Abstract
Recent studies have suggested that obesity might be protective in specific conditions such as critical illness; however, there are controversial data in critically ill children with obesity. The aim of this study was to investigate the association of obesity with mortality and other outcomes in these patients. We conducted a systematic review of observational studies investigating obesity in critically ill children, published by August 2017 in PubMed and Scopus. After screening documents, 15 articles with 142119 patients were included in the systematic review and meta-analysis. The results were reported with odds ratio (OR) or standard mean difference (SMD). The primary outcome was mortality and the secondary outcomes were length of ICU stay (ICU LOS), length of hospital stay (hospital LOS), and duration of mechanical ventilation (MV). The analysis showed that critically ill children without obesity had lower risk of mortality compared to patients with obesity (OR 0.79, 95% CI 0.64 to 0.97, P = 0.025, I2 = 35.2%). Hospital LOS was also significantly lower in children without obesity (pooled SMD −0.12, 95% CI −0.21 to −0.04, P = 0.004, I2 = 8.1%). There were no differences in ICU LOS (95% CI −0.19 to 0.01, P = 0.083) and duration of MV (95% CI −0.22 to 0.03, P = 0.136) between critically ill children with and without obesity. In conclusion, the current systematic review and meta-analysis revealed that critically ill children with obesity have higher risk of mortality and length of hospital stay compared to the group without obesity. Further prospective studies are essential to elucidate the role of obesity and underlying mechanisms in predicting outcomes of critically ill children.
Similar content being viewed by others
Introduction
Pediatric obesity has increased worldwide in recent decades. Based on 2015–2016 National Health and Nutrition Examination Survey (NHANES), around 18.5% of the population between 2 and 19 years old had obesity in the United States [1]. Childhood obesity could be associated with extensive metabolic derangements including diabetes, cardiovascular diseases, hypertension, polycystic ovary syndrome and also premature mortality in adult life [2]. Obesity might be also associated with different patterns of injury and outcomes in trauma. Higher risk of post-surgical infections, complicated artificial respiration, and coagulation disorders were observed in patients with obesity following trauma [3]. Obesity could affect the medical and surgical care of critically ill patients. Patients with obesity usually require additional hospital staff and special equipment [4]. There are major challenges in nutritional support and pharmacological treatments of these patients. The pharmacokinetics of drugs are not well defined in this group and might be different due to greater extracellular volume, fat mass and fat free mass [5].
Despite these complications, it has been shown that obesity is associated with lower risk of death compared to normal BMI in critically ill patients [6, 7]. However, this hypothesis is still a matter of discussion especially in youth. To our knowledge, no meta-analysis was conducted evaluating the association of obesity with mortality in children with critical illness. However, a systematic review [8] described that similar to studies in adults, conflicting results are observed in primary studies investigating the influence of obesity on clinical outcomes in hospitalized children. There was a relationship between obesity and mortality in almost half of the articles. A significant association was also seen between obesity with infections and hospital stay in a number of studies. This systematic review included both acute and chronic critical illnesses and no pooled data meta-analysis was performed.
Thus, the aim of this study was to investigate the association of obesity with mortality and other outcomes including length of hospital and intensive care unit (ICU) stay, and duration of mechanical ventilation in critically ill children.
Methods
Search strategy
We performed a systematic search for observational studies investigating obesity in pediatric patients with critical illness. Articles published in electronic databases including PubMed and Scopus, from 1990 to August 2017, were explored without language restriction, by EA and MY. Finally, references of the most relevant articles were checked to ensure the completeness of the search.
The search was done using following MeSH or non-MeSH keywords:
(1) “obese”, “obesity”, “overweight”, “body mass index”, “BMI”, “body weight”, and (2) “critical care”, “intensive care”, “ICU”, “critical illness”, “critically ill” and (3) “mortality”, “death”, “fatality”.
Study selection
The inclusion criteria were original observational studies (prospective or retrospective) comparing mortality in critically ill children and adolescence with and without obesity.
Obesity was defined as weight-for-length (for children below 2 years) or BMI-for-age (for those 2 years and older) percentile ≥ 95th [9] or Z score ≥ 2 [10, 11].
Articles exclusively on chronic critical illness such as advanced cancer, and transplantation were not included. The primary outcome was mortality. Length of ICU stay (ICU LOS), length of hospital stay (hospital LOS), and duration of mechanical ventilation (MV) were secondary outcomes if available. Titles and abstracts of studies were reviewed independently by two investigators (EA and SMN). Disagreements of including abstracts were referred to the other author MY.
Data extraction
The data were extracted as follows: (1) the full name of first author, (2) type of study, (3) year of publication, (4) country/region, (5) sample size, (6) the criteria used to define obesity, (7) age, (8) sex, (9) rate of mortality, and mean values and standard deviation (SD) or standard error of the mean (SEM) of (10) ICU LOS, (11) hospital LOS, and (12) MV. All SEM values were translated into SD using the sample size of the study. We contacted the corresponding author of studies with missing data at least three times, five days apart.
Study quality assessment
The quality of eligible articles was evaluated using a version of Newcastle-Ottawa scale adapted for cohort studies [12] by SMN and was rechecked by MY. This scale rates articles based on eight aspects of each study in three domains of selection with maximum 4 stars, comparability with maximum 2 stars, and outcomes with maximum 3 stars. Studies with a total score of 0–6 were considered to have moderate quality and 7–9 to have high quality.
Data analysis
To demonstrate the association of obesity with mortality in each study as well as the pooled effect and related 95% confidence intervals (CI) visually, we used forest plots. The results were reported with odds ratios (ORs) or standard mean differences (SMDs). To evaluate the heterogeneity of studies, we used the Cochran Q test and the I2 index and P value <0.05 was considered as heterogeneity. To compensate a possible heterogeneity in the results of the studies, we performed subgroup analysis for study design. In addition, we used random effect model to handle any residual heterogeneity in the results of the studies. We used Meta regression to investigate the possible effect of covariates (age and sex) on results. To evaluate a possible publication bias we used Funnel plot (Qualitative method), and Begg’s and Egger’s regression test and plot (Quantitative method). All statistical analysis was performed using the STATA (StataCorp. 2013. Stata Statistical Software: Release 13. College Station, TX: StataCorp LP).
Reporting of data was performed according to preferred reporting items for systematic reviews and meta-analyses (PRISMA) guideline. The study protocol has been registered in the international prospective register of systematic reviews database (http://www.crd.york.ac.uk/PROSPERO, registration no: CRD42017080565).
Results
Included studies
In this study, 3022 records were found by electronic and hand search. After removing the duplicate references, 2171 documents were remained, which then were checked precisely by titles and abstracts. Finally, the full texts of 41 articles were assessed and 15 articles were found eligible for the systematic review and meta-analysis [7, 13,14,15,16,17,18,19,20,21,22,23,24,25,26], (Fig. 1).
The characteristics of studies included in the systematic review and meta-analysis are available in Table 1 (and supplementary Table 1). The studies were published between 2006 and 2017. Eleven studies were retrospective and four were prospective. The majority of studies (n = 11) were performed in centers in the United States. There was no eligible study with language other than English. All the studies included both sexes.
Quality assessment of the included studies
Based on Newcastle-Ottawa scale, the overall quality scores ranged from five to eight. It has been shown that eight articles had high quality scores (7 or more), and seven articles had moderate quality scores (below 7) (Table 2).
Mortality
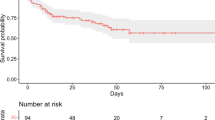
The meta-analysis of pooled data from 15 studies [7, 13,14,15,16,17,18,19,20,21,22,23,24,25,26] including 142119 critically ill children, 18323 with obesity and 123796 without obesity, showed a significant lower risk of mortality for patients without obesity compared to those with obesity (OR 0.79, 95% CI 0.64 to 0.97, P = 0.025, I2 = 35.2%, Fig. 2). We removed two studies [16, 24] and repeated the analysis, because these studies investigated specific subgroups of patients with considerable higher rate of mortality compared to other children with critical illness. The results showed again significant lower risk of mortality among critically ill children without obesity than those with obesity (OR 0.82, 95% CI 0.72 to 0.93, P = 0.001, I2 = 2.7%). No publication bias was detected using asymmetry tests (Egger’s test, P = 0.172 and Begg’s test, P = 0.956, Funnel plots in Fig. 3). Meta-regression analysis showed no modifying effect for age (P = 0.688) and sex (P = 0.709).
Forest plot demonstrating meta-analysis of studies investigating mortality in critically ill children with obesity compared to those without obesity (The shaded boxes indicate the sample size, points indicate the observed OR, and the horizontal lines around the points showed the 95% CI of the OR in each study. The diamond indicates the pooled OR and corresponding 95% CI. I-squared and P values show heterogeneity between the studies)
ICU LOS
We had 10 articles that have reported ICU LOS [13,14,15, 17, 19,20,21,22, 25, 26], with total sample size of 11830, including 1011 patients with obesity and 10819 without obesity. As shown in Fig. 4, length of ICU stay was longer in children with obesity compared to those without obesity, but not statistically significant (pooled SMD −0.09, 95% CI −0.19 to 0.01, P = 0.083, I2 = 45.9%). No publication bias was identified by Egger’s test (P = 0.180) and Begg’s test (P = 0.245).
Forest plot demonstrating meta-analysis of studies investigating length of stay in ICU in critically ill children with obesity compared to those without obesity (The shaded boxes indicate the sample size, points indicate the observed SMD, and the horizontal lines around the points showed the 95% CI of the SMD in each study. The diamond indicates the pooled SMD and corresponding 95% CI. I-squared and P values show heterogeneity between the studies)
Hospital LOS
Seven articles [14, 17, 19, 21, 22, 25, 26] reported data about length of stay in hospital. In this analysis, 5028 critically ill children, 769 with obesity and 4259 without obesity, were included. Length of stay in hospital was significantly lower in critically ill children without obesity compared to those with obesity (pooled SMD −0.12, 95% CI −0.21 to −0.04, P = 0.004, I2 = 8.1%, Fig. 5).
Forest plot demonstrating meta-analysis of studies investigating length of stay in hospital in critically ill children with obesity compared to those without obesity (The shaded boxes indicate the sample size, points indicate the observed SMD, and the horizontal lines around the points showed the 95% CI of the SMD in each study. The diamond indicates the pooled SMD and corresponding 95% CI. I-squared and P values show heterogeneity between the studies)
MV
The meta-analysis of eight studies [14, 17, 19,20,21,22, 25, 26] including 6058 patients, 909 with obesity and 5149 without obesity suggested that the duration of MV was shorter in the group without obesity, although the difference did not attain significance (pooled SMD −0.10, 95% CI −0.22 to 0.03, P = 0.136, I2 = 61.2%, Fig. 6).
Forest plot demonstrating meta-analysis of studies investigating duration of mechanical ventilation in critically ill children with obesity compared to those without obesity (The shaded boxes indicate the sample size, points indicate the observed SMD, and the horizontal lines around the points showed the 95% CI of the SMD in each study. The diamond indicates the pooled SMD and corresponding 95% CI. I-squared and P values show heterogeneity between the studies)
There was no evidence of publication bias for hospital LOS (Egger’s test, P = 0.103 and Begg’s test, P = 0.881) and MV (Egger’s test, P = 0.097 and Begg’s test, P = 0.322), Fig. 3. However, it should be considered that the power of these tests is confined when including less than 10 studies [27].
Discussion
This meta-analysis showed critically ill children with obesity, exhibited higher mortality compared to patients without obesity. In addition, length of hospital stay was significantly higher in the group with obesity compared to those without obesity. Duration of ICU stay and need for MV were also tended to be higher in children with obesity, although not statistically significant. Due to lower duration of having obesity in pediatrics and generally lower prevalence of comorbidities like diabetes and cardiovascular disorders, which all could complicate critical illness, it might be expected that children with obesity would not have worse outcomes compared to group without obesity. In addition, it has been stated that there is less challenge for appropriate equipment, hospital personnel and vascular and airway access compared to adult critically ill patients with obesity [19]. However, the current systematic review and meta-analysis did not support these speculations. The negative impact of obesity on mortality and other outcomes in children might be due to individual characteristics, type of disease, and medical care. For example, if actual body weight is used instead of ideal body weight for calculations of artificial ventilation in children with obesity (which does not seem to be rare in practice), they will be at higher risk of ventilator-induced lung injury and mortality [18]. Besides, it has been observed that obesity is associated with more adverse respiratory events and chance of dependence on respiratory support [28]. Higher BMI could also predict multiple organ failure, a significant contributor of mortality, in pediatric patients [23]. It has been stated that even in lack of significant difference in mortality between groups with and without obesity, children with obesity had longer duration of ICU stay and more complications such as sepsis and wound infection [26].
The results of this study can be compared with the findings from prior meta-analyses in critically ill adults. Contrary to the results of the current study, these meta-analysis studies showed a decreasing trend for risk of mortality in patients with overweight and obesity (BMI: 25–40 kg/m2) compared to normal weight group [29], and lower hospital, but not ICU, mortality for patients with obesity and morbid obesity [30]. Another meta-analysis in adults reported that there was no difference in mortality between patients with and without obesity; however, group with obesity showed higher survival rate at the time of hospital discharge [31]. Moreover, Akinnusi et al. [31] showed longer ICU LOS and MV duration in adult patients with obesity. Oliveros et al. [29] reported longer ICU LOS for adult patient with overweight, but not with obesity, compared to normal BMI. Hogue et al. [30] observed no correlation between obesity and ICU LOS or MV. Current data in pediatrics did not indicate any significant difference in ICU LOS or MV duration between the groups with and without obesity, however, showed higher hospital LOS in the patients with obesity. The findings of meta-analyses in adults are affected by significant heterogeneity of the studies. The prevalence of obesity in adults (about 30% [30]) was also higher compared to pediatric patients of the current study (about 13%). The adult studies have emphasized on the need for more studies on critically ill adults due to high resource utilization. The lack of researches investigating mechanisms of the effect of obesity on complications of critical illness has been also mentioned in adult meta-analysis studies; however they referred their observations on mortality to “reverse epidemiology” or “obesity paradox”. However, the findings of this study in pediatrics are an example of violation for this term. Obesity paradox has been initially used in patients with percutaneous coronary intervention in 2002 [32]. Then it was widely assessed in other chronic disorders, and recently in critical illness. Although the underlying reasons are not still well documented, some potential mechanisms have been suggested for the paradoxical role of obesity in critical conditions. It has been stated that higher BMI, body fat and muscle mass could be considered as better nutritional reserves in critical illness and trauma, which are associated with increased energy expenditure, catabolism and inflammation [33]. In addition, cellular and molecular studies have been proposed that the capacity of adipocytes to accumulate glucose and lipid metabolites increase during critical illness [34]. Changes in level and function of adipokines have also been among the causes of inverse relationship between obesity and mortality in critical conditions. For example, some clinical studies have reported higher leptin concentrations in survived critically ill patients [35,36,37]. Other studies have shown that higher adiponectin concentration was directly associated with mortality in adults with critical illness [38] and pediatric with septic shock [39]. It should be considered that many studies investigating the underlying mechanisms of obesity paradox were performed in adults, and the evidence was not confirmed in pediatric population. Besides, very recently it has been suggested that using the term “obesity paradox” might be misleading [40]; probably there is no advantageous for obesity, but being normal weight and underweight is accompanied with worse outcomes [41].
The interpretation of the findings of this study should be done considering some limitations. The literature is limited about the obesity outcomes in youth with critical illness. Some studies in the field are retrospective, have extracted and analyzed data from hospital documents or registries. This might have caused a selection bias in primary studies because a large number of patients have been removed due to lack of anthropometric data. For example, Vaughan et al. [13] included 117 of 1012 (12%) and Alselaim et al. [21] included 933 of 3848 (24%) admitted patients because of no documented height or weight for the rest. In addition, few studies have provided sufficient data on the history of diabetes, endocrine disorders, organ failure, and other comorbidities that could affect the outcomes in children with critical illness. These issues indicate the necessity of improving registration systems in pediatric intensive care centers, which might help to address the relationship of baseline characteristics with clinical outcomes. We also need to know more about important determinants including volumes of resuscitation fluids, and type, time of initiation, and adequacy of nutritional support during intensive care stay, which all might affect the clinical outcomes. Medications could also differentially affect patients with and without obesity. Currently the priority of adjusting drug dosages for body weight, and differences in pharmacokinetic and pharmacodynamic of drugs between critically ill patients with normal weight and obesity are not clear.
In the literature, many studies have classified and compared patients to groups with and without obesity. This kind of classification did not let us to differentiate the effect of BMI categories more precisely, especially about children with undernourishment and morbid obesity. Besides, different cut-offs are used to determine obesity in youth, which might affect data on the prevalence of obesity and related outcomes. Moreover, body fat distribution and body composition might be effective on outcomes. However, weight-, height- and BMI-based classifications could not discriminate body fat from muscle mass, and contribution of each component to predicting survival and other outcomes.
To our knowledge, this meta-analysis seems to be the first study investigating the association of obesity with mortality and other outcomes in critically ill children. The other strength of the current study includes the comprehensive search strategy to cover all researches investigating the relationship between obesity and morality in critical illness without language restriction. Additionally, there was very low and non-significant heterogeneity between the studies for mortality and hospital LOS, which increases the credibility of the results.
Conclusion
Critically ill children with obesity exhibited higher mortality compared to group without obesity. Length of hospital stay was also considerably higher in children with obesity. Further studies with prospective design are required to elucidate the role of obesity and underlying mechanisms in predicting outcomes of critically ill children.
References
Hales CM, Fryar CD, Carroll MD, Freedman DS, Ogden CL. Trends in obesity and severe obesity prevalence in us youth and adults by sex and age, 2007–2008 to 2015–2016. JAMA. 2018;319:1723–5.
Reilly JJ, Kelly J. Long-term impact of overweight and obesity in childhood and adolescence on morbidity and premature mortality in adulthood: systematic review. Int J Obes. 2011;35:891–8.
Brown CV, Velmahos GC. The consequences of obesity on trauma, emergency surgery, and surgical critical care. World J Emerg Surg. 2006;1:27.
Patel JJ, Rosenthal MD, Miller KR, Codner P, Kiraly L, Martindale RG. The critical care obesity paradox and implications for nutrition support. Curr Gastroenterol Rep. 2016;18:45.
Shashaty MG, Stapleton RD. Physiological and management implications of obesity in critical illness. Ann Am Thorac Soc. 2014;11:1286–97.
Pickkers P, de Keizer N, Dusseljee J, Weerheijm D, van der Hoeven JG, Peek N. Body mass index is associated with hospital mortality in critically ill patients: an observational cohort study. Crit Care Med. 2013;41:1878–83.
Ward SL, Gildengorin V, Valentine SL, Sapru A, Curley MA, Thomas N, et al. Impact of weight extremes on clinical outcomes in pediatric acute respiratory distress syndrome. Crit Care Med. 2016;44:2052–9.
Bechard LJ, Rothpletz-Puglia P, Touger-Decker R, Duggan C, Mehta NM. Influence of obesity on clinical outcomes in hospitalized children: a systematic review. JAMA Pediatr. 2013;167:476–82.
Kuczmarski RJ, Ogden CL, Grummer-Strawn LM, Flegal KM, Guo SS, Wei R, et al. CDC growth charts: United States. Adv Data. 2000;314:1–27.
WHO Child Growth. Standards based on length/height, weight and age. Acta Paediatr Suppl. 2006;76–85.
de Onis M, Onyango AW, Borghi E, Siyam A, Nishida C, Siekmann J. Development of a WHO growth reference for school-aged children and adolescents. Bull World Health Organ. 2007;85:660–7.
Wells G, Shea B, O'Connell D, Peterson J, Welch V, Losos M, et al. The Newcastle-Ottawa Scale (NOS) for assessing the quality of nonrandomised studies in meta-analyses. 2011. http://www.ohri.ca/programs/clinical_epidemiology/oxford.asp.
Vaughan N, Tweed J, Greenwell C, Notrica DM, Langlais CS, Peter SD, et al. The impact of morbid obesity on solid organ injury in children using the ATOMAC protocol at a pediatric level I trauma center. J Pediatr Surg. 2017;52:345–8.
Chen MY, Yang YJ. Being underweight is an independent risk factor for poor outcomes among acutely critically ill children. Nutr Clin Pract. 2017;33:433–8.
Martinez EE, Ariagno KA, Stenquist N, Anderson D, Munoz E, Mehta NM. Energy and protein delivery in overweight and obese children in the pediatric intensive care unit. Nutr Clin Pract. 2017;32:414–9.
Anton-Martin P, Papacostas M, Lee E, Nakonezny PA, Green ML. Underweight status is an independent predictor of in-hospital mortality in pediatric patients on extracorporeal membrane oxygenation. JPEN J Parenter Enteral Nutr. 2016; pii: 0148607116673185.
Bechard LJ, Duggan C, Touger-Decker R, Parrott JS, Rothpletz-Puglia P, Byham-Gray L, et al. Nutritional status based on body mass index is associated with morbidity and mortality in mechanically ventilated critically ill children in the PICU. Crit Care Med. 2016;44:1530–7.
Ross PA, Newth CJ, Leung D, Wetzel RC, Khemani RG. Obesity and mortality risk in critically Ill children. Pediatrics . 2016;137:e20152035.
Ross E, Burris A, Murphy JT. Obesity and outcomes following burns in the pediatric population. J Pediatr Surg. 2014;49:469–73.
Goh VL, Wakeham MK, Brazauskas R, Mikhailov TA, Goday PS. Obesity is not associated with increased mortality and morbidity in critically ill children. JPEN J Parenter Enter Nutr. 2013;37:102–8.
Alselaim N, Malaekah H, Saade M, Hussein M, Altokhais T, Albedah K, et al. Does obesity impact the pattern and outcome of trauma in children? J Pediatr Surg. 2012;47:1404–9.
Backstrom IC, MacLennan PA, Sawyer JR, Creek AT, Rue LW III, Gilbert SR. Pediatric obesity and traumatic lower-extremity long-bone fracture outcomes. J Trauma acute care Surg. 2012;73:966–71.
Kraft R, Herndon DN, Williams FN, Al-Mousawi AM, Finnerty CC, Jeschke MG. The effect of obesity on adverse outcomes and metabolism in pediatric burn patients. Int J Obes. 2012;36:485–90.
Srinivasan V, Nadkarni VM, Helfaer MA, Carey SM, Berg RA, American Heart Association National Registry of Cardiopulmonary Resuscitation I. Childhood obesity and survival after in-hospital pediatric cardiopulmonary resuscitation. Pediatrics. 2010;125:e481–8.
Rana AR, Michalsky MP, Teich S, Groner JI, Caniano DA, Schuster DP. Childhood obesity: a risk factor for injuries observed at a level-1 trauma center. J Pediatr Surg. 2009;44:1601–5.
Brown CV, Neville AL, Salim A, Rhee P, Cologne K, Demetriades D. The impact of obesity on severely injured children and adolescents. J Pediatr Surg. 2006;41:88–91.
Sterne JA, Gavaghan D, Egger M. Publication and related bias in meta-analysis: power of statistical tests and prevalence in the literature. J Clin Epidemiol. 2000;53:1119–29.
Tait AR, Voepel-Lewis T, Burke C, Kostrzewa A, Lewis I. Incidence and risk factors for perioperative adverse respiratory events in children who are obese. Anesthesiology. 2008;108:375–80.
Oliveros H, Villamor E. Obesity and mortality in critically ill adults: a systematic review and meta-analysis. Obesity. 2008;16:515–21.
Hogue CW Jr., Stearns JD, Colantuoni E, Robinson KA, Stierer T, Mitter N, et al. The impact of obesity on outcomes after critical illness: a meta-analysis. Intensive Care Med. 2009;35:1152–70.
Akinnusi ME, Pineda LA, El Solh AA. Effect of obesity on intensive care morbidity and mortality: a meta-analysis. Crit Care Med. 2008;36:151–8.
Gruberg L, Weissman NJ, Waksman R, Fuchs S, Deible R, Pinnow EE, et al. The impact of obesity on the short-term and long-term outcomes after percutaneous coronary intervention: the obesity paradox? J Am Coll Cardiol. 2002;39:578–84.
Preiser JC, Ichai C, Orban JC, Groeneveld AB. Metabolic response to the stress of critical illness. Br J Anaesth. 2014;113:945–54.
Marques MB, Langouche L. Endocrine, metabolic, and morphologic alterations of adipose tissue during critical illness. Crit Care Med. 2013;41:317–25.
Grigoras I, Branisteanu D, Ungureanu D, Rusu D, Ristescu I. Early dynamics of leptin plasma level in surgical critically ill patients: a prospective comparative study. Chir (Bucur). 2014;109:66–72.
Bornstein S, Licinio J, Tauchnitz R, Engelmann L, Negrao A, Gold P, et al. Plasma leptin levels are increased in survivors of acute sepsis: associated loss of diurnal rhythm in cortisol and leptin secretion. J Clin Endocrinol & Metab. 1998;83:280–3.
Arnalich F, López J, Codoceo R, Jiménez M, Madero R, Montiel C. Relationship of plasma leptin to plasma cytokines and human survival in sepsis and septic shock. J Infect Dis. 1999;180:908–11.
Koch A, Sanson E, Voigt S, Helm A, Trautwein C, Tacke F. Serum adiponectin upon admission to the intensive care unit may predict mortality in critically ill patients. J Crit Care. 2011;26:166–74.
Kaplan JM, Denenberg A, Monaco M, Nowell M, Wong H, Zingarelli B. Changes in peroxisome proliferator-activated receptor-gamma activity in children with septic shock. Intensive Care Med. 2010;36:123–30.
Flegal KM, Ioannidis JPA. The obesity paradox: a misleading term that should be abandoned. Obesity. 2018;26:629–30.
Li S, Wang Z, Huang J, Fan J, Du H, Liu L, et al. Systematic review of prognostic roles of body mass index for patients undergoing lung cancer surgery: does the 'obesity paradox' really exist? Eur J Cardiothorac Surg. 2017;51:817–28.
Acknowledgements
This manuscript has been supported by Iran University of Medical Sciences.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher’s note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
About this article
Cite this article
Alipoor, E., Hosseinzadeh-Attar, M.J., Yaseri, M. et al. Association of obesity with morbidity and mortality in critically ill children: a systematic review and meta-analysis of observational studies. Int J Obes 43, 641–651 (2019). https://doi.org/10.1038/s41366-019-0319-y
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41366-019-0319-y
This article is cited by
-
Association of obesity with mortality and clinical outcomes in children and adolescents with transplantation: A systematic review and meta-analysis
Reviews in Endocrine and Metabolic Disorders (2021)