Abstract
We investigated whether newborn piglets exposed to hypoxemia and severe meconium aspiration could be reoxygenated with room air as efficiently as with 100% O2. Twenty-one 2- to 5-d-old piglets were randomly divided into three groups: 1) the room air group: hypoxemia, meconium aspiration, and reoxygenation with room air (n = 8); 2) the O2 group: hypoxemia, meconium aspiration, and reoxygenation with 100% O2 (n = 8); and 3) the control group: meconium aspiration, and reoxygenation with room air (n = 5). Hypoxemia was induced by ventilation with 8% O2 until the mean blood pressure reached <20 mm Hg or the base excess reached <−20 mM. At this point, reoxygenation was started with either room air or 100% O2. Three milliliters per kilogram of meconium 110 mg/mL was instilled into the trachea immediately before the start of reoxygenation. The O2 tension in arterial blood was significantly lower in the room air group; at 5 min of reoxygenation it was 9.1 ± 0.5 kPa versus 43.5 ± 6 kPa in the O2 group (p < 0.05). At 5 min of reoxygenation the tidal volume per kilogram was 12.1 ± 0.7 mL/kg in the room air group and 13.1 ± 0.9 mL/kg in the O2 group (NS). There were no significant differences between the room air and the O2 groups during 120 min of reoxygenation in mean arterial blood pressure, pulmonary arterial pressure, cardiac index, base excess, or plasma hypoxanthine. In conclusion, hypoxic newborn piglets with meconium aspiration were found to be reoxygenated as efficiently with room air as with 100% O2.
Similar content being viewed by others
Main
Meconium aspiration syndrome (MAS) continues to be one of the most common causes of neonatal respiratory distress. Recent reports (1) show that amniotic fluid is stained with meconium in approximately 12.5% of all deliveries. And MAS has been found to occur in one tenth of infants born with meconium-stained amniotic fluid, with a mortality of 4.9–37% (median 12%) (1). It thus contributes significantly to the total number of deaths in neonatal intensive care units (2), and is the primary cause of transfer to extracorporeal membrane oxygenation (1, 3). In two recent studies from developing countries (4, 5) meconium-stained amniotic fluid was present in approximately 40% of cases where infants required resuscitation at birth, indicating that meconium aspiration (MA) perhaps represents an even larger problem in these parts of the world.
Hypoxia is known to cause meconium passage into the amniotic fluid through hormonal and neural influence on the bowl peristalsis and defecation (6, 7). Hormonal and neural maturation in the intestine does not occur until about 38 wk of gestation (8, 9), so that meconium staining of the amniotic fluid is rare before this gestational age. Meconium in amniotic fluid can lead to MA and MAS, which is clinically characterized by severe respiratory distress, right to left shunting of the blood, and hypoxemia. The pathophysiology of MAS is complex and involves airway obstruction, pulmonary inflammation, surfactant dysfunction, and imbalance in pulmonary vasoregulation (1). Asphyxia is an important contributory factor in this process (10).
Until recently, the use of 100% O2 during resuscitation of asphyxiated newborn infants was commonly recommended (11). However, in the last few years, several animal studies (12–15) and two clinical studies (4, 5) have shown that resuscitation with room air is as efficient as resuscitation with 100% oxygen, and the World Health Organization's new guidelines for resuscitation now recommend the use of room air for basic resuscitation of asphyxiated newborns without MA (16). We wished to test the hypothesis that room air is as efficient as 100% O2 for reoxygenation even after MA, because the latter is the most important cause of lung problems during resuscitation of newborns.
METHODS
To test our hypothesis, we performed a randomized controlled animal study with piglets exposed to hypoxemia and severe MA. The variables we measured were MABP, PAP, cardiac index (CI), BE, and plasma hypoxanthine.
Approval.
The Norwegian Animal Experimental Board approved the experimental protocol. The animals were cared for and handled in accordance with the European Guidelines for the Use of Experimental Animals.
Surgical preparation.
Twenty-six piglets, 2–5 d old, were delivered from a local farmer on the day of the experiment. Five piglets were excluded; two because of low Hb at baseline, one because of death from air embolus in the lungs/heart at baseline, and two because of death from hypoxia at the start of reoxygenation (O2 group).
General anesthesia was induced by halothane 3% reduced to 1–1.5% mixed with 100% O2 and continued with pentobarbital sodium 20 mg/kg and pethidine 10 mg/kg i.v. as a bolus injection in an ear vein. A continuous pentobarbital infusion at a rate of 6 mg/kg/h during surgery and 3 mg/kg/h during hypoxemia and reoxygenation in the room air and 100% O2 groups was administered in a femoral vein. The rate of infusion was reduced because pentobarbital amplifies the hypoxemia-induced fall in MABP. For the control piglets, 6 mg/kg/h of pentobarbital was given throughout the experiment. At regular intervals during the experiment, we administrated a painful stimulus by pinching the snout, and if the piglets showed signs of pain, additional pethidine was given. A continuous infusion containing 0.7% NaCl and 1.25% glucose was given at a rate of 10 mL/kg/h in the right femoral vein. Blood glucose was measured regularly with a Haemo-Glucotest (Roche Molecular Biochemicals, Mannheim, Germany) and the infusion was adjusted to maintain blood glucose between 4 and 10 mM. Lidocaine 1% was used as a local anesthetic.
The piglets were tracheotomized and a 3.5-mm uncuffed Portex endotracheal tube (Portex Ltd Hythe, Kent, UK) was inserted, with a ligature around the tube and trachea to prevent leakage. They were then ventilated with a pressure-controlled ventilator, Dräger Babylog 8000+ (Drägerwerk, Lübeck, Germany). Normoventilation (Paco2 4.5–6 kPa) and a tidal volume of 10–15 mL/kg were achieved by adjusting the PIP or ventilation rate. During surgery, stabilization and hypoxia the ventilation rate was 30 breaths pr minute. An inspiratory time of 0.4 s and a positive end-expiratory pressure of 3 cm H2O were kept constant throughout the experiment.
Both femoral arteries and the right femoral and right external jugular veins were cannulated with polyethylene catheters (Portex PE-50, inner diameter 0.58 mm (Portex Ltd Hythe, Kent, UK)). Through a left-sided thoracotomy, an 8-mm ultrasonic transit time flow probe (Cardio Med, Medi-Stim, Oslo, Norway) was placed around the common pulmonary artery proximal to the ductus arteriosus for continuous recording of cardiac output (CO). For measuring the PAP, a catheter 0.8 mm outside diameter (Vygon, Ecouen, France) was inserted into the common pulmonary artery proximal to the flow probe using a Seldinger technique involving the introduction of a 20-G needle and a 0.5-mm outside diameter guidewire. The correct position was verified by the typical pressure curve of the pulmonary artery. For measuring the pressure in the left atrium, a 5F catheter with an inflatable balloon (Baxter Healthcare, Irvine, CA) was inserted into the left atrium through a small incision, the balloon was inflated with 0.25 mL of air, and a suture was placed around the incision. The chest wall was closed in two layers. The catheters were regularly flushed with heparinized saline (4 U/mL). The catheters in the left femoral artery, the right external jugular vein, the common pulmonary artery, and the left atrium were connected to strain gauge transducers. MABP, PAP, central venous pressure, and left atrium pressure were recorded continuously by a Gould recorder TA 5000 (Gould, Cleveland, OH). The heart rate (HR) was monitored by skin electrodes. The right femoral artery catheter was used for blood sampling. Rectal temperature was maintained between 38 and 40°C with a heating blanket or a radiant heating lamp. Inspired fraction of O2 and end-tidal CO2 were continuously monitored (Datex Normocap Oxy, Datex, Helsinki, Finland).
Meconium preparation.
Meconium was obtained from the first stool of more than 20 healthy term neonates of both sexes. It was pooled, diluted with distilled water, and rotavaporated dry, then diluted with sterile saline to a concentration of 110 mg/mL. To achieve a homogeneous mixture, it was blended with a blender, Bosch MSM 4001/01(Robert Bosch, Stuttgart, Germany). The meconium mixture was kept in aliquots of 10 mL at −20°C and slowly warmed up to 38°C before administration.
Experimental protocol.
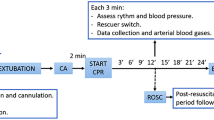
After a 30-min recovery period from surgery and before the start of hypoxia, the piglets were assigned by simple randomization to three groups. The randomization was done by the same person. Group 1 (room air group) was subjected to hypoxemia, MA, and reoxygenation with room air for 120 min (n = 8). Group 2 (O2 group) was subjected to hypoxemia, MA, and reoxygenation with 100% O2 for 30 min, followed by room air for 90 min (n = 8). Group 3 (control) was subjected to MA without hypoxemia and reoxygenated with room air for 120 min (n = 5).
Hypoxemia was achieved by ventilation with a gas mixture: 8% O2 in N2 (AGA, Oslo, Norway) until MABP fell below 20 mm Hg or BE was <−20 mM. Immediately before the start of reoxygenation, the piglets in all three groups received a bolus of 3 mL/kg of the 110 mg/kg meconium mixture via the endotracheal tube. During the first 30 s after meconium instillation they were ventilated with a Laerdal bag at a rate of 60 breaths per minute and a pressure that induced adequate chest expansion. The piglets were then put back on the ventilator with a PIP 5 cm H2O higher than baseline and the ventilation rate was increased from 30 to 60 breaths per minute. This was done to maintain a constant tidal volume of 10–15 mL/kg. During the first 30 min of reoxygenation, the Paco2 was kept between 4.5 and 6 kPa simply by altering the respiratory frequency, with a constant PIP. In the following 90 min, normoventilation was obtained primarily by reducing the respiratory frequency until a rate of 30 breaths per minute was reached. If the piglets were still hyperventilating, the PIP was reduced.
At the end of the study all the animals were killed with a dose of 100 mg/kg pentobarbital i.v. and the upper and lower lobes from the right lung were removed for histologic examination. The tissue specimens were excised, fixed in formalin, and stained with the periodic acid-Schiff (PAS) stain. The histology was then examined by a pathologist blinded to the treatment of the animals.
Blood samples.
Blood samples for blood gas analysis were drawn from the femoral artery 30 min before the start of hypoxemia, at the start of hypoxemia (baseline), every 10 min during hypoxemia, at the start of reoxygenation, and after 5, 10, 15, 30, 45, 60, 90, and 120 min of reoxygenation. Temperature-corrected acid/base status was measured with a Blood Gas Analyzer 860 (Ciba Corning Diagnostics, Midfield, MA, U.S.A.). Hb was measured at baseline and at the end of reoxygenation with a CO-Oximeter 482 (Instrumentation Laboratory, Lexington, MA, U.S.A.). Hematocrit was measured at the same time points by an ordinary centrifuge technique (results not shown).
Blood for hypoxanthine analysis was collected into prechilled EDTA-coated tubes and centrifuged without delay for 6 min at 1600 ×g at 4°C. Plasma was transferred to polypropylene tubes and frozen at −20°C until analysis. A three-fold volume of 0.9% sodium chloride replaced the withdrawn blood. Hypoxanthine concentration in plasma was analyzed by HPLC as previously described (14).
Lung function data measurements and calculation.
The Dräger Babylog 8000+ measured pressure and flow. Mean airway pressure was measured at the Y-piece. The lung volume was calculated as a function of flow. The ventilator performed the calculations of dynamic compliance (Cdyn) and resistance (R) of the respiratory system using the ventilation curve for pressure, flow, and volume and a linear regression method that measured 120 values per second (17). According to a study by Roske et al. (18), the accuracy of the volume measurements made by the Babylog 8000 was sufficient for the lung volumes used in our study. Lung function was recorded at baseline, every 10 min during hypoxemia, at the start of reoxygenation, and at 5, 10, 15, 30, 45, 60, 90, and 120 min of reoxygenation.
Hemodynamic data collection and analyses.
MABP, PAP, left atrium pressure, CO, and HR were logged into a computer using a software system developed for the logging of data (Work Bench PC for Windows, Strawberry Tree, Sunnyvale, CA, U.S.A.), using a logging frequency of 0.5 Hz. Before statistical evaluation, mean values for the logged and calculated variables for each animal were calculated in blocks of 10 s (mean of five samples) to represent each point in time.
Statistics.
All values are given as mean ± SD. All three groups were compared for differences at baseline using one-way ANOVA with Fisher's PLSD posthoc test. An unpaired t test was used to compare the room air and O2 groups to investigate whether there were any differences between the groups before the start of reoxygenation. And a paired t test was used to compare two time points in the same group. A repeated measure ANOVA was used to compare values for the room air and 100% O2 groups during the reoxygenation period. Repeated measure ANOVA with weight as covariance and simple regression analyses were performed to correlate for the difference in the weight between the groups. Two-sided p values <0.05 were considered significant. These analyses were done with the statistical computer programs: StatView 5.0, (Abacus Concepts, Berkeley, CA, U.S.A.) and Social Science, Windows Release 8.0 (SPSS, Chicago, IL, U.S.A.). A graphics program (Graphpad Prism, version 2.01, Graphpad Software, San Diego, CA, U.S.A.) was used to produce the graphs.
RESULTS
The mean body weight in the room air group, 2.5 ± 0.15 kg, was significantly higher (p = 0.03) than in either the O2 group, 2.0 ± 0.14 kg, or the control group, 2.0 ± 0.14 kg (p = 0.04). The mean age was 3.8 ± 0.3 d in the room air group, 3.5 ± 0.4 d in the O2 group, and 3.4 ± 0.7 d in the control group (NS). The mean duration of hypoxemia in the room air group was 34 ± 6 min versus 46 ± 14 min in the O2 group (NS). Nor were there any significant differences between the room air and O2 groups in Pao2, BE, plasma hypoxanthine, MABP, PAP, CI, and pulmonary vascular index at baseline or at the start of reoxygenation (Figs. 1 and 2).
Pao2, BE, and plasma hypoxanthine (Hyp) at baseline (BL) and during hypoxia (H) and reoxygenation (R). Values are expressed as mean ± SD. *p < 0.05 room air vs 100% O2 group. **p < 0.05 start of reoxygenation vs 5 min of reoxygenation in the control group. #p < 0.05 baseline vs start of reoxygenation in room air and O2 groups.
(A) MABP, (B) PAP, (C) pulmonary vascular resistance index (PVRI), and (D) cardiac index (CI), at baseline (BL), during hypoxia (H), and reoxygenation (R). Values are expressed as mean ± SD. *p < 0.05 start of reoxygenation vs 5 min of reoxygenation in the control group. #p < 0.05 start of reoxygenation vs 10 min of reoxygenation in the control group. **p < 0.05 baseline vs start of reoxygenation in the room air and O2 groups. §p < 0.05 start of reoxygenation vs 5 min of reoxygenation in the room air and O2 groups.
Blood samples.
Pao2 levels (Fig. 1) decreased from baseline to 4.3 ± 0.1 and 4.8 ± 0.3 kPa at the end of hypoxemia in the room air and O2 groups, respectively. During reoxygenation, Pao2 increased to 9.0 ± 0.5 kPa in the room air group versus 43.5 ± 6 kPa (p < 0.05) in the O2 group at 5 min of reoxygenation. This difference persisted during the 30 min of reoxygenation with 100% O2. Excluding the period of hyperoxia, there were no statistically significant differences between the room air and O2 groups. In the control group Pao2 decreased from 12.8 ± 0.7 to 6.9 ± 0.8 kPa from MA to 5 min of reoxygenation (p < 0.05). This indicates that there was acute lung injury from the MA.
BE (Fig. 1) decreased to a nadir of −19.7 ± 1.9 and −22.2 ± 0.7 mM at 5 min of reoxygenation and increased to −1.9 ± 0.8 and −5.5 ± 1.3 mM after 120 min of reoxygenation in the room air and O2 groups, respectively. There were no significant differences between the two groups either during hypoxemia or reoxygenation.
Plasma hypoxanthine (Fig. 1) increased significantly from baseline level to a maximum of 116 ± 6 and 103 ± 13 μmol/L at the start of reoxygenation and returned to baseline at the end of reoxygenation in the room air and O2 groups, respectively. We did not find any statistically significant differences between the groups during the experiment.
Hemodynamics.
During hypoxemia, MABP (Fig. 2 A) decreased to 38 ± 8 and 29 ± 3 mm Hg in the room air and O2 groups, respectively, (NS) at the start of reoxygenation. MABP returned to baseline levels after 5 min of reoxygenation. There were no significant differences in MABP between the room air and the O2 groups during the reoxygenation period. In the control group, the MABP decreased significantly after instillation of meconium and returned to baseline after 15 min of reoxygenation.
PAP (Fig. 2B) increased during the first part of hypoxia and fell subsequently in both the room air and O2 groups. During reoxygenation, PAP once more increased in the two groups but there were no statistically significant differences between the groups at any time. In the control group, PAP increased significantly after instillation of meconium.
The pulmonary vascular index (Fig. 2C) increased significantly during hypoxemia, but not during reoxygenation, without any differences between the room air and O2 groups.
The CI (Fig. 2D) decreased significantly in both the room air and O2 groups during hypoxemia, increased significantly to a maximum at 5 min of reoxygenation and then decreased to baseline levels. No significant differences were found between the room air and O2 groups at any time.
Lung functions.
There were no significant differences in tidal volume per kilogram, PIP, or ventilation rate between the room air, O2, and control groups at any time (Table 1).
Cdyn per kilogram (Table 1) was significantly different at baseline between the room air and O2 groups, with no differences at the start of reoxygenation or during reoxygenation. From baseline to 5 min of reoxygenation, Cdyn per kilogram decreased significantly in all groups. After 5 min of reoxygenation Cdyn per kilogram increased in all groups, but without completely reaching baseline level.
R (Table 1) increased significantly from baseline to the end of reoxygenation in the room air and O2 groups. In the control group, airway resistance increased significantly from the start of reoxygenation to end of reoxygenation. There were no significant differences between the room air and O2 groups from baseline to the end of reoxygenation.
Lung histology.
In all the animals, widespread meconium was seen in peripheral airspace, with no differences between the groups.
DISCUSSION
These results demonstrate that newborn piglets exposed to hypoxemia followed by MA can be reoxygenated as efficiently with room air as with 100% O2, assessed in terms of mean arterial blood pressure, PAP, CI, base deficit, and plasma hypoxanthine.
Unfortunately, there was a statistically significant difference in weight between the room air and O2 groups. To test the influence on the results, we performed statistical tests with weight as a covariant and regression analyses, and found that the weight difference had no influence. The CO, tidal volume, and Cdyn are also corrected for the weight. All medication and the amount of meconium instilled were given according to weight. Theoretically, one would expect that higher body weight in one group would increase the hypoxia time in this group, but this was not the case. The difference in weight was not large enough to make the surgical procedures more difficult in the groups with the smallest piglets. The degree of maturity of the piglets is probably more important than the body weight, but there were no differences in age between the groups.
Several investigators have studied MA in pigs, but hypoxemia was not induced before instillation of meconium in any of these studies (19–22). Meconium inhaled below the vocal cords in an unasphyxiated infant produces only mild benign self-limiting respiratory challenge that is asymptomatic in >90% of cases (23–25). The animals in this experiment were hypoxemic but not hypercarbic. Hypoxia leads to vasoconstriction in the pulmonary circulation. Repeated or longstanding prelabor asphyxia is known to induce pulmonary arterial muscle hypertrophy and increased vascular hyperreactivity of the pulmonary vessels. Hypoxemia-induced pulmonary hypertension is an important change in pulmonary circulation in MAS. MA can occur either in utero, after hypoxia-induced gasping, or with the infant's first breath. In the present study, the hypoxemia before meconium instillation mimicked the clinical situation of aspiration of meconium in an infant exposed to a single period of hypoxemia followed by aspiration of meconium at the first breath.
However, in contrast to newborn infants, the piglets were 2–5 d old and, therefore, to some extent adapted to extrauterine life. In a clinical situation, this adaptation has barely started at the time of MA. Haworth et al. (26) studied the adaptation of the pulmonary circulation to extrauterine life in piglets and concluded that functionally the pulmonary circulation did not appear to be mature until the age of 2 wk and that an adult pattern was established by the age of 6 mo. These findings seem to justify our use of piglets that were a few days old, and to indicate that our results are applicable to the study of changes in the pulmonary pressure after hypoxemia and MA in newborns. However, in an unadapted lung, the migration time of meconium from the large to the smaller airways with aspiration is probably shorter because the amniotic fluid in the airways dilutes the meconium.
The use of anesthetics in experimental animal research will obviously affect the results and complicate interpretation and comparison with a clinical situation. We chose an anesthetic that would minimize distress for the piglets and at the same time have the least possible influence on the results. Strøm et al. (27) found that pentobarbital had no significant influence on hemodynamic performance over a wide range of plasma pentobarbital concentrations. Sensitivity to barbiturates and the influence on hemodynamics are altered by conditions such as hypoxemia (28). To compensate for this, we reduced the infusion of pentobarbital during hypoxemia. Pentobarbital has little analgesic effect, and must be supplemented by an opioid. To have as little effect as possible on hemodynamics, pethidine was only given if the piglets reacted to an additional painful stimulus.
MAS has a complex pathophysiology and has early and late effects (2). The early effects may be caused by the particulate nature of meconium and are primarily the result of obstruction leading to increased expiratory resistance, inactivation of surfactant, decreased dynamic lung compliance, hypoxemia, hypercapnia, and acidosis. The late effects are caused by the components of meconium and include inflammatory changes with airway and alveolar collapse secondary to chemical pneumonitis. In our study, we followed the piglets for 2 h, so that the results only provide information on the early phase after MA.
Ninety five percent of cases of MAS develop in the presence of thick meconium. In the presence of thin meconium, the associated respiratory disease is mild (10). We therefore used thick meconium, at a concentration of 110 mg/mL, which had been homogenized with a blender. Others (20–22) have used filtered meconium. Airway obstruction is one of the early mechanical effects of MA (1), and we thought this effect might be reduced if the meconium were filtered. The findings in the control group clearly demonstrated that the meconium we used induced changes in the airways and the lungs compatible with those seen in human infants with MA.
At reoxygenation, Pao2 quickly normalized in the room air group, but reached supranormal values in the 100% O2 group. Potentially toxic amounts of free oxygen radicals like superoxide radicals and highly reactive hydroxyl radicals may be produced during reoxygenation of hypoxic ischemic tissue. The production of radicals after severe hypoxia-ischemia may be proportional to tissue Po2(29). High Po2 achieved during reactive hyperemia and high fractions of O2 during early resuscitation may therefore contribute to a burst of free oxygen radicals, resulting in damage to the epithelia and impairment of both production and functions of the surfactant system (30).
A key question is whether room air will reoxygenate the tissues as thoroughly as 100% O2. During hypoxia, MABP falls, partly as a result of reduced myocardial contractility, resulting in a fall in cardiac output. In our study, MABP and CI increased as much in the room air as in the O2 group, indicating that the myocardium was oxygenated sufficiently during reoxygenation. Further, the fact that there were no significant differences between the groups in plasma hypoxanthine and BE during reoxygenation indicates that most tissues are reoxygenated as thoroughly with room air as with pure oxygen.
Although the complete mechanism of pulmonary vasorelaxation is not known, increasing Pao2, expansion and inflation of the lungs at birth are important factors (10). In our study, the piglets were exposed to only one period of severe hypoxemia during which PAP increased as expected, confirming that the pulmonary vessels were able to react. The control group showed a significant increase in PAP after instillation of meconium, indicating, as reported by others (20), that meconium alone induces pulmonary hypertension through an inflammatory process. There were no differences in PAP between the room air and 100% O2 groups during reoxygenation, showing that resuscitation with room air provided sufficient Pao2 to dilate the pulmonary vascular system as efficiently as 100% O2. If O2 is to be diffused from the lungs into the blood, the pressure of the inspired gas needs to be adequate and a sufficient volume of gas needs to be administered for the lungs to expand. Successful room air resuscitation depends upon adequate ventilation. In our study, both groups were equally ventilated, and there was no statistical differences between the groups in ventilation rate, PIP or Vt/kg.
We did not evaluate possible differences in hypoxic-ischemic brain damage. Although vital organs like the heart are as efficiently reoxygenated with room air as with 100% O2, possible differences in hypoxic-ischemic brain damage should be ruled out before a clinical trial. There may be circumstances where resuscitation with 100% O2 is superior to room air because the available alveolar surface is so reduced that room air is not sufficient to satisfactorily oxygenate the blood perfusing the lungs.
In conclusion, these results indicate that room air under certain circumstances may be good enough to resuscitate neonatal infants after meconium aspiration. More studies are needed in animal models before clinical trials can be considered.
Abbreviations
- BE:
-
base excess
- MABP:
-
mean arterial blood pressure
- PAP:
-
mean pulmonary artery blood pressure
- PIP:
-
peak inspiratory pressure
- Paco2:
-
arterial CO2 tension
- Pao2:
-
arterial O2 tension
References
Cleary GM, Wiswell TE 1998 Meconium-stained amniotic fluid and the meconium aspiration syndrome. An update. Pediatr Clin North Am 45: 511–529
Coltart TM, Byrne DL, Bates SA 1989 Meconium aspiration syndrome: a 6-year retrospective study. Br J Obstet Gynaecol 96: 411–414
Moront MG, Katz NM, Keszler M, Visner MS, Hoy GR, O'Connell JJ, Cox C, Wallace RB 1989 Extracorporeal membrane oxygenation for neonatal respiratory failure. A report of 50 cases. J Thorac Cardiovasc Surg 97: 706–714
Ramji S, Ahuja S, Thirupuram S, Rootwelt T, Rooth G, Saugstad OD 1993 Resuscitation of asphyxic newborn infants with room air or 100% oxygen. Pediatr Res 34: 809–812
Saugstad OD, Rootwelt T, Aalen O 1998 Resuscitation of asphyxiated newborn infants with room air or oxygen: an international controlled trial: the Resair 2 study. Pediatrics 102: e1
Dawes GS, Fox HE, Leduc BM, Liggins GC, Richards RT 1972 Respiratory movements and rapid eye movement sleep in the foetal lamb. J Physiol (Lond) 220: 119–143
Duenhoelter JH, Pritchard JA 1977 Fetal respiration. A review. Am J Obstet Gynecol 129: 326–338
Grand RJ, Watkins JB, Torti FM 1976 Development of the human gastrointestinal tract. A review. Gastroenterology 70: 790–810
Lucas A, Adrian TE, Christofides N, Bloom SR, Aynsley-Green A 1980 Plasma motilin, gastrin, and enteroglucagon and feeding in the human newborn. Arch Dis Child 55: 673–677
Katz VL, Bowes WA Jr 1992 Meconium aspiration syndrome: reflections on a murky subject. Am J Obstet Gynecol 166: 171–183
American Heart Association 1992 Emergency Cardiac Care Committee and Subcommittees Guidelines for cardiopulmonary resuscitation and emergency cardiac care. VII. Neonatal resuscitation. JAMA 268: 2276–2281
Rootwelt T, Loberg EM, Moen A, Oyasaeter S, Saugstad OD 1992 Hypoxemia and reoxygenation with 21% or 100% oxygen in newborn pigs: changes in blood pressure, base deficit, and hypoxanthine and brain morphology. Pediatr Res 32: 107–113
Rootwelt T, Odden JP, Hall C, Ganes T, Saugstad OD 1993 Cerebral blood flow and evoked potentials during reoxygenation with 21 or 100% O2 in newborn pigs. J Appl Physiol 75: 2054–2060
Feet BA, Yu XQ, Rootwelt T, Oyasaeter S, Saugstad OD 1997 Effects of hypoxemia and reoxygenation with 21% or 100% oxygen in newborn piglets: extracellular hypoxanthine in cerebral cortex and femoral muscle. Crit Care Med 25: 1384–1391
Medbo S, Yu XQ, Asberg A, Saugstad OD 1998 Pulmonary hemodynamics and plasma endothelin-1 during hypoxemia and reoxygenation with room air or 100% oxygen in a piglet model. Pediatr Res 44: 843–849
World Health Organization Maternal and Newborn Health/Safe Motherhood Unit. Division of Reproductive Health (Technical Support). 1998 Basic Newborn Resuscitation: A Practical Guide. World Health Organization, Geneva
Drager Medizintechnik GmbH 1998 Babylog 8000 Plus Intensive Care Ventilators for Neonates: Instruction for Use. Version 5.n. Drager Medizintechnik GmbH, Lübeck, Germany, pp 125–126
Roske K, Foitzik B, Wauer RR, Schmalisch G 1998 Accuracy of volume measurements in mechanically ventilated newborns: a comparative study of commercial devices. J Clin Monit Comput 14: 413–420
Davey AM, Becker JD, Davis JM 1993 Meconium aspiration syndrome: physiological and inflammatory changes in a newborn piglet model. Pediatr Pulmonol 16: 101–108
Soukka H, Halkola L, Aho H, Rautanen M, Kero P, Kaapa P 1997 Methylprednisolone attenuates the pulmonary hypertensive response in porcine meconium aspiration. Pediatr Res 42: 145–150
Sun B, Curstedt T, Robertson B 1993 Surfactant inhibition in experimental meconium aspiration. Acta Paediatr 82: 182–189
Sun B, Curstedt T, Robertson B 1996 Exogenous surfactant improves ventilation efficiency and alveolar expansion in rats with meconium aspiration. Am J Respir Crit Care Med 154: 764–770
Rossi EM, Philipson EH, Williams TG, Kalhan SC 1989 Meconium aspiration syndrome: intrapartum and neonatal attributes. Am J Obstet Gynecol 161: 1106–1110
Falciglia HS 1988 Failure to prevent meconium aspiration syndrome. Obstet Gynecol 71: 349–353
Dooley SL, Pesavento DJ, Depp R, Socol ML, Tamura RK, Wiringa KS 1985 Meconium below the vocal cords at delivery: correlation with intrapartum events. Am J Obstet Gynecol 153: 767–770
Haworth SG, Hislop AA 1981 Adaptation of the pulmonary circulation to extra-uterine life in the pig and its relevance to the human infant. Cardiovasc Res 15: 108–119
Strom J, Haggmark S, Reiz S, Sorensen MB 1987 Cardiovascular effects of pentobarbital in pigs, and the lack of response to naloxone in pentobarbital induced circulatory failure. Acta Anaesthesiol Scand 31: 413–416
Gilman GA 1996 The Pharmacological Basis of Therapeutics, 9th Ed, McGraw-Hill, New York, pp 321–323
Fisher PW, Huang YC, Kennedy TP, Piantadosi CA 1993 PO2-dependent hydroxyl radical production during ischemia-reperfusion lung injury. Am J Physiol 265: L279–L285
Pitkanen OM HM 1998 Evidence for increased oxidative stress in preterm infants eventually developing lung disease. Semin Natol 3: 199–205
Acknowledgements
We thank Thore Egeland for valuable advice on statistics.
Author information
Authors and Affiliations
Corresponding author
Additional information
Supported, in part, by the Norwegian Foundation for Health and Rehabilitation, the Norwegian Council for Cardiovascular Disease, the Norwegian Women's Public Health Association, and the Research Council of Norway.
Rights and permissions
About this article
Cite this article
Tølløfsrud, P., Solås, A. & Saugstad, O. Newborn Piglets with Meconium Aspiration Resuscitated with Room Air or 100% Oxygen. Pediatr Res 50, 423–429 (2001). https://doi.org/10.1203/00006450-200109000-00020
Received:
Accepted:
Issue Date:
DOI: https://doi.org/10.1203/00006450-200109000-00020
This article is cited by
-
Initiating delivery room stabilization/resuscitation in very low birth weight (VLBW) infants with an FiO2 less than 100% is feasible
Journal of Perinatology (2009)
-
Toxic effects of different meconium fractions on lung function: new therapeutic strategies for meconium aspiration syndrome?
Journal of Perinatology (2008)
-
Effect of Resuscitation with 21% Oxygen and 100% Oxygen on NMDA Receptor Binding Characteristics Following Asphyxia in Newborn Piglets
Neurochemical Research (2007)