Abstract
The insulin (INS) and IGF 2 (IGF2) genes are in close proximity to each other and undergo maternal imprinting during fetal growth. We investigated the association between maternal and umbilical cord IGF 2 protein (IGF-II) levels and single nucleotide polymorphisms (SNPs) in the INS and IGF2 genes in 207 healthy African-American mother-newborn pairs. No association was found between maternal IGF-II levels and polymorphism in the INS-IGF2 locus. A significant association was found between newborn IGF-II levels and two SNPs (rs3842738 and rs689) at the 5′ end of the INS-IGF2 locus. Analyses of haplotypes inferred from these two SNPs demonstrate a significant relationship between paternally transmitted haplotypes and newborn IGF-II levels, but no association with maternally transmitted haplotypes.
Similar content being viewed by others
Main
Being small for gestational age is correlated with predisposition to various illnesses, although this association remains controversial (1,2). Full-term, low birth weight infants are at least five times more likely to die in the first year and are second only to premature infants in their rates of morbidity and mortality (3,4). As adults, individuals born small for gestational age (SGA) are at elevated risk of pregnancy-induced hypertension (5), gestational diabetes (6), chronic hypertension (7), type 2 diabetes (8,9), and cardiovascular disease (10).
The relationship between birth size and adult predisposition to chronic disease has been heavily debated. According to the “fetal origins” (11) hypothesis, an inadequate uterine environment results in long-term alterations in organ structure and function and in hormonal milieu that make the individual more susceptible to disease. The existence of genetic factors common to both reduced fetal growth and disease predisposition is another explanation. This hypothesis is supported by an inverse correlation between paternal mortality and offspring birth size that is only slightly weaker than that between maternal mortality and offspring birth size (12,13), even after adjusting for lifestyle risk factors and socioeconomic status. Imprinted loci, which include several genes with direct roles in pathogenesis (i.e. insulin, insulin-like growth factor 2 gene (IGF2), insulin-like growth factor gene receptor (IGF2R)), may comprise a key part of this connection.
Insulin-like growth factor 2 protein (IGF-II) is expressed abundantly in trophoblast and fetal endothelial cells (14). The IGF2 gene resides within a block of genes at 11p15 that undergo the silencing (or imprinting) of the allele inherited from one of the parents during fetal development. In the case of IGF2, the allele inherited from the mother is imprinted (15) before implantation, around the eight-cell stage (16). Several lines of evidence indicate that IGF2 and other genes at 11p15 have significant effects on fetal growth. Loss of imprinting at 11p15, including biallelic expression of IGF2, is associated with the prenatal overgrowth of Beckwith-Wiedemann Syndrome (17) and with some cases of postnatal overgrowth (18,19). Conversely, hypomethylation of the telomeric imprinting center region (ICR1) is found in a proportion of pre- and postnatally growth-retarded individuals with Silver-Russell Syndrome. The hypomethylation of ICR1 appears to result in biallelic expression of the nearby paternally imprinted H19 gene with consequent under expression of IGF2 (20–22). In the mouse, disruption of IGF2 expression during development results in growth retarded pups (23,24). Conversely, transgenic doubling of IGF2 expression in the mouse results in fetal overgrowth (25).
It has been difficult to identify a clear connection between IGF-II levels in pregnancy and newborn size. Several studies have found a significant reduction in umbilical cord IGF-II levels in small for gestational age newborns (26–29), while a similar number of studies have found no relationship (30–33). Part of the inconsistency in the relationship between birth weight and fetal IGF-II levels may be attributable to variation in the ratio of IGF-II to the soluble portion of the IGF-II receptor, which promotes the degradation of IGF-II but is rarely measured in studies of birth weight (34).
The goal of the present study was to test the relationship between single nucleotide polymorphisms (SNPs) in the insulin gene (INS)-IGF2 locus and circulating levels of IGF-II in the mother and newborn. The paternal allele of IGF2 accounts for most of the production of the IGF-II protein (15). Therefore, we tested the association between circulating IGF-II levels and polymorphism in the INS-IGF2 locus, as well as the possibility that the effect of SNPs alleles differs according to the parent of origin of the alleles.
MATERIALS AND METHODS
Subjects.
Informed consent was acquired from 207 healthy African-American women with uncomplicated pregnancies upon admission for delivery at the University of Mississippi Medical Center (Jackson, MS) and the Regional Medical Center at Memphis (Tennessee). Only subjects who delivered healthy newborns were retained in the study. Inclusion criteria were: singleton pregnancy, >36 wk gestation, 18–35 y old. Exclusion criteria were chosen to eliminate a large number of additional contributing factors to birth weight variation and included, among others: smoking, diabetes (type 1, type 2, gestational), hypertension/vascular disease, preeclampsia, autoimmune disease, infectious disease (e.g. hepatitis, HIV), sickle-cell disease, uterine infection, illicit drug use, and birth defects. The following maternal characteristics potentially related to newborn size were recorded: parity, age, body mass index (BMI), and weight gain during pregnancy. The Institutional Review Boards of both institutions approved this study.
Genotyping.
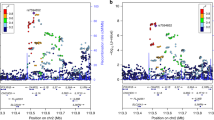
Maternal blood was collected during labor, umbilical cord blood was collected at delivery, and DNA was extracted. Six SNPs were selected by several criteria, including allele frequencies in excess of 10%, previous association with obesity- or diabetes-related traits, and linkage disequilibrium with the INS variable number of tandem repeats locus (VNTR) (35–39) (Fig. 1, Table 1). SNPs were genotyped using either TaqMan Assay by Demand or Assay by Design (rs3842748 and rs3213233; details available upon request) kits from Applied Biosystems Inc. At least two representatives of each genotype at each site were sequenced to verify the accuracy of the TaqMan assay and to resolve any ambiguous genotypes.
IGF-II measurements.
Maternal and fetal cord blood plasmas were assayed for IGF-II concentration using an ELISA assay developed with components from R & D Systems (Minneapolis, MN). Because IGF binding proteins present in plasma may compete for IGF-II binding in ELISA, an acid/ethanol extraction of the samples was performed (40,41) to separate binding proteins from IGF-II, followed by centrifugation to remove the binding proteins. Five microliters of plasma, 2.5 μL of PBS + 1% BSA (fraction V), and 62.5 μL of acid/ethanol (0.25 N HCl in 87% ethanol) were mixed and allowed to stand for 30 min. The pH was adjusted to 7.6 by addition of 22 μL of 0.8M Tris, and the samples were centrifuged in a microcentrifuge for 10 min in a cold room at 10,000× g. Twenty microliters of the supernatant was assayed for IGF-II in the presence of 80 μL of Krebs Ringer phosphate (KRP) buffer to achieve a final ethanol concentration below 15% because higher concentrations of ethanol were found to interfere with the assay. Blanks and standards were assayed in the presence of 20 μL of an acid-ethanol extract of KRP buffer +1% albumin with the same concentration of ethanol as in the samples from subjects. The final reaction volume was 100 μL. The plasma samples were assayed in duplicate, and the average of the two values was used as the protein concentration. The coefficient of variation for most samples was <5%. Plasma samples for which the coefficient of variation was 10% or greater were repeated. Only 15% of the samples required repetition because of a high coefficient of variation. ELISA used 0.3 μg/well of a mouse monoclonal anti-human IGF-II obtained from R & D Systems (MAB292, clone #75015), while the detection antibody was 0.025 μg/well of a biotin-labeled goat polyclonal anti-human IGF-II (BAF 292 from R & D Systems). The standard was recombinant human IGF-II (R & D Systems, 292-G2-050). The protocol was that recommended for use with R&D Douset ELISA development procedures.
Statistical analysis.
Characteristics of the SNPs are summarized in Table 1. Birth weight Z scores (SD from the mean birth weight), specific for gestational age, gender and ethnicity, were calculated based on U.S. Natality Statistics for 2001 and 2002 (National Center for Health Statistics).
Regression equations were selected by a backward selection process (42) in which all nongenetic variables were included in the model. The dependent variables used were maternal or newborn IGF-II concentration. With a sample size of 207 and a critical value of 0.05, we had power of 0.8 to detect a difference in IGF-II levels of 0.38 SD under an additive genetic model and 0.41 SD under a dominant genetic model (43). Fetal IGF-II values were normally distributed and required no transformation. Maternal IGF-II values were log-transformed. Among the nonsignificant partial regression coefficients, the variable with the smallest t statistic was removed and a new regression equation calculated. This process was repeated until a set of variables with significant partial regression coefficients was identified. Variables encoding the number of copies of the minor allele of each SNPs or number of copies of each haplotype in each individual were individually added to the regression equation to test for a significant association with IGF-II levels. The initial nongenetic variables used in regression on maternal IGF-II levels were newborn nearest week of gestation, parity, newborn birth weight Z, maternal BMI, and maternal height. The initial nongenetic model for regression on newborn IGF-II levels included nearest week of gestation, parity, gender, birth weight Z, and maternal BMI.
Haplotypes were inferred for the newborn SNPs exhibiting significant association with umbilical cord IGF-II levels using the program SNPHAP (http://www-gene.cimr.cam.ac.uk/clayton/software). Regression was performed with respect to the number of copies of each haplotype (i.e. 0, 1 or 2). For 162 mother-newborn pairs, the maternal and paternal origins of haplotypes could be directly inferred based upon the maternal and newborn haplotype combinations. In 45 cases, the mother and newborn were heterozygous for the same pair of haplotypes. In these cases, the parental origin of haplotypes could not be unambiguously inferred. ANOVA was performed to test for differences in mean umbilical cord IGF-II levels according to the parental origin of each haplotype, with the inclusion of birth weight Z score as a continuous covariable. In the case of ambiguous haplotype transmissions, both parental possibilities were included and given a weight half that of the unambiguous transmissions, resulting in a doubling of the variance for those observations. Separate analyses were performed for unambiguous transmissions and for a combination of ambiguous and unambiguous transmissions.
RESULTS
Association of SNPs with circulating IGF-II levels.
Maternal IGF-II levels covered a much broader range than did fetal levels (0.07–2.0 versus 0.24–0.68 μg/mL) and had a geometric mean (to compensate for extreme outliers) 20% higher than fetal levels (0.44 versus 0.53 μg/mL). None of the nongenetic variables tested (weeks gestation, parity, newborn Z score, maternal BMI, and maternal height) were found to be significant predictors of maternal IGF-II levels. Additionally, in regression analyses none of the maternal single nucleotide polymorphisms were found to be significantly associated with maternal IGF-II levels (Table 2). Among newborns, weeks gestation, parity, gender, and maternal BMI were excluded as significant predictors of newborn IGF-II levels. However, birth weight Z score was significantly associated with fetal IGF-II levels (p = 0.02). Among the SNPs, neither of the sites located within the IGF2 gene (rs734351 and rs3213233) were associated with IGF-II levels, nor were two of the SNPs within the INS (rs3842748 and rs3842756). However, the two SNPs located the furthest 5′ within the INS-IGF2 locus (rs3842738 and rs689) did exhibit significant (p = 0.02) association with fetal IGF-II levels.
Haplotypic association with fetal IGF-II levels.
Newborn haplotypes were inferred for the two SNPs exhibiting individual association with newborn IGF-II levels. Due to a high degree of linkage disequilibrium between the two sites (scaled covariance D' = 0.93) (44), one of the four possible haplotypes was not predicted while the remaining three haplotypes had frequencies ranging from 24 to 44%. Regression performed on the number of newborn copies of each haplotype and birth weight Z score indicated that one haplotype (G at rs3842738 and T at rs689) was associated with a reduction of 0.02 μg/mL per copy of the haplotype, whereas its complement (C at rs3842738 and A at rs689) was associated with an increase of 0.03 μg/mL per haplotype copy (Table 3). The third haplotype (CT) exhibited no association with newborn IGF-II levels.
Comparison of average fetal IGF-II levels according to the haplotype inherited from the mother found no significant difference among maternally inherited haplotypes (Table 4). Comparisons of fetal IGF-II levels among paternally inherited haplotypes found significant differences among the paternal haplotypes when either unambiguous or all possible transmissions were considered (p ≤ 0.01). Paternal haplotype GT is associated with the lowest average IGF-II levels (0.40 μg/mL; 0.24–0.63 μg/mL) and haplotype CA is associated with the highest average levels (0.47 μg/mL; 0.28–0.68 μg/mL).
DISCUSSION
We have found a significant effect of paternally inherited haplotypes upstream of the insulin gene on umbilical cord IGF-II levels. This observation is consistent with previous analyses demonstrating an unusually strong genetic component to IGF-II expression. Based on an analysis of middle-aged to elderly mono- and dizygotic twins, Harrela et al. (45) estimated an overall genetic heritability of 66% for IGF-II levels. The intra-twin correlation for dizygotic twins was about 50% that of monozygotic twins (r = 0.34 versus r = 0.66). A major factor in the intra-twin correlations may be the influence of shared, paternally derived INS VNTR alleles or SNPs haplotypes. Specifically, monozygotic twins share the same paternal SNPs and VNTR alleles, while dizygotic twins on average share the same paternal allele 50% of the time. In addition to environmental and epigenetic influences, the relative frequency of allele sharing of paternally derived variants between mono- and dizygotic twins may explain a significant proportion of their correlations in circulating IGF-II levels.
Furthermore, the pattern of association we observed between IGF-II levels and INS VNTR allele size classes in linkage disequilibrium with the genotyped SNPs is in agreement with the observations of Paquette et al. (46), who found that term human placentas had higher levels of IGF2 mRNA expression in the presence of the class I alleles compared with the longer class III alleles. This is consistent with our observation because haplotype CA (Table 2) is in high linkage disequilibrium with class I alleles based on the work of Stead et al. (35), and umbilical cord IGF-II levels are positively associated with the number of copies of that haplotype. Additionally, our results further suggest that it is the paternal origin of the INS-IGF2 allele that is relevant to IGF-II levels because maternally transmitted haplotypes exhibit no association with newborn IGF-II levels. This can be explained by the fact that the paternal alleles of INS and IGF2 account for the vast majority of RNA expression in several tissues key to fetal growth regulation, such as the yolk sac (47) and placenta (15).
Previously Adkins et al. (47a) found that a paternally transmitted haplotype composed of three SNPs (G at rs3842738, T at rs689, G at rs3842748) at the 5′ end of the INS-IGF2 locus conferred a 7-fold increased risk of small for gestational age birth compared with the haplotype CAC. Here, we have found that paternally transmitted haplotypes composed of two (rs3842738 and rs689) of those SNPs are associated with umbilical cord levels of IGF-II, with the lowest levels observed with haplotype GT, as would be expected given that haplotype GTG is associated with reduced birth weight. All three SNPs exhibit high linkage disequilibrium (D′ > 0.92) with one another; therefore, it is not certain why rs3842748 is not associated with both phenotypes (birth weight Z and IGF-II levels). It may be significant that the GT haplotype at rs3842738 and rs689 defines a distinct cluster of haplotypes (J, K, L, T, W, and Z, plus M, which has a back mutation from G to C) entirely of African origin (35). Possibly, the insulin VNTR substructure and/or a SNPs in high frequency among those haplotypes directly influences IGF-II production, while rs3842748 or a SNPs highly correlated with it is more directly involved in fetal growth regulation or insulin production. Indeed, there is evidence that rs689 is functional during the processing of the INS transcript (48) and that not only IGF2 SNPs but also subclasses of the INS class I VNTR alleles are associated with adult male BMI and circulating IGF-II levels (49–51). Quite possibly, the full explanation for our observations is a combination of a direct functional role of some SNPs and their high linkage disequilibrium with the functionally important INS VNTR alleles.
In contrast to newborns, we found no association among maternal IGF-II levels, newborn size, maternal anthropometry, or SNPs genotypes, despite evidence for a strong genetic component to IGF-II levels (45). The lack of a genetic association may be due to one or both of two factors. First compared with newborns there is likely to be a much greater environmental contribution to IGF-II levels among adults. For example, the duration and stress of labor, as well as endocrinological changes associated with parturition, may affect IGF-II levels and confound detection of genetic influences. This may partly explain the observation of positive correlation between maternal IGF-II levels and newborn size in some studies (26,52) but not others (53,54). Second the predominant influences on the level of IGF-II may be driven by different promoters and polymorphic sites in newborns and adults (49–51,55), and we may not have surveyed those sites that are important for adult IGF-II production.
Imprinting and other epigenetic controls of gene expression are key mechanisms through which the maternal and paternal genomes can influence the rate of fetal growth. Our demonstration that genetic polymorphism and paternal transmission of maternally imprinted loci is associated with variation in IGF-II levels suggests that imprinting may be a major influence on fetal growth regulation. On this basis, a fruitful avenue for future research would be to determine the role of polymorphisms and parental origin of other imprinted growth-regulating loci on the rate of fetal growth.
Abbreviations
- IGF-II:
-
insulin-like growth factor 2 protein
- IGF2:
-
insulin-like growth factor 2 gene
- INS:
-
insulin gene
- SNPs:
-
single nucleotide polymorphism
- VNTR:
-
variable number of tandem repeats locus
References
Huxley R, Neil A, Collins R 2002 Unravelling the fetal origins hypothesis: is there really an inverse association between birthweight and subsequent blood pressure?. Lancet 360: 659–665
Huxley R, Owen CG, Whincup PH, Cook DG, Colman S, Collins R 2004 Birth weight and subsequent cholesterol levels: exploration of the “fetal origins” hypothesis. JAMA 292: 2755–2764
Mathews TJ, MacDorman MF 2006 Infant mortality statistics from the 2003 period linked birth/infant death data set. Natl Vital Stat Rep 54: 1–29
McIntire DD, Bloom SL, Casey BM, Leveno KJ 1999 Birth weight in relation to morbidity and mortality among newborn infants. N Engl J Med 340: 1234–1238
Innes KE, Byers TE, Marshall JA, Baron A, Orleans M, Hamman RF 2003 Association of a woman's own birth weight with her subsequent risk for pregnancy-induced hypertension. Am J Epidemiol 158: 861–870
Innes KE, Byers TE, Marshall JA, Baron A, Orleans M, Hamman RF 2002 Association of a woman's own birth weight with subsequent risk for gestational diabetes. JAMA 287: 2534–2541
Frontini MG, Srinivasan SR, Xu J, Berenson GS 2004 Low birth weight and longitudinal trends of cardiovascular risk factor variables from childhood to adolescence: the bogalusa heart study. BMC Pediatr 4: 22
Rich-Edwards JW, Colditz GA, Stampfer MJ, Willett WC, Gillman MW, Hennekens CH, Speizer FE, Manson JE 1999 Birthweight and the risk for type 2 diabetes mellitus in adult women. Ann Intern Med 130: 278–284
Lithell HO, McKeigue PM, Berglund L, Mohsen R, Lithell UB, Leon DA 1996 Relation of size at birth to non-insulin dependent diabetes and insulin concentrations in men aged 50-60 years. BMJ 312: 406–410
Lawlor DA, Ronalds G, Clark H, Smith GD, Leon DA 2005 Birth weight is inversely associated with incident coronary heart disease and stroke among individuals born in the 1950s: findings from the Aberdeen Children of the 1950s prospective cohort study. Circulation 112: 1414–1418
Barker DJ 1998 Mother, Babies, and Health in Later Life. Churchill Livingstone, London
Smith GD, Sterne J, Tynelius P, Lawlor DA, Rasmussen F 2005 Birth weight of offspring and subsequent cardiovascular mortality of the parents. Epidemiology 16: 563–569
Andersen AM, Osler M 2004 Birth dimensions, parental mortality, and mortality in early adult age: a cohort study of Danish men born in 1953. Int J Epidemiol 33: 92–99
McKinnon T, Chakraborty C, Gleeson LM, Chidiac P, Lala PK 2001 Stimulation of human extravillous trophoblast migration by IGF-II is mediated by IGF type 2 receptor involving inhibitory G protein(s) and phosphorylation of MAPK. J Clin Endocrinol Metab 86: 3665–3674
Giannoukakis N, Deal C, Paquette J, Goodyer CG, Polychronakos C 1993 Parental genomic imprinting of the human IGF2 gene. Nat Genet 4: 98–101
Lighten AD, Hardy K, Winston RM, Moore GE 1997 IGF2 is parentally imprinted in human preimplantation embryos. Nat Genet 15: 122–123
Weksberg R, Smith AC, Squire J, Sadowski P 2003 Beckwith-Wiedemann syndrome demonstrates a role for epigenetic control of normal development. Hum Mol Genet 1: R61–R68
Ogawa O, Becroft DM, Morison IM, Eccles MR, Skeen JE, Mauger DC, Reeve AE 1993 Constitutional relaxation of insulin-like growth factor II gene imprinting associated with Wilms' tumour and gigantism. Nat Genet 5: 408–412
Morison IM, Becroft DM, Taniguchi T, Woods CG, Reeve AE 1996 Somatic overgrowth associated with overexpression of insulin-like growth factor II. Nat Med 2: 311–316
Bliek J, Terhal P, van den Bogaard MJ, Maas S, Hamel B, Salieb-Beugelaar G, Simon M, Letteboer T, van der Smagt J, Kroes H, Mannens M 2006 Hypomethylation of the H19 gene causes not only Silver-Russell syndrome (SRS) but also isolated asymmetry or an SRS-like phenotype. Am J Hum Genet 78: 604–614
Gicquel C, Rossignol S, Cabrol S, Houang M, Steunou V, Barbu V, Danton F, Thibaud N, Le Merrer M, Burglen L, Bertrand AM, Netchine I, Le Bouc Y 2005 Epimutation of the telomeric imprinting center region on chromosome 11p15 in Silver-Russell syndrome. Nat Genet 37: 1003–1007
Schonherr N, Meyer E, Eggermann K, Ranke MB, Wollmann HA, Eggermann T 2006 (Epi)mutations in 11p15 significantly contribute to Silver-Russell syndrome: but are they generally involved in growth retardation?. Eur J Med Genet 49: 414–418
DeChiara TM, Efstratiadis A, Robertson EJ 1990 A growth-deficiency phenotype in heterozygous mice carrying an insulin-like growth factor II gene disrupted by targeting. Nature 345: 78–80
Constancia M, Hemberger M, Hughes J, Dean W, Ferguson-Smith A, Fundele R, Stewart F, Kelsey G, Fowden A, Sibley C, Reik W 2002 Placental-specific IGF-II is a major modulator of placental and fetal growth. Nature 417: 945–948
Sun FL, Dean WL, Kelsey G, Allen ND, Reik W 1997 Transactivation of Igf2 in a mouse model of Beckwith-Wiedemann syndrome. Nature 389: 809–815
Holmes R, Montemagno R, Jones J, Preece M, Rodeck C, Soothill P 1997 Fetal and maternal plasma insulin-like growth factors and binding proteins in pregnancies with appropriate or retarded fetal growth. Early Hum Dev 49: 7–17
Leger J, Oury JF, Noel M, Baron S, Benali K, Blot P, Czernichow P 1996 Growth factors and intrauterine growth retardation. I. Serum growth hormone, insulin-like growth factor (IGF)-I, IGF-II, and IGF binding protein 3 levels in normally grown and growth-retarded human fetuses during the second half of gestation. Pediatr Res 40: 94–100
Giudice LC, de Zegher F, Gargosky SE, Dsupin BA, de las Fuentes L, Crystal RA, Hintz RL, Rosenfeld RG 1995 Insulin-like growth factors and their binding proteins in the term and preterm human fetus and neonate with normal and extremes of intrauterine growth. J Clin Endocrinol Metab 80: 1548–1555
Street ME, Seghini P, Fieni S, Ziveri MA, Volta C, Martorana D, Viani I, Gramellini D, Bernasconi S 2006 Changes in interleukin-6 and IGF system and their relationships in placenta and cord blood in newborns with fetal growth restriction compared with controls. Eur J Endocrinol 155: 567–574
Osorio M, Torres J, Moya F, Pezzullo J, Salafia C, Baxter R, Schwander J, Fant M 1996 Insulin-like growth factors (IGFs) and IGF binding proteins-1, -2, and -3 in newborn serum: relationships to fetoplacental growth at term. Early Hum Dev 46: 15–26
Christou H, Connors JM, Ziotopoulou M, Hatzidakis V, Papathanassoglou E, Ringer SA, Mantzoros CS 2001 Cord blood leptin and insulin-like growth factor levels are independent predictors of fetal growth. J Clin Endocrinol Metab 86: 935–938
Wiznitzer A, Reece EA, Homko C, Furman B, Mazor M, Levy J 1998 Insulin-like growth factors, their binding proteins, and fetal macrosomia in offspring of nondiabetic pregnant women. Am J Perinatol 15: 23–28
Lassarre C, Hardouin S, Daffos F, Forestier F, Frankenne F, Binoux M 1991 Serum insulin-like growth factors and insulin-like growth factor binding proteins in the human fetus. Relationships with growth in normal subjects and in subjects with intrauterine growth retardation. Pediatr Res 29: 219–225
Ong K, Kratzsch J, Kiess W, Costello M, Scott C, Dunger D 2000 Size at birth and cord blood levels of insulin, insulin-like growth factor I (IGF-I), IGF-II, IGF-binding protein-1 (IGFBP-1), IGFBP-3, and the soluble IGF-II/mannose-6-phosphate receptor in term human infants. The ALSPAC Study Team. Avon Longitudinal Study of Pregnancy and Childhood. J Clin Endocrinol Metab 85: 4266–4269
Stead JD, Hurles ME, Jeffreys AJ 2003 Global haplotype diversity in the human insulin gene region. Genome Res 13: 2101–2111
Le Stunff C, Fallin D, Bougneres P 2001 Paternal transmission of the very common class I INS VNTR alleles predisposes to childhood obesity. Nat Genet 29: 96–99
Huxtable SJ, Saker PJ, Haddad L, Walker M, Frayling TM, Levy JC, Hitman GA, O'Rahilly S, Hattersley AT, McCarthy MI 2000 Analysis of parent-offspring trios provides evidence for linkage and association between the insulin gene and type 2 diabetes mediated exclusively through paternally transmitted class III variable number tandem repeat alleles. Diabetes 49: 126–130
Dunger DB, Ong KK, Huxtable SJ, Sherriff A, Woods KA, Ahmed ML, Golding J, Pembrey ME, Ring S, Bennett ST, Todd JA 1998 Association of the INS VNTR with size at birth. ALSPAC Study Team. Avon Longitudinal Study of Pregnancy and Childhood. Nat Genet 19: 98–100
Lindsay RS, Hanson RL, Wiedrich C, Knowler WC, Bennett PH, Baier LJ 2003 The insulin gene variable number tandem repeat class I/III polymorphism is in linkage disequilibrium with birth weight but not Type 2 diabetes in the Pima population. Diabetes 52: 187–193
McMurtry JP, Francis GL, Upton FZ, Rosselot G, Brocht DM 1994 Developmental changes in chicken and turkey insulin-like growth factor-I (IGF-I) studied with a homologous radioimmunoassay for chicken IGF-I. J Endocrinol 142: 225–234
Breier BH, Gallaher BW, Gluckman PD 1991 Radioimmunoassay for insulin-like growth factor-I: solutions to some potential problems and pitfalls. J Endocrinol 128: 347–357
Zar JH 1999 Biostatistical Analysis. Prentice-Hall, Englewood Cliffs, NJ, pp 431–433
Ambrosius WT, Lange EM, Langefeld CD 2004 Power for genetic association studies with random allele frequencies and genotype distributions. Am J Hum Genet 74: 683–693
Lewontin RC 1964 The interaction of selection and linkage. I. General considerations; heterotic models. Genetics 49: 49–67
Harrela M, Koistinen H, Kaprio J, Lehtovirta M, Tuomilehto J, Eriksson J, Toivanen L, Koskenvuo M, Leinonen P, Koistinen R, Seppala M 1996 Genetic and environmental components of interindividual variation in circulating levels of IGF-I, IGF-II, IGFBP-1, and IGFBP-3. J Clin Invest 98: 2612–2615
Paquette J, Giannoukakis N, Polychronakos C, Vafiadis P, Deal C 1998 The INS 5′ variable number of tandem repeats is associated with IGF2 expression in humans. J Biol Chem 273: 14158–14164
Moore GE, Abu-Amero SN, Bell G, Wakeling EL, Kingsnorth A, Stanier P, Jauniaux E, Bennett ST 2001 Evidence that insulin is imprinted in the human yolk sac. Diabetes 50: 199–203
Adkins R, Krushkal J, Klauser CK, Magann EF, Morrison JC, Somes G Accepted Association between small for gestational age and paternally inherited 5′ insulin haplotypes. Int J Obesity, in press
Kralovicova J, Gaunt TR, Rodriguez S, Wood PJ, Day IN, Vorechovsky I 2006 Variants in the human insulin gene that affect pre-mRNA splicing: is -23HphI a functional single nucleotide polymorphism at IDDM2?. Diabetes 55: 260–264
Gaunt TR, Cooper JA, Miller GJ, Day IN, O'Dell SD 2001 Positive associations between single nucleotide polymorphisms in the IGF2 gene region and body mass index in adult males. Hum Mol Genet 10: 1491–1501
Gu D, O'Dell SD, Chen XH, Miller GJ, Day IN 2002 Evidence of multiple causal sites affecting weight in the IGF2-INS-TH region of human chromosome 11. Hum Genet 110: 173–181
O'Dell SD, Miller GJ, Cooper JA, Hindmarsh PC, Pringle PJ, Ford H, Humphries SE, Day IN 1997 Apal polymorphism in insulin-like growth factor II (IGF2) gene and weight in middle-aged males. Int J Obes Relat Metab Disord 21: 822–825
McIntyre HD, Serek R, Crane DI, Veveris-Lowe T, Parry A, Johnson S, Leung KC, Ho KK, Bougoussa M, Hennen G, Igout A, Chan FY, Cowley D, Cotterill A, Barnard R 2000 Placental growth hormone (GH), GH-binding protein, and insulin-like growth factor axis in normal, growth-retarded, and diabetic pregnancies: correlations with fetal growth. J Clin Endocrinol Metab 85: 1143–1150
Reece EA, Wiznitzer A, Le E, Homko CJ, Behrman H, Spencer EM 1994 The relation between human fetal growth and fetal blood levels of insulin-like growth factors I and II, their binding proteins, and receptors. Obstet Gynecol 84: 88–95
Kubota T, Kamada S, Taguchi M, Aso T 1992 Determination of insulin-like growth factor-2 in feto-maternal circulation during human pregnancy. Acta Endocrinol (Copenh) 127: 359–365
Monk D, Sanches R, Arnaud P, Apostolidou S, Hills FA, Abu-Amero S, Murrell A, Friess H, Reik W, Stanier P, Constancia M, Moore GE 2006 Imprinting of IGF2 P0 transcript and novel alternatively spliced INS-IGF2 isoforms show differences between mouse and human. Hum Mol Genet 15: 1259–1269
Acknowledgements
The authors thank two anonymous reviewers for useful comments to improve the paper. We also thank Laura Bufkin, R.N., Dr. Kimberly Fisher, Sandy Grimes, R.N., for their assistance; Taurus Rogers for subject recruitment; and Jeanette Peeples for technical expertise.
Author information
Authors and Affiliations
Corresponding author
Additional information
This work was supported in part by grants from the Children's Foundation Research Center of Memphis at Le Bonheur Children's Medical Center to R.M.A., the Accredo Foundation to R.M.A. and J.N.F., and the Center of Genomics and Bioinformatics at the University of Tennessee Health Science Center to R.M.A. Additional funds were provided by the University of Tennessee Health Science Center General Clinical Research Center (grant number M01-RR00211).
Rights and permissions
About this article
Cite this article
Adkins, R., Fain, J., Krushkal, J. et al. Association Between Paternally Inherited Haplotypes Upstream of the Insulin Gene and Umbilical Cord IGF-II Levels. Pediatr Res 62, 451–455 (2007). https://doi.org/10.1203/PDR.0b013e3181425841
Received:
Accepted:
Issue Date:
DOI: https://doi.org/10.1203/PDR.0b013e3181425841