Abstract
Previous studies demonstrated that high-frequency oscillatory ventilation using the open lung concept (OLC) resulted in superior gas exchange and a reduction in ventilator-induced lung injury (VILI). We hypothesized that these beneficial effects could also be achieved by applying the OLC during positive pressure ventilation. After repeated whole-lung-lavage, newborn piglets were assigned to either OLC positive pressure ventilation (PPVOLC), OLC high-frequency oscillatory ventilation (HFOVOLC), or conventional positive pressure ventilation (PPVCON) and ventilated for 5 h. In both OLC groups, collapsed alveoli were actively recruited and thereafter stabilized using the lowest possible airway pressures. In the PPVCON group, ventilator settings were adjusted to prevent critical hypoxia. Airway pressure, blood gas analysis, pressure-volume curve, and alveolar protein infiltration was recorded. A lung injury score was used for histologic comparison. Mean airway pressures were comparable in the three ventilation groups over time (1.2-1.5 kPa). Arterial oxygenation increased to mean values above 60 kPa in both OLC groups compared with 10 kPa in the PPVCON group (p < 0.001). Maximal lung compliance was superior in both OLC groups (PPVOLC: 91 ± 23; HFOVOLC: 90 ± 31 mL/kPa/kg, p < 0.01) compared with the PPVCON group (39 ± 14 mL/kPa/kg). Alveolar protein infiltration was significantly reduced in the PPVOLC group (0.33 ± 0.10 mg/mL, p < 0.01) and the HFOVOLC group (0.40 ± 0.13 mg/mL, p < 0.01) compared with the PPVCON group (0.70 ± 0.15 mg/mL). Lung injury scores were significantly higher in the PPVCON group (33.5 ± 9.5, p < 0.01) compared with both OLC groups (PPVOLC: 10.5 ± 2.6; HFOVOLC: 11 ± 2.2). There were no differences between the two OLC groups. We conclude that, in surfactant-depleted newborn piglets, application of the OLC during PPV is feasible and results in superior gas exchange and a reduction in VILI compared with conventional PPV. These beneficial effects are comparable to HFOV.
Similar content being viewed by others
Main
Acute respiratory failure in newborn infants is often caused by surfactant deficiency and/or inactivation. These changes in surfactant result in alveolar collapse and subsequent hypoxia and hypercapnia. Treatment with conventional PPV is often indicated, but, in the attempt to optimize gas exchange, PPV often leads to secondary lung injury, also referred to as VILI (1). This may contribute to long-term respiratory morbidity (chronic lung disease), especially in newborn infants (2).
Animal studies have shown that alveolar overdistension (volutrauma) and cyclic reopening of alveoli collapsed during expiration (atelectrauma) are the major causes of VILI (3, 4). During HFOV, alveolar overdistension is prevented by the use of small tidal volumes superimposed on a relatively high CDP to maintain adequate lung volume. However, animal studies have shown that this approach will only result in a reduction of VILI if alveoli are optimally recruited at the start of ventilation (5, 6).
The ventilation strategy based on these three important principles of lung protective ventilation (alveolar recruitment, prevention of alveolar overdistention and collapse) is also referred to as the high-volume strategy or the OLC (7–9).
In contrast to HFOV, the OLC during PPV has not been investigated in newborn animals or infants. Adult animal studies showed that PPV can effectively recruit alveoli and keep them open during the entire respiratory cycle (10). To accomplish this, PIP are increased for a short period of time to recruit collapsed alveoli and, subsequently, alveolar collapse and overdistension is prevented by sufficient amounts of PEEP and by using small pressure amplitudes (PIP - PEEP). Studies in adult patients treated for acute respiratory failure showed promising results (11).
Based on these findings, we decided to investigate the OLC during PPV (PPVOLC) in a surfactant-deficient newborn animal model. PPVOLC was compared with both conventional PPV (PPVCON) and HFOV (HFOVOLC), because these latter two strategies are mostly used in neonates (12–14). Primary outcome parameters in this comparison were gas exchange and VILI. Secondary outcome parameters were changes in ventilatory pressures and hemodynamics. We hypothesized that PPVOLC would lead to superior gas exchange and less VILI compared with PPVCON. Superior gas exchange was defined as improved oxygenation while preventing hypercapnia. A reduction in VILI was defined as a preservation of compliance, total lung capacity, and alveolar stability (lung mechanics); a decrease in alveolar protein influx; and a decrease in histologic evidence of lung injury expressed as a semiquantitative score. We further hypothesized that the magnitude of these beneficial effects on gas exchange and VILI would be comparable to HFOVOLC.
METHODS
Animal Preparation
These experiments were performed at the Department of Anesthesiology, Erasmus University Rotterdam. The study was approved by the institutional animal investigation committee.
Anesthesia was induced in 45 mixed-breed newborn piglets, aged 23 ± 15 h (mean ± SD) and weighing 1.4 ± 0.3 kg, with ketamine hydrochloride [35 mg/kg intramuscularly (i.m.)] and midazolam (0.5 mg/kg i.m.). The animals were tracheotomized, connected to a Servo ventilator 300 (Siemens-Elema, Solna, Sweden) and ventilated in the pressure-controlled timecycled mode, at a FiO2 concentration of 1.0, a rate of 25-30 breaths/min, PIP of 0.9-1.2 kPa (9-12 cm H2O), PEEP of 0.2 kPa (2 cm H2O), and an I/E ratio of 1:2. A neuromuscular block was induced with pancuronium bromide (0.5 mg/kg i.v.), followed by a continuous infusion of fentanyl (20 μg/kg/h), midazolam (0.3 mg/kg/h), and pancuronium bromide (0.3 mg/kg/h).
A 4-Fr double-lumen polyurethane catheter (Vygon, Ecouen, France) was introduced through the external jugular vein for measurement of CVP and infusion of fluids and medication. The carotid artery was cannulated for monitoring of blood pressure and blood sampling. In addition, a sensor for continuous blood gas monitoring (Paratrend/Trendcare, Philips Medical, Böblingen, Germany) was inserted through a femoral artery catheter.
A continuous infusion of 5% dextrose was started (100 mL/kg/d) and all animals received one dose of cefotaxime (100 mg/kg). Body temperature was kept between 38° and 39°C during the experiment.
Surfactant Depletion
After the instrumentation period, respiratory failure was induced by repeated saline lavage (50 mL/kg; 37°C) as described by Lachmann et al. (15). The first five lavages were performed in the prone position, after which the animals were placed in a supine position for the remainder of the lavage procedure. Lavages were repeated at 3-min interval until PaO2 was below 10.7 kPa and PaCO2 above 5.3 kPa at the following ventilator settings: PIP/PEEP, 2.45/0.49 kPa (25/5 cm H2O); rate, 40 breaths/min; I/E ratio, 1:2; and FiO2, 1.0.
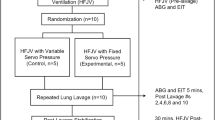
Experimental Protocol
Immediately after induction of anesthesia, five animals were killed and served as a healthy nonventilated control group. An additional group of four animals was killed immediately after the lavage procedure and served as histologic controls.
Within 10 min after the last lavage, the remaining animals were randomly allocated (T = 0 h) to one of the three treatment groups (n = 12 each) and ventilated for a period of 5 h. FiO2 was kept at 1.0 during all experiments.
PPVOLC group.
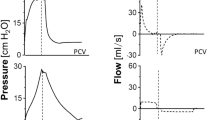
In this group, the ventilatory rate was increased to 120 breaths/min with an I/E ratio of 1:1. These settings remained unchanged during the experiment. PEEP was increased to 1.47 kPa (15 cm H2O) and PIP was stepwise increased [0.49 kPa (5 cm H2O) each step] to open up the lung. Recruitment of previously collapsed alveoli during this procedure will decrease intrapulmonary shunt and thus increase oxygenation (Fig. 1). Based on PaO2 levels in the healthy piglets, ventilated with an FiO2 of 1.0, we defined optimal alveolar recruitment as a PaO2 ≥ 60 kPa. The level of PIP needed to recruit the lung was called the opening pressure (PIPO).
Registration from a single representative experiment showing continuous measurement of arterial PaO2 (mm Hg) and PaCO2 (mm Hg) during the lung recruitment phase in the PPVOLC group. Numbers indicate the actual peak inflation pressures (cm H2O) used in stepwise recruitment of the lung. Each increase is followed by an increase in PaO2 and a decrease in PaCO2 over time. To convert mm Hg to kPa, divide by 7.5.
After this recruitment procedure, PIP and PEEP were simultaneously decreased in equal steps every 2 to 3 min until PaO2 dropped below 60 kPa, indicating increased intrapulmonary shunting due to alveolar collapse. The level of PEEP at this stage of alveolar collapse was called the closing pressure (PEEPC). PEEP was then raised to a level of 0.2 kPa (2 cm H2O) above PEEPC and PIP was momentarily (about 10 s) raised to PIPO to fully recruit the lung. Then, the pressure amplitude was set to keep the PaCO2 within the target range (4-6 kPa). PEEP was only decreased if there were signs of alveolar overdistension defined as increasing PaCO2, decreasing PaO2, or decreasing blood pressure. After 5 h of ventilation, PIPO and PEEPC were once again determined (T = 5 h).
HFOVOLC group.
Animals in this group were ventilated with HFOV (model 3100; SensorMedics Critical Care, Yorba Linda, CA, U.S.A.) using a frequency of 10 Hz and an I/E ratio of 1:2. These settings remained unchanged throughout the experiment. Opening and closing pressures (CDPO and CDPC, respectively) were determined as described in the PPVOLC group, by adjusting the CDP. The delta pressure during oscillation was set at a level that kept the PaCO2 within the target range. CDP was only decreased if there were signs of alveolar overdistension as described earlier. After 5 h of ventilation, CDPO and CDPC were once again determined (T = 5 h).
PPVCON group.
In this third group, animals were ventilated in the pressure-controlled mode, applying a conventional strategy. As preliminary experiments showed that it was not possible to achieve a target PaO2 ≥ 60 kPa, the ventilator settings after the lavage procedure were adjusted to prevent critical hypoxia (PaO2 < 8 kPa). First, the I/E ratio was set at 1:1 and, if necessary, PIP was increased with a limit of 3.43 kPa (35 cm H2O). If the level of PIP exceeded 2.94 kPa (30 cm H2O), PEEP was increased to 0.59 kPa (6 cm H2O).
The rate was preferentially changed (between 25 and 60 breaths/min) to keep the PaCO2 within the target range. If adjusting the rate proved unsuccessful in controlling PaCO2, PIP could be altered as long as the changes did not compromise PaO2.
During the experimental period, intravascular volume expansion (albumin 5%; 10 mL/kg/dose) was initiated if there were two or more signs of circulatory failure: heart rate > 200 beats/min, mean arterial blood pressure < 6.7 kPa (50 mm Hg), and deteriorating PaO2 (> 10%).
Mean arterial blood pressure, heart rate, CVP, ventilator settings, and pressures were recorded at the end of the instrumentation period, at the end of the lavage procedure, and hourly after randomization. Although blood gas values were recorded continuously, reference samples were drawn at these same time points (ABL 505, Radiometer, Copenhagen, Denmark).
Pressure-Volume Curves
After the 5 h ventilation period, eight animals in each treatment group were killed by an overdose of pentobarbital and used to assess lung mechanics. Static pressure-volume (P/V) curves were recorded using the syringe technique as previously described (16). In short, after opening the thorax and diaphragm, the endotracheal tube was connected to a pressure transducer with a syringe attached to it (model DP 45-32, Validyne Engineering, Northridge, CA, U.S.A.), and pressures were recorded on a polygraph (model 7B, Grass Instruments, Quincy, MA, U.S.A.). Using a syringe, the lungs were first inflated using steps of 1 mL up to a volume of 10 mL and thereafter steps of 5 mL until an airway pressure of 3.43 kPa (35 cm H2O) was reached. The lungs were deflated in the same manner starting with 1-mL steps, followed by 5-mL steps until the airway pressure reached 0 kPa.
Crsmax was calculated from the maximal slope on the deflation limb (17). Total lung capacity (TLC) was defined as lung volume at inflation with a distending pressure of 3.43 kPa (35 cm H2O). The Gruenwald index, which characterizes the surfactant system in situ, was calculated from the P/V curve, defined as (2V5 + V10)/2Vmax, where V5, V10, and Vmax are the lung volumes at transpulmonary pressures of 0.49, 0.98, and 3.43 kPa (5, 10, and 35 cm H2O), respectively, on the deflation limb (18).
Bronchoalveolar Lavage Procedure
After recording P/V curves, bronchoalveolar lavage was performed five times (40 mL/kg) with saline-CaCl2 1.5 mM. The recovered fluids from these five lavages were pooled and analyzed as one sample. The percentage of lung lavage fluid recovered was calculated. Samples were centrifuged for 10 min at 1500 g to remove cell material, and protein concentration was measured using the Bradford method (protein assay, Bio-Rad, Munich, Germany) (19).
Lung mechanics and alveolar protein infiltration as described above were also assessed in the healthy nonventilated control group
Histologic Processing
At the end of the experiment, the lungs of the four remaining animals in each ventilation group and in the histologic control group were fixated as previously described (20). Briefly, after perfusion, the lung was fixated with a solution consisting of 3.6% formaldehyde and 0.25% glutaraldehyde. Before fixation, the airway pressure was momentarily increased to 2.94 kPa (30 cm H2O) and thereafter maintained at 1.96 kPa (20 cm H2O).
Blocks of tissue were taken from the center of the upper and middle lobe and from the ventral and dorsal part of the lower lobe. The specimens were embedded in paraffin, sectioned, and stained with hematoxylin and eosin.
A semiquantitative morphometric analysis of lung injury was performed under blinded conditions, scoring atelectasis, hyaline membrane formation, and cellular infiltration as none, minimal, light, moderate, or severe (scores 0, 1, 2, 3, or 4, respectively). As there were no differences in lung injury scores between the left and right lung, only the right lung was used for further analysis. The lung injury score for each lung was defined as the sum of all four segments taken (maximum score 48). The total lung injury score for the different treatment groups was obtained by averaging the lung injury scores from the animals included in each group.
Statistical Analysis
Statistical analysis was performed using SPSS version 10 (SPSS, Chicago, IL, U.S.A.). Intergroup differences were analyzed with ANOVA or the t test. If ANOVA resulted in p < 0.05, a Bonferroni posthoc test was performed. Intragroup comparisons were analyzed with the paired t test. Lung injury data were analyzed after logarithmic transformation. A p value < 0.05 was considered statistically significant.
RESULTS
All animals survived the study period. There were no intergroup differences in age, weight, or number of lavages (14 ± 4 SD) needed to induce lung injury. No air leaks were observed during the study period. Blood gas values before and immediately after lavage were comparable in the three treatment groups.
Mean PaO2 values increased after the recruitment maneuver in the PPVOLC and HFOVOLC groups and remained significantly higher than in the PPVCON group at all time points (Fig. 2A).
Changes (mean ± SD) in PaO2 (A) and PaCO2 (B) before lung lavage (H), after lung lavage (L), and during the 5-h ventilation period in the three ventilation groups (PPVOLC, squares; HFOVOLC, circles; PPVCON, triangles). *p < 0.001, †p < 0.01, ‡p < 0.05 vs PPVCON group. To convert to mm Hg, multiply by 7.5.
PaCO2 decreased in all ventilation groups after randomization, but was significantly lower in the PPVCON group compared with the PPVOLC and HFOVOLC group (Fig. 2B). Because PaCO2 gradually increased over time in the PPVCON group, this difference in PaCO2 was no longer significant versus the HFOVOLC group during the last 2 h of the study period.
The MawP in both PPV groups and the CDP in the HFOV group showed no significant differences between ventilation groups during the entire experiment (Table 1). A higher level of PEEP and a lower level of PIP resulted in a significantly smaller pressure amplitude during PPVOLC compared with PPVCON. To establish adequate CO2 removal, the ventilatory rate was significantly higher during PPVOLC compared with PPVCON. It is important to mention that the delta pressure during HFOV as reported in Table 1 represents the values as displayed by the oscillator. Because we did not measure intratracheal pressures, the reported delta pressure cannot be compared with the pressure amplitude measured during PPV.
Comparison of the opening pressures (PIPO and CDPO; Fig. 3A) between both OLC groups revealed no significant differences either at the start (T = 0) or at the end (T = 5) of the ventilation period. This was also true for the closing pressures (PEEPC and CDPC; Fig. 3B). However, analyzing opening and closing pressure within each OLC group separately showed a significant decrease of both parameters over the 5-h ventilation period (T = 0 versus T = 5 h; Fig. 3).
Changes (mean ± SD) in opening (A) and closing (B) pressures immediately after randomization (T = 0 h) and at the end of the 5-h ventilation period (T = 5 h). There is a significant decrease in opening and closing pressures within each ventilation group over time. *p < 0.001 vs T = 0 h. To convert to cm H2O, multiply by 10.2.
With the exception of the CVP, circulatory parameters showed no significant differences between ventilation groups throughout the experiment (Table 2). CVP was significantly higher in the PPVOLC group compared with the PPVCON and HFOVOLC groups during the 5-h ventilation period. There were no significant differences in acid-base status and in the amount of fluid support between the groups (29 ± 15 mL/kg in PPVOLC, 23 ± 21 mL/kg in HFOVOLC, and 18 ± 13 mL/kg in PPVCON).
Figure 4 shows P/V curves of the three ventilation groups. There were no significant differences in lung mechanics between the PPVOLC and the HFOVOLC groups, which were comparable to the nonventilated healthy controls. However, TLC, Crsmax and the Gruenwald index were significantly lower in the PPVCON group compared with the PPVOLC and the HFOVOLC group (Table 3).
Static pressure-volume curves (mean ± SD) in healthy controls (open triangles) and the three ventilation groups (PPVOLC, squares; HFOVOLC, circles; PPVCON, solid triangles). Significant differences are given in Table 3. To convert to cm H2O, multiply by 10.2.
The protein concentration in the bronchoalveolar lavage fluid of the PPVCON group was significantly higher than in both OLC groups (Table 3). Protein concentration in the nonventilated healthy controls was comparable to that in the OLC groups. There were no significant differences between the groups in the amount of bronchoalveolar lavage fluid recovered.
Figure 5 shows the lung injury scores of the different treatment groups. Both PPVOLC and HFOVOLC showed significantly less lung injury than the PPVCON group.
Histologic changes seen in the PPVCON group consisted of large atelectatic areas containing hyaline membranes and a high degree of interstitial cellular infiltration (Fig. 6A). Histologic changes seen in both OLC groups were mainly increased interstitial cellular infiltration (Fig. 6, B and C), resulting in a higher lung injury score compared with the animals that were lavaged only (Fig. 6D). More detailed quantitative comparisons between the two OLC groups were not made.
Sections of lungs stained with hematoxylin-eosin, magnification 50×. (A) Diffuse atelectasis, hyaline membrane formation, and cellular infiltration in the lung of an animal treated with PPVCON. (B) Increased cellular infiltration in the lung of an animal treated with PPVOLC. (C) Increased cellular infiltration in the lung of an animal treated with HFOVOLC. (D) Minimal signs of structural damage to the lung of an animal undergoing lavage only.
DISCUSSION
The present study demonstrates that applying the OLC during PPV in surfactant-depleted newborn piglets optimizes gas exchange and reduces VILI compared with conventional PPV.
Previously, most newborn and adult animal studies investigated the beneficial effects of the OLC during HFOV. Comparison of this ventilation modality with conventional PPV in animals showed the superiority of HFOV with regard to gas exchange and several parameters of VILI (5, 6, 21–23). A recent meta-analysis confirmed these animal findings in human newborn infants with respiratory distress syndrome (24). However, some have stated that it is not the ventilation mode (HFOV or PPV) but the ventilation strategy (OLC) that is responsible for these beneficial effects (7, 25).
Until now, only two studies explored this theory. These latter studies showed that application of the OLC during PPV and HFOV resulted in comparable gas exchange and VILI (16, 26). However, neither of these studies included a conventional PPV group, making direct comparison with this (still widely used) mode of ventilation impossible. Secondly, both studies used adult animal models, which may not be ideal for testing new ventilation modalities in newborns. The newborn lung is both structurally (e.g. gas exchange unit) and biochemically (e.g. surfactant metabolism) different from the adult lung (27, 28). Some believe this makes the newborn lung much more susceptible for VILI than the adult lung (29).
We therefore decided to compare the OLC during PPV and HFOV with conventional PPV in newborn piglets. We chose the newborn piglet because it has a lung morphology similar to that of humans (30, 31).
Acute respiratory failure was induced by whole-lung lavage, which has been postulated to reflect a primary surfactant deficiency, as seen in neonatal respiratory distress syndrome (15).
Our study clearly shows that both PPVOLC and HFOVOLC are able to recruit and maintain adequate lung volume, leading to superior oxygenation compared with the PPVCON group (Fig. 2A). We used arterial oxygenation to determine optimal recruitment as it has been demonstrated that this parameter increases with increasing lung volume (5, 32). We did not measure absolute lung volume because application of this measurement bedside is still unpractical and often not available. Furthermore, a measured increase in lung volume can result from either an increased expansion of already opened alveoli (distension) or opening of previously collapsed alveoli (recruitment). Only arterial oxygenation can differentiate between these two possibilities because only recruitment will reduce intrapulmonary shunting and thus improve PaO2.
As the MawP in the PPVCON group was not different from the PPVOLC group, the relative hypoxia in the PPVCON group was probably caused by inadequate levels of PEEP (unable to prevent end-expiratory alveolar collapse) and the absence of an active recruitment maneuver. This, however, is in accordance with daily practice in the neonatal intensive care unit, where PEEP during PPVCON in newborns seldom exceeds 0.6 kPa (6 cm H2O) and recruitment maneuvers are not performed (7, 33).
Increasing PIP in the PPVCON group resulted in an only modest increase in PaO2. To keep the PIP within a clinically acceptable range and MawP comparable with the OLC groups, a target PaO2 of 8 kPa was used, as described elsewhere (22).
The higher pressure amplitude during PPVCON resulted in a significantly lower mean level of PaCO2 compared with both OLC groups (Fig. 2B). In some animals, it proved difficult to keep PaCO2 within the target range because of progressive hypoxia after lowering PIP. During the 5 h ventilation period, mean PaCO2 levels in the PPVCON group slowly increased, indicating deteriorating pulmonary mechanics. These changes in PaCO2 levels during PPVCON have also been reported in other animal models (22).
Although the pressure amplitude in the PPVOLC group was much lower than in the PPVCON group, mean PaCO2 levels in the PPVOLC group remained stable and within the target range during the ventilation period. Hypercapnia during ventilation with small pressure amplitudes in the PPVOLC group is prevented by more efficient ventilation (less pulmonary shunting) after alveolar recruitment and stabilization, and by increasing ventilatory rate. Although it seems inappropriate to compare two PPV groups with different ventilation settings and adjustments, we have to bear in mind that the present study did not aim to compare different settings but different ventilation strategies. The reported differences in ventilation settings are secondary to the ventilation strategy used and, in our opinion, therefore make the comparison valid.
Recruitment of collapsed alveoli requires inspiratory airway pressures that overcome the critical opening pressures of these alveoli, which implies application of high inspiratory airway pressures for a brief period (10). In the present study, initial mean opening pressures up to 3.92 kPa (40 cm H2O) were needed to recruit collapsed alveoli in both OLC groups. These levels are somewhat higher than previously reported in newborn and adult animals, but, during these latter experiments, lower PaO2/FiO2 ratios were used to define a fully recruited lung (5, 22). Once again, similar to those previous reports, our study shows that the use of such high pressures are essential to fully recruit the lung and, more important, that these high-pressure levels themselves do not lead to additional VILI if applied for a short period of time.
Closing pressures in both OLC groups were much lower than the opening pressures. This phenomena can be explained by the law of LaPlace, which states that because of the increase of its radius, a recruited alveolus will require a lower airway pressure level to prevent alveolar collapse (8, 9).
Determination of opening and closing pressures at the end of the ventilation period showed a significant decrease in both OLC groups, indicating increased alveolar stability. This finding is in accordance with the superior lung mechanics (TLC, Crsmax, and Gruenwald index) found in the PPVOLC and the HFOVOLC group at the end of the ventilation period (Table 3). Comparing both OLC groups to nonventilated healthy controls showed no significant differences in pulmonary mechanics after 5 h of ventilation.
These findings suggest that, during this short ventilation period, the lung of the newborn piglet is capable of regaining alveolar stability comparable to the healthy nonlavaged lung. One possible explanation could be an increased secretion of endogenous surfactant. Others have shown that stretching but not overdistending the alveoli can stimulate surfactant secretion, thus increasing alveolar stability (34). However, as we did not measure surfactant activity in the present study, we cannot substantiate this possibility.
The fact that, in contrast to both OLC groups, lung function did deteriorate in the PPVCON group could be explained by the increased alveolar influx of protein. Besides being an important indicator for VILI, protein infiltrating the alveolar space is considered one of the important inhibitors of surfactant (35, 36). We found protein levels in broncho-alveolar lavage of both the OLC groups to be comparable to healthy nonventilated controls (Table 3). In contrast, alveolar protein levels in the PPVCON group were significantly increased after 5 h of ventilation.
The histologic changes found in the PPVCON group are consistent with this increase in alveolar protein infiltration and deterioration of lung mechanics (Fig. 5). The higher degree of atelectasis, hyaline membrane formation, and interstitial cellular infiltration in the PPVCON group could be considered the start of alveolar and interstitial inflammation, currently considered one of the most important pathways for developing chronic lung disease of the newborn (29, 37).
The fact that the lung injury scores in both the OLC groups were higher than lavaged histologic controls once again shows that, independent of the strategy used, mechanical ventilation will always result in some degree of VILI in the surfactantdepleted lung. However, by applying the OLC during mechanical ventilation, the amount of VILI can be markedly reduced.
This optimization of gas exchange and the attenuation of VILI found in our study are consistent with earlier reports exploring the OLC during both HFOV and PPV, adding more evidence to the superiority of OLC ventilation and to the fact that the ventilation strategy is probably more important than the type of ventilator used (5, 6, 16, 22, 23, 26).
Which aspect of the OLC contributes most to the differences between both OLC groups and the PPVCON group cannot be answered by the present study. The aim of our study was to compare the OLC during PPV with conventional PPV as used in daily practice in the treatment of acute respiratory failure in neonates. However, based on previous studies it is reasonable to assume that all mentioned aspects of the OLC contribute to some extent to optimization of gas exchange and the reduction of VILI. Rimensberger et al. (38) clearly showed that, during PPV using optimal PEEP and small tidal volumes, application of a sustained inflation is essential in preventing deterioration of lung function. This beneficial effect of a sustained inflation on lung function during low tidal volume PPV was also reported by Bond et al. (39). On the other hand, McCulloch et al. (5) reported the importance of maintaining adequate lung volume after a recruitment maneuver during HFOV. Finally, Froese et al. (40) showed that establishing an adequate endexpiratory lung volume by using high tidal volumes and suboptimal levels of PEEP during PPV will only result in a temporary improvement in gas exchange followed by deteriorating oxygenation and lung condition.
Recent studies have shown that hypercapnia can attenuate lung injury whereas hypocapnia may increase lung injury (41–43). Although these experiments were performed in isolated perfused lungs with PaCO2 levels in the extreme limits, we cannot rule out that the differences in PaCO2 reported in the present study influenced the differences in VILI. Future in vivo experiments should further clarify whether PaCO2 also influences lung injury if levels are closer to the normal range and differences are small, as in the present study.
Several studies reported no hemodynamic differences between HFOV and conventional PPV (22, 44); our study confirms these findings. However, in our PPVOLC group, CVP was significantly higher than in the other two groups (Table 2). We can only speculate on the reasons for this difference. Because no differences were found in blood pressure, heart rate, and acid-base status, cardiac failure is unlikely to have caused this rise in CVP. Furthermore, the amount of volume expansion did not differ between the three groups.
Although not statistically significant, there was a clear trend to higher CVP values in the PPVOLC group before randomization (healthy and lavaged), which could in part explain the differences found during the ventilation period. The difference could also be explained by the higher PEEP level in the PPVOLC group compared with the PPVCON group. However, the fact that the high CDP during HFOVOLC did not result in an increased CVP seems to weaken this explanation. Nevertheless, the question whether CVP is also influenced by the ventilation mode remains to be answered in future studies using more invasive hemodynamic monitoring.
In conclusion, the present study shows for the first time in a surfactant-depleted newborn animal model that applying the OLC during PPV is feasible, and results in superior gas exchange and a reduction in VILI compared with conventional PPV. Furthermore, the magnitude of these beneficial effects is comparable to HFOV. These results are important in those clinical situations where HFOV is not an option or is limited due to the lack of availability of proper equipment.
As the present study only explored the short-term effects of PPVOLC, future animal studies should investigate long-term effects on gas exchange and VILI.
Furthermore, application of PPVOLC in different animal models of neonatal lung injury, may identify which infants will benefit most from this ventilation strategy. Depending on these results, implementation by randomized controlled trials in human newborn infants should be the next step and OLC PPV as described here should not be applied clinically outside controlled studies.
Abbreviations
- PPV:
-
positive pressure ventilation
- HFOV:
-
high-frequency oscillatory ventilation
- OLC:
-
open lung concept
- VILI:
-
ventilator-induced lung injury
- MawP:
-
mean airway pressure
- PIP:
-
peak inspiratory pressure
- PEEP:
-
positive end-expiratory pressure
- I/E:
-
inspiration/expiration time
- CDP:
-
continuous distending pressure
- FiO2:
-
fraction of inspired oxygen
- PaO2:
-
arterial PO2
- PaCO2:
-
arterial PCO2
- Crsmax:
-
maximal lung compliance
- TLC:
-
total lung capacity
- CVP:
-
central venous pressure
REFERENCES
Dreyfuss D, Saumon G 1998 Ventilator-induced lung injury: lessons from experimental studies. Am J Respir Crit Care Med 157: 294–323.
Farrell PA, Fiascone JM 1997 Bronchopulmonary dysplasia in the 1990s: a review for the pediatrician. Curr Probl Pediatr 27: 129–163.
Dreyfuss D, Soler P, Basset G, Saumon G 1988 High inflation pressure pulmonary edema. Respective effects of high airway pressure, high tidal volume, and positive end-expiratory pressure. Am Rev Respir Dis 137: 1159–1164.
Taskar V, John J, Evander E, Robertson B, Jonson B 1997 Surfactant dysfunction makes lungs vulnerable to repetitive collapse and reexpansion. Am J Respir Crit Care Med 155: 313–320.
McCulloch PR, Forkert PG, Froese AB 1988 Lung volume maintenance prevents lung injury during high frequency oscillatory ventilation in surfactant-deficient rabbits. Am Rev Respir Dis 137: 1185–1192.
Hamilton PP, Onayemi A, Smyth JA, Gillan JE, Cutz E, Froese AB, Bryan AC 1983 Comparison of conventional and high-frequency ventilation: oxygenation and lung pathology. J Appl Physiol 55: 131–138.
Thome U, Kössel H, Lipowsky G, Porz F, Fürste HO, Genzel BO, Tröger J, Oppermann HC, Högel J, Pohlandt F 1999 Randomized comparison of highfrequency ventilation with high-rate intermittent positive pressure ventilation in preterm infants with respiratory failure. J Pediatr 135: 39–46.
Lachmann B 1992 Open up the lung and keep the lung open. Intensive Care Med 18: 319–321.
Bohm SH, Vazquez de Anda GF, Lachmann B 1998 The open lung concept. In: Vincent JL (ed) Yearbook of Intensive Care and Emergency Medicine. Springer-Verlag, Berlin, 430–440.
Lachmann B, Jonson B, Lindroth M, Robertson B 1982 Modes of artificial ventilation in severe respiratory distress syndrome. Lung function and morphology in rabbits after wash-out of alveolar surfactant. Crit Care Med 10: 724–732.
Amato MB, Barbas CS, Medeiros DM, Magaldi RB, Schettino GP, Lorenzi FG, Kairalla RA, Deheinzelin D, Munoz C, Oliveira R, Takagaki TY, Carvalho CR 1998 Effect of a protective-ventilation strategy on mortality in the acute respiratory distress syndrome. N Engl J Med 338: 347–354.
Horbar JD (ed) 2000 The Vermont Oxford Network 1999 Database Summary. Burlington, Vermont Oxford Network
Egreteau L, Pauchard JY, Semama DS, Matis J, Liska A, Romeo B, Cneude F, Hamon I, Truffert P 2001 Chronic oxygen dependency in infants born at less than 32 weeks' gestation: incidence and risk factors. Pediatrics 108:E26.
Lotze A, Mitchell BR, Bulas DI, Zola EM, Shalwitz RA, Gunkel JH 1998 Multicenter study of surfactant (beractant) use in the treatment of term infants with severe respiratory failure. Survanta in Term Infants Study Group. J Pediatr 132: 40–47.
Lachmann B, Robertson B, Vogel J 1980 In vivo lung lavage as an experimental model of the respiratory distress syndrome. Acta Anaesthesiol Scand 24: 231–236.
Vázquez de Anda GF, Hartog A, Verbrugge SJ, Gommers D, Lachmann B 1999 The open lung concept: pressure-controlled ventilation is as effective as high-frequency oscillatory ventilation in improving gas exchange and lung mechanics in surfactantdeficient animals. Intensive Care Med 25: 990–996.
Hickling KG 2001 Best compliance during a decremental, but not incremental, positive end-expiratory pressure trial is related to open-lung positive end-expiratory pressure: a mathematical model of acute respiratory distress syndrome lungs. Am J Respir Crit Care Med 163: 69–78.
Gruenwald P 1963 A numerical index of the stability of lung expansion. J Appl Physiol 18: 665–667.
Bradford MM 1976 A rapid and sensitive method for the quantitation of microgram quantities of protein utilizing the principle of protein-dye binding. Anal Biochem 72: 248–254.
Gommers D, Hartog A, Schnabel R, De Jaegere A, Lachmann B 1999 High-frequency oscillatory ventilation is not superior to conventional mechanical ventilation in surfactant-treated rabbits with lung injury. Eur Respir J 14: 738–744.
Delemos RA, Coalson JJ, Gerstmann DR, Null DM, Ackerman NB, Escobedo MB, Robotham JL, Kuehl TJ 1987 Ventilatory management of infant baboons with hyaline membrane disease: the use of high frequency ventilation. Pediatr Res 21: 594–602.
Meredith KS, Delemos RA, Coalson JJ, King RJ, Gerstmann DR, Kumar R, Kuehl TJ, Winter DC, Taylor A, Clark RH 1989 Role of lung injury in the pathogenesis of hyaline membrane disease in premature baboons. J Appl Physiol 66: 2150–2158.
Jackson JC, Truog WE, Standaert TA, Juul SE, Murphy JH, Chi EY, Mackenzie AP, Hodson WA 1991 Effect of high-frequency ventilation on the development of alveolar edema in premature monkeys at risk for hyaline membrane disease. Am Rev Respir Dis 143: 865–871.
Cools F, Offringa M 1999 Meta-analysis of elective high frequency ventilation in preterm infants with respiratory distress syndrome. Arch Dis Child Fetal Neonatal Ed 80:F15–F20.
Jobe AH 1998 Too many unvalidated new therapies to prevent chronic lung disease in preterm infants. J Pediatr 132: 200–202.
Rimensberger PC, Pache JC, McKerlie C, Frndova H, Cox PN 2000 Lung recruitment and lung volume maintenance: a strategy for improving oxygenation and preventing lung injury during both conventional mechanical ventilation and high-frequency oscillation. Intensive Care Med 26: 745–755.
Hodson WA, Bancalari E 1998 Normal and abnormal structural development of the lung. In: Polin RA, Fox WW (Eds) Fetal and neonatal physiology. W.B. Saunders, Philadelphia, 1033–1037.
Jobe AH, Ikegami M 1993 Surfactant metabolism. Clin Perinatol 20: 683–696.
Jobe AH, Ikegami M 1998 Mechanisms initiating lung injury in the preterm. Early Hum Dev 53: 81–94.
Bartlett D, Areson JG 1977 Quantitative lung morphology in newborn mammals. Respir Physiol 29: 193–200.
Rendas A, Branthwaite M, Reid L 1978 Growth of pulmonary circulation in normal pig—structural analysis and cardiopulmonary function. J Appl Physiol 45: 806–817.
Suzuki H, Papazoglou K, Bryan AC 1992 Relationship between PaO2 and lung volume during high frequency oscillatory ventilation. Acta Paediatr Jpn 34: 494–500.
Gerstmann DR, Minton SD, Stoddard RA, Meredith KS, Monaco F, Bertrand JM, Battisti O, Langhendries JP, Francois A, Clark RH 1996 The Provo multicenter early high-frequency oscillatory ventilation trial: improved pulmonary and clinical outcome in respiratory distress syndrome. Pediatrics 98: 1044–1057.
Wirtz H, Schmidt M 1992 Ventilation and secretion of pulmonary surfactant. Clin Investig 70: 3–13.
Kobayashi T, Nitta K, Ganzuka M, Inui S, Grossmann G, Robertson B 1991 Inactivation of exogenous surfactant by pulmonary edema fluid. Pediatr Res 29: 353–356.
Lachmann B, Eijking EP, So KL, Gommers D 1994 In vivo evaluation of the inhibitory capacity of human plasma on exogenous surfactant function. Intensive Care Med 20: 6–11.
Speer CP 1999 Inflammatory mechanisms in neonatal chronic lung disease. Eur J Pediatr 158( Suppl 1): S18–S22.
Rimensberger PC, Pristine G, Mullen BM, Cox PN, Slutsky AS 1999 Lung recruitment during small tidal volume ventilation allows minimal positive end-expiratory pressure without augmenting lung injury. Crit Care Med 27: 1940–1945.
Bond DM, McAloon J, Froese AB 1994 Sustained inflations improve respiratory compliance during high-frequency oscillatory ventilation but not during large tidal volume positive-pressure ventilation in rabbits. Crit Care Med 22: 1269–1277.
Froese AB, McCulloch PR, Sugiura M, Vaclavik S, Possmayer F, Moller F 1993 Optimizing alveolar expansion prolongs the effectiveness of exogenous surfactant therapy in the adult rabbit. Am Rev Respir Dis 148: 569–577.
Laffey JG, Tanaka M, Engelberts D, Luo X, Yuan S, Tanswell AK, Post M, Lindsay T, Kavanagh BP 2000 Therapeutic hypercapnia reduces pulmonary and systemic injury following in vivo lung reperfusion. Am J Respir Crit Care Med 162: 2287–2294.
Laffey JG, Engelberts D, Kavanagh BP 2000 Injurious effects of hypocapnic alkalosis in the isolated lung. Am J Respir Crit Care Med 162: 399–405.
Broccard AF, Hotchkiss JR, Vannay C, Markert M, Sauty A, Feihl F, Schaller MD 2001 Protective effects of hypercapnic acidosis on ventilator-induced lung injury. Am J Respir Crit Care Med 164: 802–806.
Kinsella JP, Gerstmann DR, Clark RH, Null DM Jr, Morrow WR, Taylor AF, Delemos RA 1991 High-frequency oscillatory ventilation versus intermittent mandatory ventilation: early hemodynamic effects in the premature baboon with hyaline membrane disease. Pediatr Res 29: 160–166.
Acknowledgements
The authors thank S. Krabbendam (Department of Anesthesiology, Erasmus University Rotterdam) for expert technical assistance, Laraine Visser-Isles for English-language editing, and W. Hop (Department of Epidemiology/Biostatistics, Erasmus University Rotterdam) for statistical advice.
Author information
Authors and Affiliations
Corresponding author
Additional information
Financially supported by Serono Benelux BV and by generous gifts from the Melssen family. Equipment was made available by Siemens Elema AB, Solna, Sweden, and Sensormedics Critical Care, Bilthoven, The Netherlands.
Rights and permissions
About this article
Cite this article
van Kaam, A., de Jaegere, A., Haitsma, J. et al. Positive Pressure Ventilation with the Open Lung Concept Optimizes Gas Exchange and Reduces Ventilator-Induced Lung Injury in Newborn Piglets. Pediatr Res 53, 245–253 (2003). https://doi.org/10.1203/01.PDR.0000047520.44168.22
Received:
Accepted:
Issue Date:
DOI: https://doi.org/10.1203/01.PDR.0000047520.44168.22
This article is cited by
-
Computational assessment of airflow circuit in a double-acting solenoid-type non-invasive bi-level ventilator
Research on Biomedical Engineering (2024)
-
Standardized lung recruitment during high frequency and conventional ventilation: similar pathophysiologic and inflammatory responses in an animal model of respiratory distress syndrome
Intensive Care Medicine (2004)