Abstract
The mechanism of sudden infant death syndrome (SIDS) may be linked to an interaction between the SIDS risk factors of hyperthermia and infection, and between their effect on cytokine production and arousal. This study investigated the effects of hyperthermia and a surrogate of infection (muramyl dipeptide or MDP) on cytokine production and mortality in a neonatal rat model. Four temperature groups were studied: 34°C (baseline), 38°C, 39°C, and 40°C. Body temperatures of neonatal rat pups in the hyperthermic groups were raised and maintained at the desired temperature (38°C, 39°C, or 40°C) for 1 h and then returned to the baseline temperature (34°C) for a further hour. The heat source was a covered, heatable aluminum metal plate in a Perspex heating chamber. Intraperitoneal (IP) injection of 0.1 mL normal saline was given 30 min before the start to control for MDP (protocol A). Four equivalent treatment groups were pretreated with MDP (25 nmol/animal) instead of normal saline (protocol B). IP ketamine (55 mg/kg) was used for anesthesia during the experiments and for euthanasia. Blood was collected by direct cardiac puncture immediately after the 2-h experiments and assayed for the cytokines IL-6 and IL-1β by ELISA. Hyperthermia significantly increased the production of IL-6 (p = 0.049) but not IL-1β and significantly increased mortality. Administration of MDP significantly increased the IL-1β production (p = 0.006) but not IL-6. Cox regression analysis showed that MDP in combination with hyperthermia had a significant effect on mortality in the neonatal rat. The risk of experiencing mortality was two and half times higher in the MDP group than in the non-MDP group (p = 0.016) [hazard ratio (95% confidence interval) = 2.66 (1.20–5.92)]. We conclude that hyperthermia and a surrogate of infection (MDP) influence cytokine production and that the combination of heat stress and MDP increases mortality in the neonatal rat.
Similar content being viewed by others
Main
Despite impressive recent decreases in incidence, SIDS remains a leading cause of postneonatal mortality in Western countries. These decreases in incidence have been attributed to campaigns advising parents and healthcare providers about modifiable SIDS risk factors. These factors, identified in numerous case-controlled studies, include prone (front) sleep position, smoking by mother or father, bed sharing (especially if the mother smokes), sleeping under bedclothes, not breast-feeding, and not using a pacifier (dummy) (1–4). Other factors such as young maternal age, low socioeconomic status, high parity, low birth weight, male infant, winter months, and cold climates have long been known to be associated with SIDS (5), but are to a large extent considered to be immutable or nonmodifiable. The prone sleep position is the most important SIDS risk factor and is likely to be causal (6). However, the mechanism whereby prone sleep position causes SIDS remains unknown. Suggested mechanisms include reduction of heat loss, which increases the risk of relative or absolute hyperthermia (7), rebreathing of expired gases (8, 9), and airway obstruction (10).
Prone sleep position will reduce heat loss (11), as will covering the head with bedding. Galland and colleagues (12, 13) induced hyperthermia in neonatal piglets by covering the head with bedding and showed that this could lead to death in both sedated (with chloral hydrate) and nonsedated animals. Postmortem examination of these animals showed findings similar to those seen in heatstroke and some SIDS victims, e.g. intrathoracic petechial hemorrhages, thymic congestion, pulmonary hemorrhage, edema, and congestion (12). It has also been suggested that the possible effects of temperature in SIDS may be influenced by co-existing infection, and several species of toxigenic bacteria or their toxins have been identified in SIDS infants (14). Both hyperthermia and infection influence the production of cytokines.
Cytokines are protein or glycoprotein factors secreted by cells of both monocytoid and lymphoid lineages. These proteins function as up- and down-regulators of immunologic, inflammatory, and reparative host response to injury (15). Externally induced WBH induce production of the cytokines IL-1 and IL-6 in rats (41.5°C for 60 min) (16) and IL-1β and IL-6 in humans (41.8°C for 60 min) (17). Infection in normal-weight and low-birth weight neonates may be predicted by increased levels of IL-6, and to a lesser extent IL-1β(18, 19). Tobacco smoke, another important SIDS risk factor, may also influence cytokine production. Bronchoalveolar lavage supernatant of adult smokers has been shown to contain higher levels of IL-1β and IL-6 than does that of nonsmokers (20). Cytokines are involved in physiologic sleep regulation, e.g. IL-1 increases slow wave sleep (21), and it has been proposed that IL-1 may be the link between infection and SIDS by its adverse effect on respiratory control and arousal mechanisms (22). IL-1 may also increase the severity of apneas (23).
Muramyl peptides are derived from bacterial cell wall peptidoglycan, which constitutes as much as 90% of the cell wall of Gram-positive bacteria. In Gram-negative bacteria, only 5–20% of the cell wall is peptidoglycan, with the remainder being composed predominantly of LPS (21). MDP is a synthetic muramyl peptide. Both synthetic MDP and naturally occurring muramyl peptides exert their biologic effects, in part by inducing IL-1 (24).
An infant at a vulnerable developmental age may enter a state of positive thermal balance by virtue of the prone sleep position, soft under-bedding, heavy clothing, and/or room heating (5, 25). This could influence the production of cytokines (IL-1β, IL-6), as could other risk factors such as recent upper respiratory infection or possibly parental smoking. In turn, an increased level of IL-1 may increase slow wave sleep, blunt arousal, and increase the severity of apnea in the presence of moderate hyperthermia. This study aimed to explore the hypothesis that a mechanism of death in SIDS is linked to an interaction between hyperthermia, cytokine production, and sleep state by looking at the combined effects of hyperthermia and a surrogate for infection (MDP) on cytokine production and mortality in a small animal model (neonatal rat).
METHODS
Female Sprague Dawley rats (weights: 17.3–24.5 g) aged 10 d were used in this study. The original stock of rats was obtained from Animal Resource Centre, Perth, Australia, and mated at the Laboratory Animal Science Centre of the Chinese University of Hong Kong. The neonatal rats were kept with the mother until the start of each experiment. Three sets of experiments were conducted: protocol A to assess the effects of hyperthermia; protocol B to assess the effects of hyperthermia and MDP; and control experiments to assess possible effects of anesthesia and direct cardiac puncture on cytokine production. Animals from multiple litters were randomly assigned to the study groups.
Control of WBH.
Animals in protocols A and B were removed from the mothers and placed in a Perspex heating chamber (12.5 × 22.5 × 19.5 cm) for the 2-h duration of the experiment. The heat source in the heating chamber consisted of a covered, heatable aluminum metal plate onto which the animal was placed. The plate was connected to a temperature controller, which maintained the animal at a desired temperature by using a feedback temperature recorded from a sensor placed in the animal's rectum. The experiments were conducted in an environmental temperature of 23°C with humidity of 50–70%.
Protocol A: Animal model to examine the effects of hyperthermia.
Ten animals were studied at each of four temperatures (34°C, 38°C, 39°C, 40°C). The 34°C group (baseline temperature) was the sham heat-treatment group. This baseline temperature was determined by measuring rectal temperatures of neonatal rats aged 10–14 d (n = 12) immediately after removal from the mother using the temperature sensor connected to the temperature controller in an environmental temperature of 23°C, humidity 50–70% (the mean temperature was 33.75°C, SD 0.86). Each study animal was given 0.1 mL i.p. normal saline to control for injection of MDP (protocol B). After injection of normal saline, the pups were marked on the back and returned to the mother for 30 min. The animal was then taken from the mother again and anesthetized with ketamine hydrochloride (55 mg/kg i.p.). The pup was placed in the heating chamber and the body temperature was kept at the desired temperature (34°C, 38°C, 39°C, or 40°C) for 1 h and then returned to baseline temperature (34°C) for 1 h. The time to reach the desired temperature was 26.67 min (SD 15.15) for 38°C, 25.22 min (SD 14.03) for 39°C, and 20.29 min (SD 9.27) for 40°C. A second dose of ketamine (55 mg/kg i.p.) was given before euthanasia by direct cardiac puncture using a 27-gauge needle.
Protocol B: Animal model of MDP (infection surrogate) and hyperthermia.
This protocol was identical to protocol A with the exception that the animals were given MDP (25 nmol/animal i.p.) instead of normal saline at the start of each experiment. MDP powder (Wako Pure Chemical, Osaka, Japan) was reconstituted and stored in aliquots at −70°C until use.
Control protocol.
Three groups of experiments were conducted to assess the possible effects of anesthesia and direct cardiac puncture on cytokine production. In the first control group, five animals were studied. Each pup was given 0.1 mL i.p. normal saline and returned to the mother for 2.5 h without heating. Euthanasia and blood collection was by percutaneous cardiac puncture without anesthesia. In the second control group, 10 animals were studied. Each pup was given 0.1 mL i.p. normal saline and returned to the mother for 2.5 h without heating. Euthanasia and blood collection was by percutaneous cardiac puncture after administration of ketamine 55 mg/kg i.p.. The third control group of 10 animals was identical to the second control group, with the exception that blood was taken by direct cardiac puncture. This third control group was compared with the 34°C (baseline temperature) sham heat-treatment group (protocol A).
Data collection.
The PowerLab system (ADInstruments, Castle Hill, NSW, Australia) was used to record rectal temperature, skin temperature, power output of temperature controller, heat plate temperature, ambient temperature, concentration of ambient oxygen, and ambient carbon dioxide. All data were recorded for the duration of the experiment, with a sampling rate of two per second. Body temperature was recorded continuously from thermistor probes placed under the thigh (skin temperature) and in the rectum (inserted about 3 mm into the rectum with lubrication). Visual monitoring of movement, respiratory rate (by observing the movement of abdominal wall), and skin color was made every 15 min and recorded manually on a chart.
Blood collection and storage, and cytokine assay.
After collection by cardiac puncture at the end of each experiment, the blood sample was placed into a blank tube (Bio Plas, San Francisco, CA, U.S.A.) and centrifuged at 3000 rpm for 10 min. The serum was stored in two or three aliquots (120 μL) at −70°C until cytokine assay. IL-6 and IL-1β assay were undertaken in batches using commercially available ELISA kits (BioSource, Camarillo, CA, U.S.A.). Measurements were performed according to manufacturer's instructions and standard curves were generated for each measurement. The minimum detectable doses for IL-1β and IL-6 were noted to be <3 pg/mL and <8 pg/mL, respectively. For the IL-1β immunoassay kits, the percentage coefficients of variation for the intra-assay precision were noted to be 6.7–8.2 and for the interassay precision 8.7–9.7 (BioSource). Corresponding data for IL-6 immunoassay kits were 3.7–4.9 and 5.9–9.9.
Statistical analysis.
All values were expressed as mean (SD). Level of IL-6 was log transformed to make the data more normally distributed and homogenous of variance for further analysis. One-way ANOVA was used to evaluate the effects of anesthesia and direct cardiac puncture on cytokine production in the control group. Comparison of IL-1β and log (IL-6) measures in the non-MDP and MDP groups were analyzed by means of two-way ANOVA. Mortality in non-MDP and MDP groups was examined using the Cox proportional hazard model. All analyses were adjusted for any weight difference.
Ethical approval.
The study was approved by the Animal Research Ethics Committee of the Chinese University of Hong Kong, and a license to conduct animal experiments was obtained from the Hong Kong Department of Health.
RESULTS
There was no significant difference in the IL-1β and log (IL-6) levels between the three control groups and the sham heat-treatment group (Table 1), indicating that anesthesia (ketamine 55 mg/kg i.p.), direct cardiac puncture, and the experimental set-up did not influence the levels of these cytokines. Although all animals were studied at the age of 10 d and received the same standard diet, the body weights were significantly heavier in the non-MDP group (protocol A) as compared with the MDP group (protocol B) (mean [SD] = 21.67 [2.38]versus 20.59 [1.59] g, respectively, p = 0.019) (Table 2). No significant differences in animal weights were found between the different temperature levels (34°C, 38°C, 39°C, 40°C) in either the non-MDP or the MDP groups (p = 0.39).
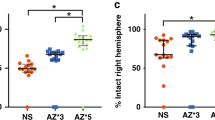
The mean values of the cytokines, IL-1β and log (IL-6), for the non-MDP and MDP groups at each of the four different temperature levels (34°C, 38°C, 39°C, 40°C) are shown in Table 2. IL-1β was significantly higher in the MDP group (43.12 pg/mL) than in the non-MDP group (34.56 pg/mL) (p = 0.006). However, IL-1β did not differ significantly between the four different temperature group (34°C, 38°C, 39°C, 40°C) (p = 0.278). A significant interaction between non-MDP/MDP and temperature (34°C, 38°C, 39°C, 40°C) was observed (p = 0.044), suggesting that the change in IL-1β level between non-MDP and MDP group differed across the four temperature groups. In contrast, the log (IL-6) value at 34°C was significantly less than the values at 38°C, 39°C, and 40°C (p = 0.049). The log (IL-6) values did not differ significantly between the non-MDP and MDP groups (p = 0.419). These results remained unchanged after adjusting for weight difference.
Baseline respiratory rates were around 150 breaths/min (93–150 breaths/min), and the respiratory rates in the heated groups (38°C, 39°C, 40°C) tended to be lower by 10–20 breaths/min. In the animals that died, the respiratory rate dropped below 90 breaths/min approximately 15 min before death (30–89 breaths/min). The color of the skin and mucosa of the animal turned pale and then dark before the breathing stopped. Both MDP and hyperthermia showed a significant association with mortality (Table 3). The risk of experiencing mortality was two and a half times higher in the MDP group than in the non-MDP group (p = 0.016) [hazard ratio (95% confidence interval) = 2.66 (1.20–5.92)]. Compared with temperature at 34°C, higher hazard ratios were found at higher temperature levels (p < 0.0001) (Table 3). Again, results were consistent after taking into account the weight effect.
Macroscopic findings at postmortem showed evidence of bleeding into the liver and kidney, but not into the lung, in the majority of the animals in the hyperthermia groups, with the proportion and degree of bleeding increasing with the level of temperature.
DISCUSSION
The study demonstrated that, in a 10-d-old neonatal rat model, hyperthermia and MDP influenced the production of the cytokines IL-1β and IL-6. An increase in body temperature in combination with a surrogate for infection (MDP) significantly increased the mortality rate in the neonatal rat. These findings are consistent with the hypothesis that hyperthermia and infection may interact with cytokine production to increase mortality.
Hyperthermia in both humans and animals has been associated with production of IL-1 and IL-6 (16, 17, 26). Although a few tissues express IL-1 constitutively, macrophages and most other cell types produce IL-1 only in response to external stimuli such as infections, bacterial LPS, and MDP (27). Two types of IL-1 (IL-1α and IL-1β) have been reported. IL-1β is the predominant form of IL-1 and the amount of IL-1β in activated cells is usually 50-fold greater than IL-1α. Both IL-1α and IL-1β have the same surface receptors and share similar biologic activities (27). Both forms of IL-1 can induce sleep, somnolence, and systemic acute phase response including fever, hepatic acute-phase protein synthesis, neutrophilia, hypozincemia, and increase level of hormones (28). Many of the biologic effects of IL-1 and TNF are similar to those observed during septic shock (29). IL-1 can also induce other cytokine synthesis, such as IL-6 and TNF (15). IL-6 can be produced by many cell types, including activated T and B lymphocytes, monocytes, endothelial cells, epithelial cells, and fibroblasts (27). It is stimulated by viral infection, bacterial products such as endotoxin and MDP, or other cytokines such as IL-1 or TNF (15, 30). IL-6 plays a central role in defense mechanisms, regulating the immune response, hematopoiesis, and acute phase reaction (31).
Our results showed that WBH (38°C, 39°C, 40°C) significantly increased the level of IL-6 compared with the sham heat-treated group (34°C), but that WBH did not significantly increase the level of IL-1β. A study of 28 heat-stroke patients showed that IL-6 was elevated in 100%, whereas IL-1β was only elevated in 39%(26). Haveman and co-workers (16) reported elevated cytokine levels in the serum of rats after both externally induced WBH (41.5°C 1 h) and local hyperthermia. Serum IL-1 and IL-6 were enhanced after WBH. The IL-1 started peaking during WBH about 15 min after reaching 41.5°C, and 2 h after WBH the IL-1 levels returned to baseline. In contrast, the IL-6 levels were not enhanced during WBH but peaked 1 h after WBH, with levels returning to baseline 4 h after WBH. For technical reasons in this neonatal rat model, it was only possible to collect a blood sample at one time point, which might therefore have missed an increase in IL-1β.
MDP, given in a dose of 25 nmol/animal i.p. in the present study, led to a significant increase in the level of IL-1β (p = 0.006) but not IL-6 (p = 0.419). MDP is both pyrogenic and somnogenic (21). It has been shown to be somnogenic in rabbits, cats, rats, and monkeys. However, in rabbits, low somnogenic doses are pyrogenic only if given during the day but not at night (21). It is possible that muramyl peptides elicit their effects on slow wave sleep via newly induced IL-1 production (21). MDP has been noted to stimulate the production of IL-1, IL-6, TNF, and IL-1 receptor antagonist in human monocytes (30). In this latter in vitro study, the IL-1, TNF, and IL-1 receptor antagonist were induced after 4 h, whereas the IL-6 was produced at a later phase (30). Studies in dogs have shown that MDP in vitro can induce IL-6 after 2 h and that liposome-encapsulated muramyl tripeptide-phosphatidylethanolamine in vivo can induce IL-6 after 3–4 h (32) Our in vivo study showed a lack of effect of MDP on IL-6 production after a 2-h period, but whether any effect might be seen after a longer period is unknown.
As stressors, hyperthermia and infection may impact the HPA system in rats. In the adult rat, response to stress is characterized by increased levels of circulating ACTH and plasma corticosterone, whereas in the first 2 wk of life this response is greatly reduced (33). The period between 2 and 15 d of life in neonatal rats has been called the SHRP (33), and during this period basal levels of circulating ACTH and corticosterone are low and do not increase appreciably after stress (33). Reasons for this hyporesponsiveness are not clear but may relate to failure of the neonatal pituitary to respond to corticotrophin-releasing factor (CRF) or to an unusually strong negative feedback mechanism to circulating levels of corticosterone (33). However, other work has suggested that the HPA axis in neonatal rats is responsive to stress throughout development in a time-dependent and stressor-specific fashion (34). Results of recent studies suggest that although the adrenal undergoes SHRP, the rest of the HPA axis is entirely competent to respond during the neonatal period (35). In view of the stresses involved in our study, it would have been desirable to assay ACTH and corticosterone levels to evaluate the HPA response to the challenges of temperature and MDP. However, it was not possible to undertake these assays in view of the limited volume of blood obtained from each animal.
The study protocol required the use of anesthesia for ethical reasons and to enable data recordings to be made. This precluded any assessment of a possible role of hyperthermia, MDP, and cytokines on sleep state and arousal in this model. Neonatal rats of 10 d of age were used in this study for theoretical and practical reasons. It was not possible to conclude at what age a neonatal rat would be most equivalent to a 2- to 3-mo-old infant, but if animals much younger than 10 d of age were used, it would not be possible to collect sufficient blood for cytokine assay. Animals much older than this age start to develop significant covering of hair and were not considered suitable. Only female rat pups were used in the study so as to remove any possible effect that gender might have had on the results. However, cyclic changes in sex hormones would not be expected to occur at this age. The neonatal rat as a model to study the effects of hyperthermia and MDP on cytokines production and mortality has limitations but also potential advantages, including convenience and ready availability of commercial kits for cytokine assay. Previous studies have used a neonatal piglet model to look at the role of hyperthermia in sudden infant death (12, 36, 37). Our study was initially designed to try to mimic these previous experiments in a small animal model. However, instrumentation and monitoring in this small animal model proved difficult. Although described in adult rats, monitoring heart rate using a pulse transducer on the tail was not successful in the neonatal rat (38).
CONCLUSIONS
In conclusion, hyperthermia significantly increased the production of IL-6 but not IL-1β, and MDP, a surrogate for infection, significantly increased the IL-1β production but not IL-6. MDP in combination with hyperthermia had a significant effect on mortality in the neonatal rat. Previous study of sedated and nonsedated neonatal piglets subjected to head-covering has shown that a proportion of piglets did not arouse before dying during the development of hyperthermia (12, 36). These circumstances of head-covering are similar to those in which some cases of SIDS occur (1). To explore an animal model of SIDS further, it may be possible, after ethical consideration, to develop this neonatal rat model further. If the body temperature of the animal could be raised to a moderate level of 38°C to 39°C without instrumentation or anesthesia, then it might be possible to assess the effect of varying temperature, MDP dose, ambient oxygen, and carbon dioxide levels on sleep, arousal, and possible mortality.
Abbreviations
- SIDS:
-
sudden infant death syndrome
- TNF:
-
tumor necrosis factor
- LPS:
-
lipopolysaccharide
- MDP:
-
muramyl dipeptide or N-acetyl-muramyl-l-alanyl-d-isoglutamine
- WBH:
-
whole-body hyperthermia
- HPA:
-
hypothalamic-pituitary-adrenal
- SHRP:
-
stress-hyporesponsive period
- CRF:
-
corticotrophin-releasing factor
References
Kemp JS, Unger B, Wilkins D, Psara RM, Ledbetter TL, Graham MA, Case M, Thach BT 2000 Unsafe sleep practices and an analysis of bedsharing among infants dying suddenly and unexpectedly: results of a four-year, population-based, death-scene investigation study of sudden infant death syndrome and related deaths. Pediatrics 106: E41
Henderson-Smart DJ, Ponsonby AL, Murphy E 1998 Reducing the risk of sudden infant death syndrome: a review of the scientific literature. J Paediatr Child Health 34: 213–219
Mitchell EA, Tuohy PG, Brunt JM, Thompson JM, Clements MS, Stewart AW, Ford RP, Taylor BJ 1997 Risk factors for sudden infant death syndrome following the prevention campaign in New Zealand: a prospective study. Pediatrics 100: 835–840
Fleming PJ, Blair PS, Bacon C, Bensley D, Smith I, Taylor E, Berry J, Golding J, Tripp J 1996 Environment of infants during sleep and risk of the sudden infant death syndrome: results of 1993–5 case-control study for confidential inquiry into stillbirths and deaths in infancy. Confidential Enquiry into Stillbirths and Deaths Regional Coordinators and Researchers. BMJ 313: 191–195
Nelson EA 1989 Sudden Infant Death Syndrome and Child Care Practices. University of Otago, Dunedin, New Zealand
Mitchell EA, Ford RP, Taylor BJ, Stewart AW, Becroft DM, Scragg R, Barry DM, Allen EM, Roberts AP, Hassall IB 1992 Further evidence supporting a causal relationship between prone sleeping position and SIDS. J Paediatr Child Health 28( suppl 1): S9–S12
Nelson EA, Taylor BJ, Weatherall IL 1989 Sleeping position and infant bedding may predispose to hyperthermia and the sudden infant death syndrome. Lancet 1: 199–201
Bolton DP, Taylor BJ, Campbell AJ, Galland BC, Cresswell C 1993 Rebreathing expired gases from bedding: a cause of cot death?. Arch Dis Child 69: 187–190
Kemp JS 1996 Rebreathing of exhaled gases: importance as a mechanism for the causal association between prone sleep and sudden infant death syndrome. Sleep 19: S263–S266
Bass M, Kravath RE, Glass L 1986 Death-scene investigation in sudden infant death. N Engl J Med 315: 100–105
Tuffnell CS, Petersen SA, Wailoo MP 1995 Prone sleeping infants have a reduced ability to lose heat. Early Hum Dev 43: 109–116
Galland BC, Taylor BJ, Bolton DPG, Elder DE, Dempster AG 1997 Experimental pathophysiological data from the piglet sleeping under bedclothes: findings compared to SIDS and to heat stroke. J SIDS Infant Mortal 2: 29–45
Galland BC, Taylor BJ, Bolton DPG, Elder DE, Dempster AG 1995 Death under bedding—pathophysiological findings compared with SIDS and heatstroke. Pediatr Pulmonol 20: 336
Blackwell CC, Weir DM, Busuttil A 1999 Infection, inflammation and sleep: more pieces to the puzzle of sudden infant death syndrome (SIDS). APMIS 107: 455–473
Bona CA, Bonilla FA (eds) 1996 Soluble mediators of cellular cooperation: the cytokines. In: Textbook of Immunology. Hardwood Academic Publishers, Amsterdam, pp 187–220
Haveman J, Geerdink AG, Rodermond HM 1996 Cytokine production after whole body and localized hyperthermia. Int J Hyperthermia 12: 791–800
Robins HI, Kutz M, Wiedemann GJ, Katschinski DM, Paul D, Grosen E, Tiggelaar CL, Spriggs D, Gillis W, d'Oleire F 1995 Cytokine induction by 41.8°C whole body hyperthermia. Cancer Lett 97: 195–201
Buscher U, Chen FC, Pitzen A, Menon R, Vogel M, Obladen M, Dudenhausen JW 2000 IL-1 beta, IL-6, IL-8 and G-CSF in the diagnosis of early-onset neonatal infections. J Perinat Med 28: 383–388
Ng PC, Cheng SH, Chui KM, Fok TF, Wong MY, Wong W, Wong RP, Cheung KL 1997 Diagnosis of late onset neonatal sepsis with cytokines, adhesion molecule, and C-reactive protein in preterm very low birthweight infants. Arch Dis Child Fetal Neonatal Ed 77: F221–F227
Kuschner WG, D'Alessandro A, Wong H, Blanc PD 1996 Dose-dependent cigarette smoking-related inflammatory responses in healthy adults. Eur Respir J 9: 1989–1994
Krueger JM, Majde JA 1994 Microbial products and cytokines in sleep and fever regulation. Crit Rev Immunol 14: 355–379
Guntheroth WG 1989 IL-1 as intermediary causing prolonged sleep apnoea and SIDS during respiratory infections. Med Hypotheses 28: 121–123
Lindgren C, Grogaard J 1996 Reflex apnoea response and inflammatory mediators in infants with respiratory tract infection. Acta Paediatr 85: 798–803
Dinarello CA, Krueger JM 1986 Induction of interleukin 1 by synthetic and naturally occurring muramyl peptides. Fed Proc 45: 2545–2548
Bolton DP, Nelson EA, Taylor BJ, Weatherall IL 1996 Thermal balance in infants. J Appl Physiol 80: 2234–2242
Bouchama A, al Sedairy S, Siddiqui S, Shail E, Rezeig M 1993 Elevated pyrogenic cytokines in heatstroke. Chest 104: 1498–1502
Oppenheim JJ, Ruscetti FW, Faltynek C 1994 Cytokines. In: Stites DP, Terr AI, Parslow TG (eds) Basic and Clinical Immunology. Appleton & Lange, Norwalk, CT, pp 105–123
Dinarello CA 1989 Interleukin-1 and its biologically related cytokines. Adv Immunol 44: 153–205
Dinarello CA 1997 Proinflammatory and anti-inflammatory cytokines as mediators in the pathogenesis of septic shock. Chest 112: 321S–329S
Suzuki K, Torii K 1994 Differences in IL-1, IL-6, TNF and IL-1 receptor antagonist production by human monocytes stimulated with muramyl dipeptide and its stearoyl derivative, romurtide. Immunopharmacology 289: 31–38
Hirano T 1992 The biology of interleukin-6. Chem Immunol 51: 153–180
Shi F, Kurzman ID, MacEwen EG 1995 In vitro and in vivo production of interleukin-6 induced by muramyl peptides and lipopolysaccharide in normal dogs. Cancer Biother 10: 317–325
Walker SJ, Vrana KE 1993 Pituitary corticotroph function during the stress hyporesponsive period in neonatal rats. Neuroendocrinology 57: 1003–1010
Walker CD, Scribner KA, Cascio CS, Dallman MF 1991 The pituitary-adrenocortical system of neonatal rats is responsive to stress throughout development in a time-dependent and stressor-specific fashion. Endocrinology 128: 1385–1395
Dallman MF 2000 Moments in time—the neonatal rat hypothalamo-pituitary-adrenal axis. Endocrinology 141: 1590–1592
Galland BC, Peebles CM, Bolton DPG, Taylor BJ 1994 The micro-environment of the sleeping newborn piglet covered by bedclothes: gas exchange and temperature. J Paediatr Child Health 30: 144–150
Jardine DS, Haschke RH 1992 An animal model of life-threatening hyperthermia during infancy. J Appl Physiol 73: 340–345
Widdop RE, Li XC 1997 A simple versatile method for measuring tail cuff systolic blood pressure in conscious rats. Clin Sci 93: 191–194
Acknowledgements
The authors thank Dr. A.E. James, Laboratory Animal Sciences Centre of the Chinese University of Hong Kong, for providing practical advice and support.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Nelson, E., Wong, Y., Yu, L. et al. Effects of Hyperthermia and Muramyl Dipeptide on IL-1β, IL-6, and Mortality in a Neonatal Rat Model. Pediatr Res 52, 886–891 (2002). https://doi.org/10.1203/00006450-200212000-00013
Received:
Accepted:
Issue Date:
DOI: https://doi.org/10.1203/00006450-200212000-00013