Abstract
Background
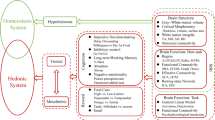
High body mass index (BMI) is associated with neurocognitive impairments that contribute to overeating and interfere with weight loss efforts. Overweight and obesity at midlife can accelerate neurodegenerative changes and increase the risk of late-life dementia. Noninvasive neuromodulation represents a novel, affordable and scalable approach to improve neurocognitive function in this context. The purpose of this proof-of-concept study was to examine whether transcranial direct current stimulation (tDCS) aimed at enhancing prefrontal cortex activity could enhance weight loss, in combination with a hypocaloric diet, and study underlying mechanisms.
Methods
Overall, 38 women with BMI 25–35 kg/m2 underwent a 4 week randomized, double-blinded, sham-controlled, and parallel-design intervention, during which they received eight sessions of tDCS (n = 18 sham, n = 20 active) in combination with a diet (caloric goal of 20 kcal/kg/day). We evaluated longitudinal changes in body weight, appetite and food craving. In addition, we examined the contribution of cognitive-executive processes via food-modified computerized tasks.
Results
We found that the active group had more reduction in body weight than the sham group throughout the study (p = 0.020) and significant weekly weight loss. At 4 weeks, the active group lost 2.32% of initial body weight (sham: 1.29%). Components of subjective appetite and food craving showed a trend toward more reduction in the active group. These changes were paralleled by significant improvements in task performance in the active group, particularly in a dual task that required inhibitory control and working memory (p = 0.007–0.031). Improvement in inhibitory control performance predicted reduction in lack of control overeating, explaining 43.5% of its variance at the end of the study (p = 0.003). No significant adverse effects were observed.
Conclusions
Our results provide proof-of-concept validation of prefrontal-targeted tDCS, combined with a diet, in midlife women with excess body weight, paving the way for larger studies evaluating clinical efficacy and long-term effects of this intervention.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout



Similar content being viewed by others
References
Hales CM, Carroll MD, Fryar CD, Ogden CL. Prevalence of obesity among adults and youth: United States, 2015–2016. Atlanta, GA: Centers for Disease Control and Prevention, National Center for Health Statistics; 2017.
World Health Organization (WHO). Fact sheet: obesity and overweight. https://www.who.int/en/news-room/fact-sheets/detail/obesity-andoverweight. Accessed 14 Nov 2019.
Patterson RE, Frank LL, Kristal AR, White E. A comprehensive examination of health conditions associated with obesity in older adults. Am J Prev Med. 2004;27:385–90.
Pi-Sunyer FX. Medical hazards of obesity. Ann Intern Med. 1993;119:655–60.
Hammond RA, Levine R. The economic impact of obesity in the United States. Diabetes Metab Syndr Obes Targets Ther. 2010;3:285–95.
Dobbs R, Sawers C, Thompson F, Manyika J, Woetzel J, Child P, et al. Overcoming obesity: an initial economic analysis. Discussion paper. London, UK, McKinsey Global Institute, McKinsey & Company; 2014.
Kivipelto M, Ngandu T, Fratiglioni L, Viitanen M, Kåreholt I, Winblad B, et al. Obesity and vascular risk factors at midlife and the risk of dementia and Alzheimer disease. Arch Neurol. 2005;62:1556–60.
Emmerzaal TL, Kiliaan AJ, Gustafson DR. 2003-2013: a decade of body mass index, Alzheimer’s disease, and dementia. J Alzheimers Dis JAD. 2015;43:739–55.
Xu WL, Atti AR, Gatz M, Pedersen NL, Johansson B, Fratiglioni L. Midlife overweight and obesity increase late-life dementia risk: a population-based twin study. Neurology. 2011;76:1568–74.
Mattson MP. An evolutionary perspective on why food overconsumption impairs cognition. Trends Cogn Sci. 2019;23:200–12.
Bocarsly ME, Fasolino M, Kane GA, LaMarca EA, Kirschen GW, Karatsoreos IN, et al. Obesity diminishes synaptic markers, alters microglial morphology, and impairs cognitive function. Proc Natl Acad Sci USA. 2015;112:15731–6.
Wing RR, Phelan S. Long-term weight loss maintenance. Am J Clin Nutr. 2005;82:222S–225S.
Forcano L, Mata F, de la Torre R, Verdejo-Garcia A. Cognitive and neuromodulation strategies for unhealthy eating and obesity: Systematic review and discussion of neurocognitive mechanisms. Neurosci Biobehav Rev. 2018;87:161–91.
Val-Laillet D, Aarts E, Weber B, Ferrari M, Quaresima V, Stoeckel LE, et al. Neuroimaging and neuromodulation approaches to study eating behavior and prevent and treat eating disorders and obesity. NeuroImage Clin. 2015;8:1–31.
Neseliler S, Hu W, Larcher K, Zacchia M, Dadar M, Scala SG, et al. Neurocognitive and hormonal correlates of voluntary weight loss in humans. Cell Metabol. 2019;29:39–49.e4.
Gluck ME, Viswanath P, Stinson EJ. Obesity, appetite, and the prefrontal cortex. Curr Obes Rep. 2017;6:380–8.
Lowe CJ, Reichelt AC, Hall PA. The prefrontal cortex and obesity: a health neuroscience perspective. Trends Cogn Sci. 2019. https://doi.org/10.1016/j.tics.2019.01.005.
Vainik U, Baker TE, Dadar M, Zeighami Y, Michaud A, Zhang Y, et al. Neurobehavioral correlates of obesity are largely heritable. Proc Natl Acad Sci USA. 2018;115:9312–7.
Hofmann W, Friese M, Strack F. Impulse and self-control from a dual-systems perspective. Perspect Psychol Sci J Assoc Psychol Sci. 2009;4:162–76.
Hare TA, Camerer CF, Rangel A. Self-control in decision-making involves modulation of the vmPFC valuation system. Science. 2009;324:646–8.
Kober H, Mende-Siedlecki P, Kross EF, Weber J, Mischel W, Hart CL, et al. Prefrontal-striatal pathway underlies cognitive regulation of craving. Proc Natl Acad Sci USA. 2010;107:14811–6.
Wang G-J, Volkow ND, Telang F, Jayne M, Ma Y, Pradhan K, et al. Evidence of gender differences in the ability to inhibit brain activation elicited by food stimulation. Proc Natl Acad Sci USA. 2009;106:1249–54.
DelParigi A, Chen K, Salbe AD, Hill JO, Wing RR, Reiman EM, et al. Successful dieters have increased neural activity in cortical areas involved in the control of behavior. Int J Obes. 2007;31:440–8.
McCaffery JM, Haley AP, Sweet LH, Phelan S, Raynor HA, Del Parigi A, et al. Differential functional magnetic resonance imaging response to food pictures in successful weight-loss maintainers relative to normal-weight and obese controls. Am J Clin Nutr. 2009;90:928–34.
Hassenstab JJ, Sweet LH, Del Parigi A, McCaffery JM, Haley AP, Demos KE, et al. Cortical thickness of the cognitive control network in obesity and successful weight loss maintenance: a preliminary MRI study. Psychiatry Res. 2012;202:77–79.
Weygandt M, Mai K, Dommes E, Leupelt V, Hackmack K, Kahnt T, et al. The role of neural impulse control mechanisms for dietary success in obesity. NeuroImage. 2013;83:669–78.
DSNT Le, Pannacciulli N, Chen K, Del Parigi A, Salbe AD, Reiman EM, et al. Less activation of the left dorsolateral prefrontal cortex in response to a meal: a feature of obesity. Am J Clin Nutr. 2006;84:725–31.
Le DSN, Pannacciulli N, Chen K, Salbe AD, Del Parigi A, Hill JO, et al. Less activation in the left dorsolateral prefrontal cortex in the reanalysis of the response to a meal in obese than in lean women and its association with successful weight loss. Am J Clin Nutr. 2007;86:573–9.
Bikson M, Grossman P, Thomas C, Zannou AL, Jiang J, Adnan T, et al. Safety of transcranial direct current stimulation: evidence based update 2016. Brain Stimulat. 2016;9:641–61.
Nitsche MA, Cohen LG, Wassermann EM, Priori A, Lang N, Antal A, et al. Transcranial direct current stimulation: state of the art 2008. Brain Stimulat. 2008;1:206–23.
Wagner T, Fregni F, Fecteau S, Grodzinsky A, Zahn M, Pascual-Leone A. Transcranial direct current stimulation: a computer-based human model study. NeuroImage. 2007;35:1113–24.
Rahman A, Reato D, Arlotti M, Gasca F, Datta A, Parra LC, et al. Cellular effects of acute direct current stimulation: somatic and synaptic terminal effects. J Physiol. 2013;591:2563–78.
Nitsche MA, Paulus W. Excitability changes induced in the human motor cortex by weak transcranial direct current stimulation. J Physiol. 2000;527:633–9.
Stagg CJ, Nitsche MA. Physiological basis of transcranial direct current stimulation. Neurosci Rev J Bringing Neurobiol Neurol Psychiatry. 2011;17:37–53.
Peña-Gómez C, Sala-Lonch R, Junqué C, Clemente IC, Vidal D, Bargalló N, et al. Modulation of large-scale brain networks by transcranial direct current stimulation evidenced by resting-state functional MRI. Brain Stimulat. 2012;5:252–63.
Fonteneau C, Redoute J, Haesebaert F, Le Bars D, Costes N, Suaud-Chagny M-F, et al. Frontal transcranial direct current stimulation induces dopamine release in the ventral striatum in human. Cereb Cortex. 2018;28:2636–46.
Lefaucheur J-P, Antal A, Ayache SS, Benninger DH, Brunelin J, Cogiamanian F, et al. Evidence-based guidelines on the therapeutic use of transcranial direct current stimulation (tDCS). Clin Neurophysiol Off J Int Fed Clin Neurophysiol. 2017;128:56–92.
Hall PA, Vincent CM, Burhan AM. Non-invasive brain stimulation for food cravings, consumption, and disorders of eating: A review of methods, findings and controversies. Appetite. 2018;124:78–88.
Mostafavi S-A, Khaleghi A, Mohammadi MR, Akhondzadeh S. Is transcranial direct current stimulation an effective modality in reducing food craving? A systematic review and meta-analysis. Nutr Neurosci. 2018:1–13. https://www.tandfonline.com/doi/abs/10.1080/1028415X.2018.1470371?journalCode=ynns20.
Gluck ME, Alonso-Alonso M, Piaggi P, Weise CM, Jumpertz-von Schwartzenberg R, Reinhardt M, et al. Neuromodulation targeted to the prefrontal cortex induces changes in energy intake and weight loss in obesity. Obes Silver Spring Md. 2015;23:2149–56.
Heinitz S, Reinhardt M, Piaggi P, Weise CM, Diaz E, Stinson EJ, et al. Neuromodulation directed at the prefrontal cortex of subjects with obesity reduces snack food intake and hunger in a randomized trial. Am J Clin Nutr. 2017;106:1347–57.
Sedgmond J, Lawrence NS, Verbruggen F, Morrison S, Chambers CD, Adams RC. Prefrontal brain stimulation during food-related inhibition training: effects on food craving, food consumption and inhibitory control. R Soc Open Sci. 2019;6:181186.
Gómez Candela C, Julián Viñals R, Arrebola VIva E, Koester T, Boticario D, Parrado JA, et al. On-line individualized diet program focused on diabetics. Nutr Hospi. 2014;30:11–18.
Gandiga PC, Hummel FC, Cohen LG. Transcranial DC stimulation (tDCS): a tool for double-blind sham-controlled clinical studies in brain stimulation. Clin Neurophysiol Off J Int Fed Clin Neurophysiol. 2006;117:845–50.
Blundell JE, Graaf K, Finlayson G, Halford JCG, Hetherington M, King NA, et al. Measuring food intake, hunger, satiety and satiation in the laboratory. In: Allison DB, Baskin ML, editors. Handbook of assessment methods for eating behaviours and weight-related problems: measures, theory and research. 2nd ed. Newbury Park, California: Sage; 2009. p. 283–325.
Moreno S, Rodríguez S, Fernandez MC, Tamez J, Cepeda-Benito A. Clinical validation of the trait and state versions of the Food Craving Questionnaire. Assessment. 2008;15:375–87.
Jáuregui-Lobera I, García-Cruz P, Carbonero-Carreño R, Magallares A, Ruiz-Prieto I. Psychometric properties of Spanish version of the Three-Factor Eating Questionnaire-R18 (Tfeq-Sp) and its relationship with some eating- and body image-related variables. Nutrients. 2014;6:5619–35.
Batterink L, Yokum S, Stice E. Body mass correlates inversely with inhibitory control in response to food among adolescent girls: an fMRI study. NeuroImage. 2010;52:1696–703.
Blechert J, Meule A, Busch NA, Ohla K. Food-pics: an image database for experimental research on eating and appetite. Front Psychol. 2014;5:617.
Marron EM, Viejo-Sobera R, Cuatrecasas G, Redolar-Ripoll D, Lorda PG, Datta A et al. Prefronto-cerebellar neuromodulation affects appetite in obesity. Int J Obes. 2018. https://doi.org/10.1038/s41366-018-0278-8.
Ziauddeen H, Alonso-Alonso M, Hill JO, Kelley M, Khan NA. Obesity and the neurocognitive basis of food reward and the control of intake. Adv Nutr Bethesda Md. 2015;6:474–86.
Vainik U, Dagher A, Dubé L, Fellows LK. Neurobehavioural correlates of body mass index and eating behaviours in adults: a systematic review. Neurosci Biobehav Rev. 2013;37:279–99.
Brunoni AR, Amadera J, Berbel B, Volz MS, Rizzerio BG, Fregni F. A systematic review on reporting and assessment of adverse effects associated with transcranial direct current stimulation. Int J Neuropsychopharmacol. 2011;14:1133–45.
Giacomo Fassini P, Das S, Suen V, Magerowski G, da Silva Junior W, Marchini J, et al. Prefrontal tDCS effects on appetite may depend on dopamine status: preliminary analysis of a clinical trial. Brain Stimulat. 2019;12:536.
Lapenta OM, Sierve KD, de Macedo EC, Fregni F, Boggio PS. Transcranial direct current stimulation modulates ERP-indexed inhibitory control and reduces food consumption. Appetite. 2014;83:42–8.
Fregni F, Orsati F, Pedrosa W, Fecteau S, Tome FAM, Nitsche MA, et al. Transcranial direct current stimulation of the prefrontal cortex modulates the desire for specific foods. Appetite. 2008;51:34–41.
Goldman RL, Borckardt JJ, Frohman HA, O’Neil PM, Madan A, Campbell LK, et al. Prefrontal cortex transcranial direct current stimulation (tDCS) temporarily reduces food cravings and increases the self-reported ability to resist food in adults with frequent food craving. Appetite. 2011;56:741–6.
Kekic M, McClelland J, Campbell I, Nestler S, Rubia K, David AS, et al. The effects of prefrontal cortex transcranial direct current stimulation (tDCS) on food craving and temporal discounting in women with frequent food cravings. Appetite. 2014;78:55–62.
Ljubisavljevic M, Maxood K, Bjekic J, Oommen J, Nagelkerke N. Long-term effects of repeated prefrontal cortex transcranial direct current stimulation (tDCS) on food craving in normal and overweight young adults. Brain Stimulat. 2016;9:826–33.
Truong DQ, Magerowski G, Blackburn GL, Bikson M, Alonso-Alonso M. Computational modeling of transcranial direct current stimulation (tDCS) in obesity: Impact of head fat and dose guidelines. NeuroImage Clin. 2013;2:759–66.
Acknowledgements
PLV is supported by University of Alcalá (grant FPI2016). MA-A is a recipient of grants from the Boston Nutrition and Obesity Research Center, P30 DK046200, the Nutrition Obesity Research Center at Harvard, P30 DK040561, and the Center for Nutritional Research Charitable Trust. We thank Dr Daniela S. Trifu, Centro Médico Complutense, for her time, advice and supervision of the dietary component of the intervention. We are deeply grateful to all volunteers who took part in this study for their time and help.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Amo Usanos, C., Valenzuela, P.L., de la Villa, P. et al. Neuromodulation of the prefrontal cortex facilitates diet-induced weight loss in midlife women: a randomized, proof-of-concept clinical trial. Int J Obes 44, 568–578 (2020). https://doi.org/10.1038/s41366-019-0486-x
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41366-019-0486-x
This article is cited by
-
Neurobiological regulation of eating behavior: Evidence based on non-invasive brain stimulation
Reviews in Endocrine and Metabolic Disorders (2022)
-
Efficacy and acceptability of noninvasive brain stimulation interventions for weight reduction in obesity: a pilot network meta-analysis
International Journal of Obesity (2021)
-
Noninvasive neuromodulation of the prefrontal cortex in young women with obesity: a randomized clinical trial
International Journal of Obesity (2020)