Abstract
Methylxanthines such as caffeine and theophylline are known to inhibit glucose transport. We have studied such inhibition in the glucose transporter type 1 deficiency syndrome (Glut1DS) by erythrocyte glucose transport assays. Data from four patients with individual mutations in the GLUT1 gene are discussed: patient 1 (hemizygosity), 3 (S66F), 15 (368Ins23), and 17 (R333W). Zero-trans influx of 14C-labeled 3-O-methyl glucose (3-OMG) into erythrocytes of patients is reduced (patient 1, 51%; 3, 45%; 15, 31%; 17, 52%) compared with maternal controls. Inhibition studies on patients 1, 3, 17, and maternal controls show an IC50 for caffeine of approximately 1.5 mM both in controls (n = 3) and patients (n = 3) at 5 mM 3-OMG concentration. In the same two groups, kinetic studies show that 3 mM caffeine significantly decreases Vmax (p < 0.005), whereas the decrease in Km is significant (p < 0.01) only in the three controls and one patient (patient 3). Kinetic data from individual patients permit us to speculate that the interactions between caffeine and Glut1 are influenced by the mutation. Three mM caffeine also inhibits the transport of dehydroascorbic acid (DHA), another substrate for Glut1. The combined effects of caffeine (3 mM) and phenobarbital (10 mM) on glucose transport, as determined in patient 15 and the maternal control, show no additive or synergistic inhibition. These data indicate that caffeine and phenobarbital have similar Glut1 inhibitory properties in these two subjects. Our study suggests that Glut1DS patients may have a reduced safety margin for methylxanthines. Consumption of methylxanthine-containing products may aggravate the neurologic symptoms associated with the Glut1DS.
Similar content being viewed by others
Main
Transport of d-glucose across the blood-brain barrier is mediated by a sodium-independent facilitative transport protein, Glut1 (1–4). Mutations in the GLUT1 gene leading to defective function of the transporter have been identified as the pathogenetic mechanism of the Glut1DS. Erythrocyte and fibroblast 3-OMG uptake studies reveal a reduced Glut1 activity (5–8). The defect has recently been defined at the molecular level (5, 9, 10). The failure to meet brain glucose demand leads to hypoglycorrhachia, infantile seizures, acquired microcephaly, and developmental delay (6–8), a state of GLUT1 haploinsufficiency.
Additional inhibition of Glut1 activity can be expected to intensify impaired cerebral glucose homeostasis in these patients. In this context, methylxanthines such as caffeine and theophylline have been reported to inhibit glucose transport in erythrocytes and adipocytes (11, 12). Methylxanthine neurotoxicity includes potentially life-threatening convulsions (13). The proconvulsant actions of methylxanthines have been associated with their antagonistic properties to the adenosine receptors (14, 15). Whether the inhibition of glucose transport by methylxanthines could potentiate the proconvulsant effects of these compounds is unclear.
Methylxanthines are well-known phosphodiesterase inhibitors. The inhibition of sugar transport by these compounds has been attributed to changes in intracellular cAMP levels in systems in which adenyl cyclase and phosphodiesterases are active (16). In these studies (using the adipocyte system, for example), the effects of methylxanthines on sugar transport are further complicated by the abilities of these compounds to modulate gene expression and other metabolic pathways (17). These potential confounding factors are minimized in erythrocytes due to the absence of nuclei and low adenyl cyclase and phosphodiesterase activities in these cells. Thus, erythrocytes provide a simple system for studying the effects of methylxanthines directly on glucose transporters, circumventing the confounding factors mentioned above.
In the present study, we investigated the effect of caffeine and theophylline on Glut1-mediated transport of glucose in erythrocytes of four Glut1DS patients and maternal controls. Our results confirm the hypothetical risks that these compounds pose for the Glut1DS patients.
METHODS
Clinical material.
Blood samples were obtained from four patients diagnosed with the Glut1DS. Samples from mothers (n = 4) were used as intraassay controls. The present study was reviewed and approved by the Columbia University Institutional Review Board. All patients and parents gave informed consent for the studies.
Patient 1 (male, 11 y).
The clinical history of this patient has been described previously (5, 6).
Patient 3 (male, 15 y).
The clinical history of this patient has been described previously (18).
Patient 15 (female, 8 y).
Patient was born after a 39-wk pregnancy complicated by vomiting. Labor was induced and followed by cesarean section. No problem was noted during the newborn period. Seizures started at 3 mo of age. Patient showed decreased head growth and delayed neurologic development during the first year of life. Phenobarbital treatment from age 18 mo to 3 y was ineffective. Hypoglycorrhachia was noted at 45 mo of age. Glut1DS was confirmed at age 4 y; the ketogenic diet was initiated, and seizures were controlled. The child continues to have mild microcephaly and delays in language and cognitive skills.
Patient 17 (male, 9 y).
Patient was born after an uncomplicated full-term pregnancy. Cesarean section was necessary because of fetal positioning. Birth and newborn periods were normal. Seizures started at age 17 d. Hypoglycorrhachia was noted by 27 d of age, and a ketogenic diet was initiated. The Glut1DS was diagnosed at 2 mo of age. The child has enjoyed normal development and has had no further seizures.
Controls (four females).
Four mothers of Glut1DS patients were used as intraassay controls. All were healthy individuals with no clinical or molecular evidence for the Glut1DS.
Mutations in the GLUT1 gene.
All four patients reported in this study have heterozygous mutations (one normal allele and one mutant allele) in the GLUT1 gene (1p35–31.3). Patient 1 has GLUT1 hemizygosity (5). Patients 3 and 17 have heterozygous missense mutations on different locations of the gene, whereas patient 15 has a heterozygous insertion mutation. In patient 3, the mutation is located in the extracellular loop between helices 1 and 2, causing a substitution of phenylalanine for serine (S66F) (18). In patient 17, the mutation is located in the intracellular loop between helices 8 and 9, substituting a tryptophan for an arginine (R333W). In patient 15, a 23-nucleotide insertion is present at nucleotide number 368 of the GLUT1 cDNA (368Ins23), resulting in a frameshift mutation (9, 10). Molecular screening of the maternal controls was negative in all cases.
Reagents.
3-OMG, caffeine, theophylline, phenobarbital, phloretin, and mercuric chloride were purchased from Sigma Chemical Co. (St. Louis, MO, U.S.A.).
Solutions.
To approximate physiologic conditions, 3-OMG concentrations at incubation were 5 mM unless otherwise indicated. Caffeine or theophylline was added using 100 mM stock solution freshly prepared with PBS, pH 7.4. 14C-labeled 3-OMG (stock, 56.4 mCi/mmol) was purchased from DuPont NEN (Boston, MA, U.S.A.). Final radioactivity in the uptake samples was 1.5 μCi/mL. The stop solution contained 100 μM mercuric chloride and 50 μM phloretin in ice-cold PBS, prepared immediately before use.
Blood samples.
Blood samples were preserved in citrate-phosphate-dextrose anticoagulant solution (5:1, vol/vol) and immediately stored at 4°C. Samples were processed within 10 d. Sample volumes were limited, precluding performance of every test in each patient. Samples were excluded if hemolysis occurred. None of the subjects had been transfused in the past 3 mo.
Preparation of erythrocytes.
Procedures were performed at 4°C. Blood specimens (2–5 mL) were centrifuged at 1000 ×g for 10 min. The supernatant was discarded, and the erythrocytes were washed three times with PBS. Erythrocytes were then resuspended in PBS at approximately the original blood-sample volume. Fifty-microliter aliquots were taken for immediate assay, and 100 μL was used for a cell count.
3-OMG uptake.
The Lowe and Walmsley techniques were modified as previously described (19). In a 4°C cold room, 100 μL 14C-labeled 3-OMG solution at the specified concentrations was added to the 50-μL aliquot of the erythrocyte suspension; the assay was terminated at appropriate time points by rapid addition of 1 mL of ice-cold stop solution. The washing steps were carried out at room temperature. After centrifugation at 2000 ×g for 5 min, the erythrocyte pellet was washed twice with ice-cold 1 mL stop solution. After the final centrifugation, pellets were digested in 0.5 mL of quarternary ammonium hydroxide solubilizing agent (Soluene, Packard, Meriden, CT, U.S.A.). At room temperature, samples were bleached with 0.25 mL 30% hydrogen peroxide. The mixture was swirled until all foaming subsided (20). Five mL/sample of Hionic Fluor scintillation fluid (Packard, Meriden, CT, U.S.A.) was added, and aliquots were counted with a Packard TR 2300 scintillation counter.
DHA uptake.
1–14C-labeled ascorbic acid was oxidized to 1–14C-labeled DHA by the addition of ascorbate oxidase (125 U/mL H2O) and measured by HPLC as described (21). After a 15-s incubation of 50 μL of erythrocyte suspension with 50 μL of 1–14C-labeled DHA (10 and 25 μM, 8 μCi/mL) at 4°C (in the presence or absence of 3 mM caffeine), the uptake was terminated by the addition of ice-cold stop solution. Washing procedures were performed as described in the 3-OMG uptake section. Influx of 1–14C-labeled DHA was determined as previously described (21).
Use of methylxanthines.
14C-labeled 3-OMG stock solution was premixed with caffeine or theophylline stock solution to obtain the final concentrations of interest (0 to 10 mM for methylxanthines, 0.6 to 10 mM for 3-OMG). Influx was started by adding 100 μL of the 14C-labeled 3-OMG solution with the specified 3-OMG and methylxanthine concentrations to the erythrocyte suspension. Influx was terminated after 15 s (unless otherwise indicated) by the rapid addition of 1 mL ice-cold stop solution. The washing steps were performed as described in the 3-OMG uptake section.
Use of phenobarbital.
Phenobarbital was dissolved in a vehicle solution containing 10% (vol/vol) EtOH, 75% 1.2-propanediol, and 15% distilled water. In previous studies, we have shown that this vehicle does not interfere with erythrocyte 3-OMG uptake (18). Based on previous results, a concentration of 10 mM (50% inhibition of 3-OMG uptake) was used for assays (18).
GLUT1 genomic analyses.
DNA analyses were performed in all patients and maternal controls as described previously (5, 8, 9). A detailed analysis of techniques and results has been discussed elsewhere (9).
Statistical analyses.
Data are expressed as the mean ± SD unless otherwise indicated. The t test was performed to identify significant differences between the experimental groups. A significant difference was determined at p < 0.05. Data analyses and best fits were generated using Microsoft Excel and Origin software (Microcal Software Inc., Northampton, MA, U.S.A.).
RESULTS
Erythrocyte 3-OMG influx.
Zero-trans 3-OMG uptake is determined in four patients to confirm the clinical diagnosis of Glut1DS. Samples from the mothers serve as normal controls. 3-OMG uptake is expressed as the natural logarithm of the ratio of intracellular radioactivity at each time point and at equilibrium versus time (Fig. 1). All four patients show decreased (patient 1, 51%; 3, 45%; 15, 31%; 17, 52%) 3-OMG uptake compared with the controls.
Erythrocyte 3-OMG uptake studies. The data (two determinations per data point) are expressed as the natural logarithm of the ratio of intracellular radioactivity (Ct) at each time point and at equilibrium (Ceq) vs time in seconds. Slope of the linear-fit curve derived from patient uptake values was divided by the slope of the curve derived from maternal control uptake values and multiplied by 100 to obtain the relative uptake level in percentage (patient 1, 51%; 3, 45%; 15, 31%; 17, 52%). Closed circles represent patient data points;open diamonds represent maternal control data points.
Time course of 3-OMG influx in the presence and absence of caffeine.
To decide on a suitable uptake interval, we followed the time course of 3-OMG uptake over a period of 25 s. The 3-OMG concentration (5 mM) approximates the blood d-glucose concentration. Inhibition of glucose uptake is observed within 5 s of incubation with 3 mM caffeine, as shown in Figure 2A (patient 1 and maternal control 1). The inset shows the pooled data of similar observations in three patients (1, 3, and 17) and three maternal controls (1, 3, and 17). For technical reasons, we settled on a 15-s time interval for all uptake assays. Caffeine clearly impairs 3-OMG uptake values in both controls and patients. DHA, also transported by Glut1 (21, 22), demonstrates similar inhibition by caffeine. Shown in Figure 2B, 15-s coincubation with 3 mM caffeine significantly decreases erythrocyte DHA uptake in both the patient 1 and the maternal control 1.
Caffeine inhibits zero-trans influx of 3-OMG and DHA. (A) Initial time course (0–25 s) of zero-trans influx of 3-OMG (5 mM) at 4°C into erythrocytes in the presence or absence of 3 mM caffeine. The results represent the mean of triplicate experiments ± SE performed on samples from patient 1 and his mother. Inset, pooled data of three patients and three maternal controls (x axis time in seconds, y axis 3-OMG uptake in fmol/106 cells). Open diamonds represent mother without caffeine;closed circles represent patient without caffeine. Open triangles represent mother with caffeine;open circles represent patient with caffeine. (B) Zero-trans DHA (10 and 25 μM) influx at 4°C into erythrocytes in the presence or absence of 3 mM caffeine (three determinations per data point) after a 15-s incubation. Closed bars represent data from patient;open bars represent data from maternal control. *For the same subject at a given DHA concentration (10 or 25 μM), the difference in DHA uptake between no caffeine control group and 3 mM caffeine treatment group is statistically significant (p < 0.05).
Influence of caffeine concentration on zero-trans 3-OMG influx.
Erythrocytes of maternal controls (1, 3, 17) and patients (1, 3, 17) are incubated with caffeine (0–10 mM) and 3-OMG (5 mM) for 15 s, followed by the measurement of 3-OMG influx. Figure 3A shows that, both in controls and patients, caffeine apparently inhibits glucose uptake at concentrations of 1 mM and above. This is similar to the minimal concentration (1 mM) required for inhibition with phenobarbital (18). At higher concentrations of caffeine, 3-OMG influx is increasingly inhibited. In the patients, even low concentrations of caffeine inhibit 3-OMG influx (note that 100% influx in the patients equals 42 to 54% influx of the controls, which results in a shallower slope for patient influx). Influx of 3-OMG into the patients' erythrocytes is inhibited further to 10 to 18% of the baseline (no caffeine treatment) maternal control value after incubation with 10 mM caffeine. The data of individual patients and controls in Figure 3A are pooled and converted into relative degrees of inhibition of 3-OMG uptake in response to increasing dosage of caffeine (Fig. 3B). 3-OMG influx was inhibited by caffeine in a hyperbolic dose-dependent fashion. Extrapolation [using the equation y = a + b × K/(x + K), where y represents 3-OMG uptake, x represents caffeine concentration, a represents residual 3-OMG uptake not inhibited by caffeine, b represents caffeine inhibitable 3-OMG uptake, and K represents IC50] yielded an IC50 of 1.6 ± 1.1 mM in controls and 1.4 ± 1.1 mM in patients. This difference is not statistically significant. Similarly, theophylline also exhibits dose-dependent inhibition on erythrocyte 3-OMG uptake (Fig. 3C).
Dose-dependent inhibition of caffeine and theophylline on erythrocyte zero-trans 3-OMG influx. (A) Data of individuals. Each data point represents the mean of triplicate experiments. The data are presented as 3-OMG transport in fmol/s/106 cells vs caffeine concentration in mM. (B) Pooled data (three patients and three maternal controls) of erythrocyte 3-OMG uptake in response to increasing caffeine concentrations in triplicate experiments. The values from the patients and the maternal controls are calculated as separate data sets. The uptake value in the absence of caffeine is set at 100% (control value). The uptake value at each caffeine concentration is divided by the control value and multiplied by 100 to generate the relative value of 3-OMG uptake in percentage. (C) The data are presented as 3-OMG transport in fmol/s/106 RBC vs theophylline concentration in mM. Each point represents the mean of triplicate experiments in patient 1 or mother 1. Inset, 3-OMG uptake at increasing theophylline concentrations relative to the 3-OMG uptake without theophylline treatment in percentage. Open diamonds represent maternal control data points;closed circles represent patient data points.
Effects of caffeine on zero-trans 3-OMG influx kinetics.
Zero-trans erythrocyte 3-OMG influx kinetics in three patients (1, 3, and 17) and their mothers is determined as a function of substrate concentration (Fig. 4, A–C). The pooled data are expressed as a double reciprocal plot of 3-OMG concentration versus uptake. Using the linear fit model, mean Vmax values are, in fmol/s/106 cells, maternal controls: 2300 ± 498, patients: 802 ± 96 (37 ± 10% of controls, p < 0.01), and mean apparent Km values are, in mM, controls: 2.8 ± 0.3; patients: 2.2 ± 0.2 (79 ± 10% of controls). Addition of 3 mM caffeine to erythrocytes inhibits 3-OMG influx by predominantly decreasing the Vmax values in maternal controls and patients (Fig. 4, A–C). The individual data for Vmax and apparent Km values are summarized in Figure 4, D and E. Vmax values are significantly reduced in all subjects, whereas decrease in Km values is significant only in the three maternal controls and patient 3.
Caffeine effects on zero-trans 3-OMG influx kinetics. Erythrocyte zero-trans influx of 3-OMG (0.6–10 mM, 4°C, 15-s interval) in patients and maternal controls was measured in the presence or absence of 3 mM caffeine. (A) The pooled data (three patients and three maternal controls, four determinations per data point, expressed as mean ± SE) are presented as a double-reciprocal plot of 3-OMG transport velocity (v) in fmol/s/106 cells vs substrate concentration [3-OMG] in mM. Open circles represent patient with caffeine;closed circles represent patient without caffeine. Open squares represent maternal control with caffeine;open diamonds represent maternal control without caffeine. (b) and (c) Pooled kinetic parameters: (B) Vmax, (C) Km. (D) and (E) Individual kinetic parameters: (D) Vmax, (E) Km. Open bars, without caffeine;closed bars, with caffeine. *Significant difference between groups without caffeine treatment and with caffeine treatment (p < 0.01).
Phenobarbital does not significantly potentiate caffeine inhibition on 3-OMG uptake.
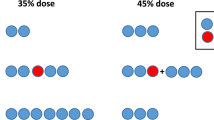
Barbiturate inhibition of glucose or 3-OMG uptake in normal and Glut1DS patients has been reported (18). We investigated possible kinetic interactions between caffeine and phenobarbital. In the fourth patient (15) and the maternal control, erythrocytes are coincubated with 5 mM 3-OMG ± 3 mM caffeine ± 10 mM phenobarbital. The comparison of Figure 5, A and B reveals the expected lower 3-OMG uptake in the patient compared with the control in the absence of caffeine or phenobarbital. Consistent with the prior results, addition of caffeine or phenobarbital alone substantially inhibits 3-OMG uptake in both the patient (Fig. 5A) and the maternal control (Fig. 5B). Combination of caffeine and phenobarbital slightly augments the inhibition compared with each compound alone. This added inhibition, however, is not statistically significant.
Combined effects of caffeine and phenobarbital on erythrocyte 3-OMG uptake. Zero-trans influx of 3-OMG (0–10 mM, 4°C, 15-s interval) into erythrocytes of patient 15 and maternal control was measured. (A) Data from patient. Closed circles represent 3-OMG influx without additional treatment, open triangles represent 10 mM phenobarbital, open squares represent 3 mM caffeine, and asterisks represent 3 mM caffeine + 10 mM phenobarbital. (B) Data from maternal control. Open diamonds represent 3-OMG influx without additional treatment, open triangles represent 10 mM phenobarbital, open squares represent 3 mM caffeine, and asterisks represent 3 mM caffeine + 10 mM phenobarbital.
DISCUSSION
The human brain is dependent upon glucose as an energy source (23, 24). The Glut1DS represents impaired glucose transport across the blood-brain barrier caused by partial Glut1 deficiency that results in hypoglycorrhachia, seizures, and developmental delay (5–8). Identifying potential inhibitors of Glut1 is essential in preventing further impairment of glucose transport in these patients. Methylxanthines have been shown to inhibit glucose transport (11, 12). Our present study represents the first in vitro analysis of methylxanthine inhibition in the Glut1-deficient state and provides further evidence for a significant inhibitory effect of caffeine and theophylline on glucose transport across cell membranes.
In the brain, Glut1 mediates glucose transport 1) across the blood-brain barrier and 2) from the interstitial fluid into astrocytes, oligodendrocytes, and neurons (25). In the first case, transport is close to equilibrium exchange conditions because the glucose concentration is high on both sides of the endothelium. In the second case, intracellular glucose concentration is very low, and transport simulates the zero-trans state. In the Glut1DS, because the glucose concentration in CSF (and presumably brain interstitium) is about half the normal level, conditions will favor zero-trans flux for the endothelium as well. Data in this study have all been obtained under zero-trans conditions, which makes the findings representative of expected conditions in Glut1DS patients.
In the absence of caffeine, the apparent Km for 3-OMG in patients and controls is 2–4 mM (Fig. 4, C and E, and our unpublished data). This range resembles Km values reported in the literature for zero-trans influx of glucose analogues under conditions similar to those used here (25). In our study, caffeine affects glucose uptake in normal controls through noncompetitive mechanisms, as there are significant reductions of both Km and Vmax values (Fig. 4, B and C). In addition, time course studies show apparent inhibition within 5 s of caffeine incubation, indicating direct and extracellular interactions between caffeine and Glut1 molecules. Direct interaction of methylxanthines with glucose transporters has been reported in adipocytes (26). Although the site of such interaction is unknown, data from each of the individuals in this study show a significant reduction in the Vmax values. As for the glucose binding affinity, there is a decrease in Km, indicating an increase in affinity, in all controls and in patient 3 who has similar glucose affinity kinetics compared with the controls (Fig. 4E). The data from patients 1 and 17 support a noncompetitive mode of inhibition, as only Vmax is significantly reduced (Fig. 4D). Because the three patients carry different mutations, it is possible that mutation-specific interactions between Glut1, glucose, and caffeine result in the observed differences in glucose transport kinetics. However, mechanisms such as membrane targeting or protein misfolding cannot be excluded. It is possible that in some of the mutations, the functional deficits in the patients can be traced to defects unique to individual mutant transporters. Our ongoing studies on Xenopus oocytes expressing specific mutant Glut1 forms may provide further insights into the molecular interactions between specific mutant Glut1 and ligands such as glucose and methylxanthines (8, 18, 27). Our current data support the interpretation that a decrease in glucose transport velocity is the principal mechanism by which caffeine inhibits glucose uptake.
Because the human erythrocyte glucose transporter is immunochemically identical to the human brain Glut1 (28), kinetic data obtained in human erythrocytes are likely to reflect transendothelial glucose transport across the blood-brain barrier. The effect of methylxanthines on glucose transport into human erythrocytes of normal individuals has been studied previously (11). Zero-trans d-glucose influx is inhibited after incubation with 0.75 mM isobutyl-methylxanthine, resulting in a 40% reduction in transport velocity and a 50% decrease in glucose affinity (11). The findings in glucose transport velocity agree with our velocity data in controls and patients (Fig. 4). However, caffeine (trimethylxanthine), unlike isobutyl-methylxanthine, when coincubated with erythrocytes does not reduce 3-OMG affinity. In fact, glucose affinity is increased in the presence of caffeine, as discussed above. It is likely that isobutyl-methylxanthine and caffeine induce different Glut1 conformational changes and, thus, result in different affinities for glucose. The net effects of isobutyl-methylxanthine, caffeine, and theophylline on reducing erythrocyte glucose uptake observed in this and other studies remain consistent. The kinetic signature of methylxanthine inhibition on glucose transport is a decrease in Vmax.
In Glut1DS patients, transport function is about half normal, as shown by glucose influx studies (5–8). We have replicated these observations in this study. At this point, it is unclear whether the functional transporters are derived from the wild-type allele only or represent heteromeric combinations of the wild-type and the mutated alleles. The molecular implications of these and other GLUT1 mutations have been described in more detail elsewhere (9).
Caffeine and theophylline are used medically as treatment for infantile apnea. These agents are common dietary components as well. Methylxanthines are used clinically as a diuretic, circulatory and respiratory stimulant, and treatment for headaches. The convulsive properties of methylxanthines have been well documented (14, 15, 29). Intoxication with caffeine and theophylline can lead to seizures at plasma concentrations > 100 μM (30). The convulsive potency of methylxanthines has been attributed to the abnormal elevation of neuronal cAMP concentrations resulting from phosphodiesterase inhibition or adenosine A1 receptor blockade (16). The rise of cAMP levels activates a cAMP-dependent protein kinase, catalyzing the phosphorylation and opening of calcium channels and facilitating excessive transmembrane calcium currents. However, from the present evidence, it appears likely that inhibition of glucose transport also contributes to the convulsive effects of methylxanthines at high doses.
We conclude that methylxanthines inhibit Glut1-mediated glucose transport both in normal individuals and in Glut1DS. These results indicate that impaired glucose transport across the blood-brain barrier in Glut1DS patients would be aggravated further by methylxanthine exposure and, thus, could exacerbate the underlying genetic vulnerability.
Abbreviations
- DHA:
-
dehydroascorbic acid
- GLUT1:
-
facilitated glucose transporter type 1 gene
- Glut1:
-
facilitated glucose transporter type 1 protein
- Glut1DS:
-
glucose transporter type 1 deficiency syndrome
- 3-OMG:
-
3-O-methyl-D-glucose
- >Vmax:
-
maximal transport velocity
- >Km:
-
substrate affinity
References
Pardridge WM, Boado RJ, Farrell CR 1990 Brain-type glucose transporter (Glut-1) is selectively localized to the blood-brain barrier. J Biol Chem 265: 18035–18040
Baldwin SA 1993 Mammalian passive glucose transporters: members of active and passive transport proteins. Biochim Biophys Acta 1154: 17–49
Bell IG, Burant CF, Takeda J, Gould GW 1993 Structure and function of mammalian facilitative sugar transporters. J Biol Chem 268: 19161–19164
Gould GW, Holman GD 1993 The glucose transporter family: structure, function, and tissue-specific expression. Biochem J 295: 329–341
Seidner G, Garcia-Alvarez M, Yeh JI, O'Driscoll KR, Klepper J, Stump TS, Wang D, Spinner NB, Birnbaum MJ, De Vivo DC 1998 Glut-1 deficiency syndrome caused by haploinsufficiency of the blood-brain barrier hexose carrier. Nat Genet 18: 1–4
De Vivo DC, Trifiletti RR, Jacobson RI, Ronen GM, Behmand RA, Harik SI 1991 Defective glucose transport across the blood-brain barrier as a cause of persistent hypoglycorrhachia, seizures, and developmental delay. N Engl J Med 325: 703–709
De-Vivo DC, Garcia-Alvarez M, Ronen G, Trifiletti R 1995 Glucose transport protein deficiency: an emerging syndrome with therapeutic implications. Int Ped 10: 51–56
Klepper J, Wang D, Fischbarg J, Vera JC, Jarjour IT, O'Driscoll KR, De Vivo DC 1999 Defective glucose transport across brain tissue barriers: a newly recognized neurological syndrome. Neurochem Res 24: 587–594
Wang D, Kranz-Eble P, De Vivo DC 2000 Mutational analysis of the GLUT1 (SLC2A1) in Glut-1 deficiency syndrome. Hum Mutat 16: 224–231
Ho YY, Wang D, De Vivo DC 2001 Glucose transporters. In: The Encyclopedia of Molecular Medicine. John Wiley & Sons Publishing, New York (in press)
Challiss JRA, Taylor LP, Holman GD 1980 Sugar transport asymmetry in human erythrocytes—the effect of bulk haemoglobin removal and the addition of methylxanthines. Biochem Biophys Acta 602: 155–166
Steinfelder HJ, Petho-Schramm S 1990 Methylxanthines inhibit glucose transport in rat adipocytes by two independent mechanisms. Biochem Pharmacol 40: 1154–1157
Yasuhara M, Levy G 1988 Caffeine as a potential risk factor for theophylline neurotoxicity. J Pharm Sci 77: 745–747
Ault B, Olney MA, Joyner JL, Boyer CE, Notrica MA, Soroko FE, Wang CM 1987 Pro-convulsant actions of theophylline and caffeine in the hippocampus: implications for the management of temporal lobe epilepsy. Brain Res 426: 93–102
Moraidis I, Bingmann D 1994 Epileptogenic actions of xanthines in relation to their affinities for adenosine A1 receptors in CA3 neurons of hippocampal slices. Brain Res 640: 140–145
Biaggioni I, Puckett PS, Arzubiaga C 1991 Caffeine and theophylline as adenosine receptor antagonists in humans. J Pharmacol Exp Ther 258: 588–593
Dassesse D, Vanderwinden JM, Goldberg I, Vanderhaeghen JJ, Schiffmann SN 1999 Caffeine-mediated induction of c-fos, zif-268, and arc expression through A1 receptors in the striatum: different interactions with the dopaminergic system. Eur J Neurosci 11: 3101–3114
Klepper J, Fischbarg J, Vera JC, Wang D, De Vivo DC 1999 GLUT1 deficiency: barbiturates potentiate haploinsufficiency in vitro. Pediatr Res 46: 677–683
Klepper J, Garcia-Alvarez M, O'Driscoll KR, Parides MK, Wang D, Ho YY, De-Vivo DC 1999 Erythrocyte 3-O-methyl-d-glucose uptake assay for diagnosis of glucose-transporter-protein syndrome. J Clin Lab Anal 13: 116–121
Naftalin RJ, Holman GD 1977 Transport of sugars in human red cells. In: Ellory JC, Lew VL (eds) Membrane Transport in Red Cells. Academic Press, New York, pp 257–300
Klepper J, Vera JC, De-Vivo DC 1998 Deficient transport of dehydroascorbic acid in the glucose transporter protein syndrome. Ann Neurol 44: 286–287
Rumsey SC, Kwon O, Xu GW, Burant CF, Simpson I, Levine M 1997 Glucose transporter isoforms GLUT1 and GLUT3 transport dehydroascorbic acid. J Biol Chem 272: 18982–18989
Chugani HT, Phelps ME, Mazziotta JC 1978 Positron emission tomography study of human brain functional development. Ann Neurol 22: 487–497
Clarke DD, Sokoloff L 1999 Circulation and energy metabolism of the brain. In: Siegel GJ (ed) Basic Neurochemistry: Molecular, Cellular, and Medical Aspects, 16th Ed. Raven Press, New York, pp 645–748
Vannucci SJ, Maher F, Simpson IA 1997 Glucose transporter proteins in brain: delivery of glucose to neurons and glia. Glia 21: 2–21
Kashiwagi A, Huecksteadt TP, Foley JE 1983 The regulation of glucose transport by c-AMP stimulators via three different mechanisms in rat and human adipocytes. J Biol Chem 258: 13685–13692
Pascual JM, Wang D, Kuang K, Yang H, Wen Q, Ma L, Fischbarg J, De Vivo DC 2000 Transport properties of disease-causing GLUT1 mutations. Carden Jennings Publishing, Charlottesville, VA, Society of Neuroscience Conference 26: 814( abstr)
Dick APK, Harik SI, Klip A, Walker DM 1984 Identification and characterization of the glucose transporter of the blood/brain barrier by cytochalasin-B binding and immunological reactivity. Proc Natl Acad Sci USA 81: 7233–7237
Sarro AD, Grasso S, Zappala M, Nava F, De Sarro G 1997 Convulsant effects of some xanthine derivatives in genetically epilepsy-prone rats. Arch Pharmacol 356: 48–55
Rall TW 1985 Central nervous stimulants. In: Gilman AG, Goodman LS, Rall TW, Murad F (eds) The Pharmacological Basis of Therapeutics. McMillan Publishers Company, New York, pp. 589–603
Acknowledgements
The authors thank Pamela Kranz-Eble for skillful assistance in the laboratory and David Diuguid, M.D., Hematology Laboratory, Columbia Presbyterian Medical Center, for blood cell counts. CPD anticoagulant solution was generously provided by Baxter Healthcare Corporation, Fenwal Division, Deerfield, IL 60014, U.S.A.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Ho, YY., Yang, H., Klepper, J. et al. Glucose Transporter Type 1 Deficiency Syndrome (Glut1DS): Methylxanthines Potentiate GLUT1 Haploinsufficiency In Vitro. Pediatr Res 50, 254–260 (2001). https://doi.org/10.1203/00006450-200108000-00015
Received:
Accepted:
Issue Date:
DOI: https://doi.org/10.1203/00006450-200108000-00015
This article is cited by
-
Tune in to the terrific applications of turanose
European Food Research and Technology (2024)
-
Natural Products and Derivatives Targeting at Cancer Energy Metabolism: A Potential Treatment Strategy
Current Medical Science (2020)
-
Crystal structure of a bacterial homologue of glucose transporters GLUT1–4
Nature (2012)
-
Interactions of androgens, green tea catechins and the antiandrogen flutamide with the external glucose‐binding site of the human erythrocyte glucose transporter GLUT1
British Journal of Pharmacology (2003)