Abstract
Blood from seven newborns, a 13-y-old, and seven adult family members with a suspected hemoglobinopathy because of unexplained cyanosis was obtained for analysis to determine Hb oxygen affinity and to characterize and quantify the Hb variants. Their oxygen saturation was 76 to 84%. The P50 was 30.3 ± 2.9 for the newborns and 32.5 ± 2.6 mm Hg for their related adults. In the same order, the plasma erythropoietin was 7.4 ± 2.9 and 15.9 ± 3.7 mU/mL, whereas 2,3-diphosphoglycerate was 16.1. ± 2.9 and 15.9 ± 3.7 μmol/g Hb. In four of the newborns with increased P50, the mother had a normal P50 (27 mm Hg), which indicated a greater maternal oxygen affinity than the fetus with no adverse effects on the fetus. Genetic analysis of α-globin genes demonstrated a heterozygous mutation on the α2 gene [α94(G1)Asp→His] for each of the newborns and their related adults. The same mutation was found on the α1 gene in an adolescent and her father. The mRNA measurements showed that the α2- to α1-globin mRNA mean ratio was 2.5, α2 mutant globin mRNA/total α2-globin mRNA was 45.0%, whereas the α1 mutant globin mRNA/total α1-globin mRNA was 37.8%. The level of α2 mutant globin/total α-globin was 27.3 ± 1%, and α1 mutant globin/total α-globin was 23.8 ± 1%. The percentage of synthesized α2 and α1 mutant globins was 27.5 ± 2 and 26.1 ± 1, respectively. The ratio of the α2/α1 mutant globins was 1.1, which corresponded to a ratio at the mRNA level of α2/α1 of 2.5 ± 0.5, which suggested that there is a less efficient translation of the α2 mRNA than α1 mRNA. The reversal of the physiologic fetomaternal oxygen affinity had no effects on fetal development.
Similar content being viewed by others
Main
A rare mutant Hb with a low oxygen affinity designated as Sunshine Seth [α94(G1) Asp→His] (1) was detected in a series of newborn infants as well as in a 13-y-old and her father. The infants, because of persistent cyanosis, were transferred soon after birth to a neonatal intensive care unit to investigate the cause of their Hb desaturation. The cyanotic infants and their parents provided an opportunity to evaluate the physiologic implications of low oxygen Hb affinity during the perinatal period as well as carry out genetic analysis to further the knowledge of the of human α-globin gene expression.
The two human α-globin genes α1 and α2 are coexpressed in normal erythroid cells and encode identical α-globin protein products. The α2 gene encodes a 2–3-fold higher level of mRNA than the α1 gene (2). Because of the identical α-globin produced, the relative levels of expression are difficult to determine. Despite some data that suggest posttranscriptional/translational modifications balancing the amount of protein expressed from these mRNA (3), it is still controversial how the difference in α2 and α1 mRNA levels are reflected at the protein level (4). Because of a rare occasion in which an identical mutation in both the α1 and α2 genes existed in different individuals, the relative rate of mutant protein production from each of the loci can be determined and compared. These values can be used to evaluate the efficiency of the translation of the α1 and α2 mRNA and to determine the relative contribution of normal α1 and α2 to the total α-globin production.
Blood samples obtained from patients with an Hb oxygen desaturation with a suspected hemoglobinopathy were used to determine their ODC and to measure the effects of Hb desaturation on DPG and erythropoietin levels. The samples were also used to determine their mutant globin chain identification and its quantification and rate of synthesis. Finally, a series of molecular genetic studies such as a selective amplification of α1- and α2-globin genes for sequencing and/or digestion with specific restriction enzymes were carried out to determine the mutation locations, RNase protection assay to determine the relative amounts of α2- and α1-globin mRNA, and reverse transcriptase-PCR (RT-PCR)-ApaL I digestion to quantify the relative amounts of α2 or α1 mutant globin mRNA.
METHODS
During a 5-y period (1994–1999), seven newborns from the same region of the province of Quebec were transferred to the neonatal intensive care unit soon after birth because of persistent cyanosis. The infants were born at term with a mean birth weight of 3350 ± 440 g. They were all appropriate for weight for gestational age. Because of unexplained desaturation and the lack of symptoms, a hemoglobinopathy was suspected. Six parents of these infants and one grandparent with cyanosis were also investigated. More recently, a 13-y-old girl and her father were added to this series because of unexplained cyanosis and desaturation detected in a pediatric clinic. The arterial oxygen saturation by pulse oximetry (Ohmeda oximeter) of these infants and their related adults ranged from 76 to 84%.
Blood samples were obtained to determine the P50 from ODC by use of an ODC Hemox-Analyzer (5). Total globin chain content and the rate of protein synthesis was determined by labeling immature red cells with 3H-leucine and separation of the globins by HPLC (6); as plasma erythropoietin and red cell DPG concentrations were determined by RIA (7) and an enzymatic method, respectively (8). Finally, DNA and mRNA analysis was carried out on the samples as described below.
ODC.
ODC were obtained using the Hemox-Analyzer (TCS Scientific Corp., New Hope, PA, U.S.A.). Fifty microliters of whole blood was added to 4 mL of buffer (135 mM NaCl, 30 mM TES, 5 mM KCl, and NaOH adjusted to pH 7.4 ± 0.02) (TCS buffer; TCS Scientific Corp.), 10 μL of antifoam solution, and 20 μL of 20% BSA. Samples were analyzed immediately upon collection from the patient. Nitrogen (100%) was bubbled through the sample at a constant rate that resulted in complete deoxygenation within 20 min, followed by reoxygenation with air for 15 min. The analyzer measured the oxygen tension with a standard Clark O2 electrode (model 5331 Oxygen Probe; Yellow Springs Instrument Co., Yellow Springs, OH, U.S.A.) and simultaneously calculated the Hb saturation by use of dual-wavelength spectrophotometry. The ODC were recorded during both deoxygenation and reoxygenation. The membrane was deoxygenated and reoxygenated in distilled water for a 12-h period the day before all patient studies. The night before each study day, a sample of fresh adult blood was run as a standardization control.
DNA analysis.
Genomic DNA was isolated using a QIA amp kit (Qiagen) from the blood samples of patients who had an α-globin variant detected by HPLC. The genomic DNA (0.5 μg) was subjected to selective amplification of α1 and α2 DNA using primers in which the upstream primer is common for both α genes- 5′CCACCAAGATCTACTTCCCGC3′ (located in Fig. 1). The α1-specific downstream primer-5′TCAAAGACCACGGGGGTACG3′ (located in Fig. 1) and the α2-specific downstream primer-5′CTTTATTCAAAGACCAGGAAGGG3′ (located in Figs. 1 and 2) amplified specific fragments of 550 bp each. The reaction mixture (50 μL) contained 1X PCR buffer (GIBCO), 25 pmol of primer, 0.2 mM dNTP, 1.5 mM magnesium chloride, 10% DMSO, 5% glycerol, and 1.25 U of Taq polymerase (GIBCO). An initial denaturation for 3 min at 94°C followed by 25 cycles of 94°C for 1 min, 52°C for 1 min, 72°C for 1 min, and a final extension at 72°C for 10 min was done in a Perkin-Elmer thermal cycler. The amplified product was electrophoresed on 2% metaphor agarose. The band containing the PCR fragment was purified from the gel with the Qiaquick gel extraction kit (Qiagen). The α1 and α2 DNA fragments were sequenced using the Thermo Sequenase kit (Amersham Pharmacia Biotech) with the same upstream primer.
Identification of 94 (G→C) mutation in α1-globin gene by PCR. The subject is heterozygous for α1-globin gene and homozygous normal for α2-globin gene. Markers are φΧ174/ Hae III digest. The location of the restriction sites and expected lengths of the DNA fragments are listed below the autoradiographs.
RT-PCR of α2-globin mRNA. Top, Lane 1 and 2 represent the undigested and ApaL I-digested product, respectively, for a normal subject;lanes 3 and 4, undigested and ApaL I-digested product, respectively, for a patient with an α2-globin mutation. Lane 5 contains pBR322DNA/MscI markers. Bottom, Location of the restriction enzyme sites and primers used in this study.
To assess the mutation location on α1 or α2 gene locus, we labeled the DNA fragments by use of the same PCR technique described above by adding 2 μci [α32P]dCTP (3000Ci/mmol) (Amersham) to the reaction mix. Because the mutation abolishes the normal Ava II site at codon 94 and created a new ApaL I site, we used the respective restriction enzymes to evaluate whether the mutation was present in both α locus and both alleles. The specificity of α2 and α1 amplification was confirmed using Msc I restriction enzyme (Bal I isoschizomer), which recognized a site in α1 and not in α2. Ten microliters of PCR product was digested separately with 10 U of Ava II (Amersham Pharmacia Biotech), 10 U of ApaL I (New England Biolabs), and 10 U of Msc I (New England Biolabs) for 2 h at 37°C. Fragments were resolved on 5% polyacrylamide gel and visualized on PhosporImager (Molecular Dynamics).
RNA Analysis.
Total RNA was isolated using RNeasy blood kit (Qiagen). To determine the ratio of mRNA α2/α1, we used RNase protection assay as previously published (9). To quantify the relative amounts of normal and mutant mRNA, we used RT-PCR based on published methods (10). At first, 0.5 μg of RNA was reverse transcribed using 0.5 μg of oligo dT primer (GIBCO) in 1X PCR buffer (GIBCO), 0.2 mM dNTP, 1.5 mM MgC12, 10 mM DTT, 40 U of RNA guard (Amersham Pharmacia Biotech), with 400 U of M-MLV reverse transcriptase (GIBCO) by incubation at 42°C for 60 min followed by inactivation of reverse transcriptase at 94°C for 5 min. The entire reverse-transcribed sample was then PCR amplified in a 50-μL volume containing 25 pmol of common upstream primer-5′CGACAAGACCAACGTCAAGG3′ (located in Fig. 2), 25 pmol of the desired α-specific downstream primer (described above), and 1.25 U of Taq polymerase (GIBCO). Cycling was 94°C for 1 min, 52°C for 1 min, 72°C for 1 min, for 30 cycles and a final extension at 72°C for 10 min done in a Perkin-Elmer thermal cycler. The upstream primer (800 pmol) was labeled to high specific activity with 5 μL of γ32P-ATP (6000ci/mmol) (Amersham), 30 U of polynucleotide kinase (New England Biolabs), and purified on a Qiaquick nucleotide removal kit (Qiagen). Ten microliters of the amplified products was then radioactively labeled with 32P end-labeled upstream primer by one cycle of extension. The reaction mixture contained 1X PCR buffer (GIBCO), 0.1 mM dNTP, 1.5 mM MgCl2, 40 pmol of labeled primer, and 1.25 U of Taq polymerase (GIBCO) in final volume of 20 μL (denaturation for 3 min at 94°C, annealing for 2 min at 52°C, and extension for 10 min at 72°C). Ten microliters of the labeled PCR product was subsequently digested with 10 U of ApaL I (New England Biolabs) for 2 h at 37°C and resolved on a nondenaturing 6% polyacrylamide gel and quantified with PhosphorImager (Molecular Dynamics).
Genotype analysis.
The α-globin gene arrangement was confirmed by PCR amplification of genomic DNA similarly as described by Molchanova et al.(3). Briefly, 0.5 μg of DNA was amplified for 35 cycles with an upper and downstream primer common for both α1 and α2, followed by a 5′ end labeling of the amplified product in a one-cycle PCR. A digestion of the amplified product with the restriction enzyme Apa I, which has a site in α1-IVS-II, allowed the separation and quantitation of α1 and α2 DNA fragments.
The present study was approved by the Institutional Review Board and has been conducted with informed consent.
RESULTS
The P50 values for the carriers of the α2-globin mutant were 30.3 ± 2.9 mm Hg for the newborn infants and 32.5 ± 2.6 for the adults, whereas the mean P50 was 31.3 ± 0.4 for the adults with α1-globin mutant. The plasma erythropoietin and DPG concentrations both in adults and newborns were within normal limits (11–13). These results are shown in Table 1.
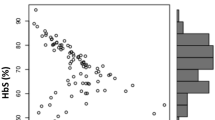
An example of the globin chain separation from a newborn infant by HPLC after 3H-leucine labeling is shown in Figure 3. The split in the α-globin peak identified the mutant α-globin. Fetal Hb comprised 84% of the total Hb, whereas synthesis of fetal Hb was 68% of total Hb synthesis. This level of Hb F synthesis was within the normal range of term infants (14). The mutant α-subunit was 28% of the total α-subunits. As shown on Table 1, the mean α1 mutant globin of the infants included in this study was 23.8%, whereas its synthesis was 26%. Also, the mean α2 mutant globin level was 27% of total α-globin, whereas its synthesis was 27% of total α synthesis.
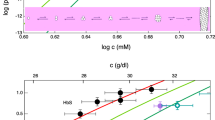
Figure 4 illustrates the Hb ODC from a newborn with a low oxygen affinity hemoglobinopathy in comparison with the normal mother as well as a normal control newborn infant. The normal maternal-fetal oxygen gradient is reversed because the mutation is on the α-globin, and, therefore, it affects the Hb oxygen affinity during most of fetal development. Four of the infants included in this study were born to mothers without a hemoglobinopathy, which meant that these infants had a reversal of their maternal-fetal gradient during fetal life. There was no evidence of any adverse sequelae in these infants.
The results of the sequencing of the regions of the α genes in which the heterozygous mutations occurred are shown in Figure 5, which demonstrates the normal α1 and α2 gene as well as the α1 and α2 mutation in the region of interest. The mutation α94 GAC→CAC results in a replacement of asparagine by histidine. The confirmation of the presence of a heterozygous α1 mutation is demonstrated in Figure 1. Figure 2 illustrates an example of the separation of the products of RT-PCR after ApaL I digestion, which provides the data to determine α2 mutant mRNA ratio to total α2 mRNA. The ratio of the sample shown in Figure 2 was 44.0%. The mean percentages of α2 mutant mRNA in total α2 mRNA and α1 mutant in total α1 mRNA were 45.0 ± 1.3% and 37.8 ± 2%, respectively. The ratio of the α2- to α1-globin mRNA as determined by RNase protection assay ranged from 2.2 to 2.8. The mean values of the ratio were similar in the newborns and the adults (as shown in Table 1).
The variations in α1 and α2 mutant mRNA abundance could not be attributed to deviations from normal αα/αα genotype, because simultaneous amplification and quantification of α1 and α2 gene fragments revealed a ratio of 1.2. Thus, the subjects had a normal genetic complement of αα/αα.
The molecular analysis demonstrated a rare heterozygous mutation [α94(G1)Asp→His] on the α2 gene for all of the infants and their related adults except for a 13-y-old and her father in whom the identical mutation was found on the α1 gene.
DISCUSSION
The transport of oxygen from mother to fetus is believed to be aided by their differences in oxygen affinity. The ODC of paired fetal-maternal samples from 16 species of mammals have been studied showing that fetal oxygen affinity exceeds that of the maternal, the only exception being the cat in which they are the same (15, 16). Although nearly all mammals show such a difference, the usual difference in oxygen affinity between adult and fetal Hb has never been shown to be necessary for a healthy fetal development. The infants in this study were all born at term, appropriate in weight for gestational age and without any evidence of hypoxic erythropoietic stress. They are all followed by a pediatrician and are considered to be growing and developing normally. There are numerous cases described in which maternal blood has a higher oxygen affinity without any detrimental effects on the fetus (17). This difference in oxygen affinity between fetal and adult blood per se may not be an essential requirement for the transfer of oxygen across the placenta.
In this study, a rare mutation [α94(G1)Asp→His] in one of the α2 alleles in a group of related French Canadian families from the same region of the Province of Quebec, Canada, as well as an identical mutant in one of the α1 alleles of a father and daughter of the same ethnic group but unrelated has been studied. The identical mutant could be the result of a gene conversion between duplicated loci or an independent mutation. Normally, when Hb A is oxygenated, β102 Asn forms a hydrogen bond with α94 Asp. An amino acid substitution at this location that is critical to Hb function prevents the formation of the bond between α94 and β102 that normally stabilizes oxyhemoglobin. This phenomenon explains the low oxygen affinity mutants such as Hb Kansas (β102 Asn→Thr), Hb Beth Israel (β102 Asn→Ser), and Hb Titusville (α94 Asp→Asn) (18). The same mechanism is a likely explanation of the low oxygen affinity in the groups of patients of this study with Hb Sunshine Seth (α94 Asp→His). The individuals described in this study have no apparent clinical or hematologic abnormalities. Unexplained cyanosis in association with normal arterial oxygen pressure should prompt investigation for an abnormal Hb mutant and may obviate the need for extensive diagnostic procedures.
Although the protein products of the α2 and α1 genes are identical, methods exploiting the sequence divergence in their noncoding regions have enabled the relative amounts of α2 and α1 mRNA to be determined. The synthesis of an α-globin mutant in a heterozygous individual represents the expression of one of the four α-globin genes. The mean percentage of the abnormal globin in the α2 mutation was 27.5 ± 1% and the α1 mutation 23.8 ± 1%. These values correspond to a ratio of α2 mutant to α1 mutant of 1.1 to 1 at both the protein and protein synthesis level, whereas the mean ratio of α2 and α1 mRNA ranged from 2.3 to 2.5. This finding supports the observations of Molchanova et al.(3) showing that mutations at the two α-globin loci result in small differences on their effects on α-globin synthesis, but does not concord with the work of Liebhaber et al.(4) who carried out in vitro translation studies showing higher output of α2-globin gene in both mRNA and protein.
This mutant caused a reversal of the maternal fetal oxygen affinity gradient with no detrimental effects on fetal growth and development. The presence of an identical mutation on either the α1- or the α2-globin gene in different individuals provided a unique opportunity to substantiate whether there is the existence of a major and minor α-globin locus. The observed base change was confirmed by amplification, sequencing, and/or digestion with specific restriction enzymes in samples from subjects with either α1 or α2 mutant globin. The effect of each of the identical α-globin mutants on the lowering Hb oxygen affinity was the same. The mutant α1- and α2-globin chains comprised close to 25% of the α-globin chains in the circulating red cells as well as the newly synthesized mutant α-globins in the reticulocytes. (If α2-globin were expressed 2.5 times α1-globin, the proportion of mutant α1-globin chains would be in the 10% range.) There was, thus, a 2.5 higher transcription of α2-globin gene compared with the α1-globin gene and a 2.5 higher efficiency in the translation of the α1-globin gene. The result is an almost equal synthesis of α-globin chains by either one of the two genes.
Abbreviations
- ODC:
-
Hb-oxygen dissociation curve
- DPG:
-
2,3-diphosphoglycerate
- P50:
-
Po2 required to achieve a saturation of 50% at pH 7.4 and 37°C
References
Shroeder WA, Shelton JB, Shelton JR, Powars D 1979 Hemoglobin Sunshine Seth - α2 (94(G1)Asp→His) β2 . Hemoglobin 3: 145–159
Liebhaber SA, Wain Kan Y 1982 Different rates of mRNA translation balance the expression of the two human α-globin loci. J Biol Chem 257: 11852–11855
Molchanova TP, Pobedimskaya DD, Huisman THJ 1994 The differences in quantities of α2- and α1-globin gene variant in heterozygotes. Br J Haematol 88: 300–306
Liebhaber SA, Cash FE, Ballas SK 1986 Human α-globin gene expression. The dominant role of the α2-locus in mRNA and protein synthesis. J Biol Chem 261: 15327–15333
Guarnone R, Centenara E, Barosi G 1995 Performance characteristics of Hemox-Analyzer for assessment of the hemoglobin dissociation curve. Haematologica 80: 426–430
Bard H, Widness JA, Ziegler EE, Gagnon C, Peri KG 1995 The proportions of Gγ- and Aγ-globins in the fetal hemoglobin synthesized in preterm and term infants. Pediatr Res 37: 361–364
Georgieff MK, Landon MB, Hedlund B, Faasen AE, Mills MM, Hedlund BE, Faasen AF, Schmidt RL, Ophouen JJ, Widness JA 1990 Abnormal iron distribution in infants of diabetic mothers: spectrum and maternal antecedents. J Pediatr 117: 455–461
Keitt AS 1971 Reduced nicotinamide adenine dinucleotide-linked analysis of 2,3-diphosphoglyceric acid: spectrophotometric and fluorometric procedures. J Lab Clin Med 77: 470–475
Peri K, Gagnon C, Bard H 1998 Quantitative correlation between globin mRNAs and synthesis of fetal and adult hemoglobins during hemoglobin switchover in the perinatal period. Pediatr Res 43: 504–508
Dimovski AJ, Efremov DG, Gu L-H, Huisman THJ 1994 The relative levels of βA and βS mRNAs in Hb S heterozygotes and in patients with HbS-β+-thalassaemia or HbS-β+-HPFH combinations. Br J Haematol 87: 353–356
Cotes PM, Spivak JL 1991 Erythropoietin in health and disease. In: Erslev AJ, Adamson JW, Eschbach JW, Winearls CG(eds) Erythropoietin. The Johns Hopkins University Press, Baltimore, 184–207.
Bard H, Teasdale F 1979 Red cell oxygen affinity, hemoglobin type, 2,3-diphosphoglycerate, and pH as a function of fetal development. Pediatrics 64: 483–487
Bureau MA, Shapcott D, Berthiaume Y, Monette J, Blouin D, Blanchard P, Begin R 1983 Maternal cigarette smoking and fetal oxygen transport: a study of P50, 2,3-diphosphoglycerate, total hemoglobin, hematocrit, and total F hemoglobin in fetal blood. Pediatrics 72: 22–26
Bard H 1975 The postnatal decline of hemoglobin F synthesis in normal full-term infants. J Clin Invest 55: 395–398
Metcalfe J, Bartels H, Moll W 1967 Gas exchange in the pregnant uterus. Physiol Rev 47: 782–838
Novy MJ, Parer JT 1969 Absence of high blood oxygen affinity in the fetal cat. Respir Physiol 6: 144–150
Charache S, Catalano P, Burns S, Jones RT, Koler RD, Rutstein R, Williams RR 1985 Pregnancy in carriers of high-affinity hemoglobins. Blood 65: 713–718
Bunn HF 1994 Sickle hemoglobin and other hemoglobin mutants. In: Stamatoyannopoulos G, Nienhuis AW, Majerus PW, Varmus H(eds) The Molecular Basis of Blood Diseases. WB Saunders, Philadelphia, 207–256.
Author information
Authors and Affiliations
Additional information
Supported by Grant #MT-11552 from the Medical Research Council of Canada.
Rights and permissions
About this article
Cite this article
Bard, H., Peri, K. & Gagnon, C. The Biologic Implications of a Rare Hemoglobin Mutant That Decreases Oxygen Affinity. Pediatr Res 49, 69–73 (2001). https://doi.org/10.1203/00006450-200101000-00016
Received:
Accepted:
Issue Date:
DOI: https://doi.org/10.1203/00006450-200101000-00016