults. N Engl J Med. 2011;364:1218–29.
Svetkey LP, Stevens VJ, Brantley PJ, Appel LJ, Hollis JF, Loria CM, et al. Comparison of strategies for sustaining weight loss: the weight loss maintenance randomized controlled trial. JAMA. 2008;299:1139–48.
Coughlin JW, Brantley PJ, Champagne CM, Vollmer WM, Stevens VJ, Funk K, et al. The impact of continued intervention on weight: Five-year results from the weight loss maintenance trial. Obesity (Silver Spring). 2016;24:1046–1053.
Organisation for Economic Co-operation and Development (OECD), Life expectancy at birth. Available at: https://data.oecd.org/healthstat/life-expectancy-at-birth.htm/. Accessed August 20, 2021.
Sanderson WC, Scherbov S. Choosing between the UN’s alternative views of population aging. PLoS One. 2020;15:e0233602.
Sanderson WC, Scherbov S (eds). Prospective Longevity: A New Vision of Population Aging. Cambridge, MA, USA: Harvard University Press; 2019.
Arterburn DE, Olsen MK, Smith VA, Livingston EH, Van Scoyoc L, Yancy WS Jr, et al. Association between bariatric surgery and long-term survival. JAMA. 2015;313:62–70.
Poole NA, Al Atar A, Kuhanendran D, Bidlake L, Fiennes A, McCluskey S, et al. Compliance with surgical after-care following bariatric surgery for morbid obesity: a retrospective study. Obes Surg. 2005;15:261–5.
Author information
Authors and Affiliations
Contributions
PI: principal investigator—design and conception of the study, data collection, data analysis, interpretation of data, manuscript drafting. VB: design and conception of the study, interpretation of data, critical revision for important intellectual content. KR: interpretation of data, critical revision for important intellectual content. KB: data collection, data analysis, interpretation of data, critical revision for important intellectual content. OL: data collection, interpretation of data, critical revision for important intellectual content. MA: design and conception of the study, interpretation of data, critical revision for important intellectual content. All authors approve the final version of the manuscript to be published and all authors agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. All authors fulfill the four ICMJE criteria for authorship.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
About this article
Cite this article
Iranmanesh, P., Boudreau, V., Ramji, K. et al. Outcomes of bariatric surgery in elderly patients: a registry-based cohort study with 3-year follow-up. Int J Obes 46, 574–580 (2022). https://doi.org/10.1038/s41366-021-01031-w
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41366-021-01031-w
This article is cited by
-
Early outcomes of one-anastomosis gastric bypass in the elderly population at high-volume bariatric centers
Updates in Surgery (2024)
-
Bariatric Surgery Should Be Proposed in Certain Septuagenarian Patients with Obesity
Obesity Surgery (2023)