Abstract
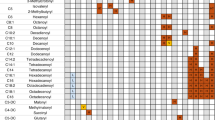
A galactose breath test that quantitates [1-13C]galactose conversion to 13CO2 provides information on the whole body galactose oxidative capacity. As there is little information on the relationship between whole body oxidation and the genotype in patients with galactosemia, we measured the 13CO2 excretion for 2 h after administration of [1-13C]galactose in 37 patients (3–48 y old) with galactose-1-phosphate uridyltransferase (GALT) deficiency and 20 control subjects (3–37 y old). Eleven patients with the common Q188R/Q188R genotype and no detectable erythrocyte GALT activity eliminated <2% of a bolus of [1-13C]galactose as 13CO2 compared with 8.47 to 28.23% in controls. This defines a severe metabolic phenotype. Seven patients with one Q188R allele and a second mutant allele such as L195P, E308K, V151A, M142K, or Q344K and one patient with a K285N/unknown genotype also released <2% as 13CO2 in 2 h. The presence of N314D or S135L as the second mutant allele does not impair total body galactose oxidation, as individuals with the GALT genotype of Q188R/N314D, K285N/N314D, and Q188R/S135L had normal 2-h galactose breath tests. Subjects with S135L/S135L, N314D/N314D, S135L/ΔT2359 as well as other rarer genotypes such as R258C/Y209C, E203 K/IVSC-N314D, K285N/T138M, Q188R/D113N, S135L/F171S, R148W/N314D, and IVSC-N314D/N314D oxidized galactose comparable to controls. The dissociation of residual erythrocyte GALT activity and whole body galactose oxidative capacity is exemplified by blacks with a S135L/S135L genotype and absent erythrocyte GALT activity. An oral 2-h [1-13C]galactose breath test distinguishes severe and variant GALT genotypes and enables delineation of the extent of impaired galactose metabolism in an array of patients who possess diverse GALT mutations. It may prove to be useful in establishing whether a patient is capable of manifesting disease similar to patients with a Q188R/Q188R genotype.
Similar content being viewed by others
Main
Hereditary galactosemia is due to a deficiency in GALT enzyme activity (1). Inherited as an autosomal recessive trait, classic galactosemia is the term frequently used to describe the disease phenotype associated with hepatotoxicity in the infant. The most common genotype producing severe GALT deficiency is the presence of a GALT mutation in which arginine is substituted for glutamine at amino acid 188 (Q188R) (2, 3). However, variant or less severe phenotypes exist even when GALT enzyme activity in erythrocytes is absent. The most notable example is the type in blacks (4, 5) now associated with the S135L allele (6, 7). There is debate as to whether the relatively common Duarte/galactosemia compound heterozygosity state with substantial residual erythrocyte GALT activity (8) due to one N314D allele (9, 10) and one galactosemia allele such as Q188R results in clinical disease. Additionally, the Duarte allele may not decrease enzyme activity by an average of 25% if associated with a 1721 C→T transition in cis that may increase GALT translation (11, 12). As is often the case with nutritional toxicity-genetic diseases, phenotype characterization on clinical and even biochemical grounds is not always helpful because of the interplay among the gene, environmental factors such as dietary lactose, and epigenetic phenomena. For example, patients both with classic and variant types may display comparable degrees of elevation of blood galactose, erythrocyte galactose-1-phosphate, urinary galactitol, and galactonate depending on the amount and duration of lactose intake. Particularly now as over 152 different GALT mutations have been described (13), there is a need to better characterize the metabolic phenotype as well as the clinical status of galactosemic patients with different types of galactosemia.
We previously demonstrated the utilization of [1-13C]galactose to assess whole body oxidation and collection of expired air for measurement of 13CO2 in patients with galactosemia (6, 14, 15). After an i.v. bolus of 1–7 mg/kg, patients homo- or heteroallelic for the Q188R mutation eliminated ≤0.31 and ≤3.5% of the dose as 13CO2 in expired air after 1 and 5 h, respectively. In contrast, control subjects eliminated 3 to 6% and 21 to 47% in 1 and 5 h, respectively. Because the liver is the most important organ for whole body galactose metabolism (16) and blacks were previously shown to have 10% residual hepatic GALT activity (17) despite undetectable erythrocyte GALT activity, it was not surprising that a S135L/S135L patient eliminated as much as 2 and 19% in 1 and 5 h, respectively (6, 7).
Preliminary studies indicated that PO administration of labeled galactose gave results comparable to i.v. dosing (14). We have now validated that earlier work and have studied the usefulness of different time points for collection of 13CO2 in air to assess whole body galactose oxidative capacity. Furthermore, to generate a new model of phenotypic classification of patients with the emphasis on whole body metabolic handling of [1-13C]galactose, we have examined the utility of 2-h PO and i.v. breath tests in a large number of infants, children, and adults with different genotypes.
METHODS
Patients.
Subjects were studied in the outpatient or inpatient General Clinical Research Centers and outpatient clinics of the Children's Hospital of Philadelphia and Emory University. The protocol was approved by the Institutional Review Board of both institutions. Informed consent was obtained from each subject. All of the patients were on a lactose-restricted diet and had not eaten for at least 2 h before administration of [1-13C]galactose. There were 37 patients ranging in age from 3 to 48 y and 20 control subjects (3 to 37 y old). Twelve of the subjects were studied on two to three occasions. The genomic DNA from each of the subjects with reduced erythrocyte GALT activity was analyzed for a GALT gene mutation (2).
Breath test.
During the study period of 50–300 min, the patients were resting in bed or in a chair except for periodic use of a bathroom to void. They were permitted to drink water during the study. Two baseline breath samples were collected, after which a PO or i.v. bolus of 7 mg/kg [1-13C]galactose was administered. Breath samples were collected at 120 min for some subjects and at 50 to 300 min in others. The sample of air exhaled into a breath-collecting bag at each time point was trapped in a vacuum tube and stored at room temperature until analyzed.
Measurement of 13CO2 in air.
In each air sample, the enrichment of 13C in expired CO2 was measured by automated gas-isotope-ratio mass spectrometry (18). Results were expressed as the Δ %versus the limestone standard, PeeDee Belemnite. To determine the micromoles of 13CO2 released into expired air per minute, the CO2 production rate must be measured directly or calculated using the estimated BMR. The Schofield equations were used to calculate the BMR (19). Using a fasting RQ of 0.80, the CO2 production rate was calculated from the Weir equation (20), which relates energy expenditure to CO2 production and O2 consumption. Using the CO2 production and isotopic enrichment values, the 13CO2 production rate was calculated as well as the percentage dose recovered at each time point (21). After integration of the latter by the trapezoidal method, the CUMPCD recovered at 50–300 min was determined. In some instances, the enrichment of 13C in CO2 in samples of expired air was performed by Metabolic Solutions, Inc. (Merimack, NH, U.S.A.).
Data analysis.
Linear regression analysis was used to determine the correlation between the CUMPCD 13CO2 and time, including the correlation coefficient. The difference between the CUMPCD 13CO2 in different groups of subjects was assessed by the t test.
RESULTS
Comparison of PO with i.
v. breath testing.
To more easily carry out the breath testing, particularly in the outpatient clinic setting, we switched to the use of PO breath testing in the course of this study. As a prelude, we studied the differences between elimination of [1-13C]galactose in expired air after a PO versus an i.v. bolus in normal subjects. The results are shown in Table 1 and Figure 1. The cumulative percent of the [1-13C]galactose bolus eliminated as 13CO2 in expired air (CUMPCD 13CO2) at 50, 60, 120, 180, and 300 min after PO and i.v. administration was 2.84 ± 1.98, 4.19 ± 2.82, 17.46 ± 6.72, 20.19 ± 6.62, and 43.00 ± 7.95 for the PO breath test and 3.98 ± 0.81, 5.26 ± 1.25, 14.03 ± 3.73, 24.02 ± 5.64, and 39.78 ± 7.73 for the i.v. test. There was considerable overlap between both groups with no significant differences in CUMPCD 13CO2 at any time point. As shown in Figure 1, there was a highly significant linear relationship between time from 50 to 300 min and the CUMPCD 13CO2 for both groups. The data are shown as the mean ± SD. Linear regression analyses yielded an r2 of 0.978 and 0.998 for the PO and i.v. data, respectively. Each line is straight, the slopes are not different, and the means at each time point are not different. As shown in Table 2, all of the patients with a severe galactose oxidative phenotype eliminated <2% of a PO [1-13C]galactose bolus as 13CO2 in 120 min, comparable to those given the bolus i.v. as we previously published (14, 15). As shown in Table 3, the 13CO2 released by variant subjects given a PO bolus also overlapped with the 2-h CUMPCD elimination results obtained after i.v. dosing. Thus, the results obtained with PO breath testing are comparable to those obtained with an i.v. bolus in both normal subjects and patients. Furthermore, the data obtained with PO breath testing are comparable to our previously published results in normal subjects and patients with galactosemia (6, 14, 15).
Breath testing in subjects with different genotypes versus normal subjects at 120 min.
Based on the percent of elimination of the [1-13C]galactose dose as 13CO2 at 120 min, we divided the patients into those with a severe or variant galactose oxidation deficiency phenotype. Only 19 of the 37 patients tested at 120 min released <2% of the bolus, and all but one possessed either 1 or 2 Q188R alleles. The results for the patients with a severe and variant phenotype are shown in Tables 2 and 3, respectively. The comparison data for the normal subjects are shown in Table 4. Results for both PO and i.v. breath tests are shown. Several of the subjects were tested more than once and results were comparable.
We defined a galactose oxidation deficiency phenotype as follows: patients with a severe phenotype eliminated between 0 and 1.48% of the galactose bolus at 2 h. The mean ± SD CUMPCD 13CO2 was 0.43 ± 0.41 (n = 25). More than half of these subjects were homoallelic for the Q188R mutation. Another eight subjects with a severe phenotype had missense mutations, L195P, K285N, E308 K, V151A, Q344K, M142K, or an unknown mutation in addition to a Q188R allele except for the one patient with a K285N/unknown genotype.
Subjects were defined with a variant phenotype in two separate groups based on the presence or absence of GALT activity in erythrocytes. In both variant phenotypes, the cumulative 13CO2 eliminated in 2 h after the bolus overlapped with a range between 7.31 and 25.81% of the dose and a mean ± SD of 15.44 ± 6.50 (n = 20). The first group (Table 2) were patients whose genotype did not contain the Duarte N314D allele except for one individual in whom an IVSC mutation was in cis with N314D. Their 2-h CUMPCD varied from 8.01 to 22.07% of the dose. The mean ± SD was 13.07 ± 5.12 (n = 11). Five of the nine subjects in this group had one allele that was S135L, which is prevalent in blacks, one of whom was homoallelic for S135L and the others possessing S135L/ΔT2359, S135L/F171S, and Q188R/S135L genotypes. Other genotypes in the group-1 variant phenotype were R258C/Y209C, E203 K/IVSC-N314D, K285N/T138M, and Q188R/D113N. Erythrocyte GALT activity was undetectable in all patients in this group except for the R258/Y209C subject who had greater than 5% residual activity and a Duarte-like isoelectric focusing banding pattern. It is noteworthy that the erythrocyte GALT activity in the majority of non-Duarte variants is indistinguishable from subjects with the severe phenotype. All patients were under optimal dietary control before oxidative studies were accomplished. Erythrocyte galactose-1-phosphate was at therapeutic concentrations, but severe GALT genotypes tended to be higher (i.e. 1.4–5.6 mg %) when compared with less severe forms (0.5–3.1 mg %), but there were no significant differences at the statistical level.
The second variant group consisted of nine subjects who were all compound heterozygotes with the Duarte N314D allele plus a second galactosemic allele such as Q188R or K285N. Six in this group had N314D/Q188R genotypes. As a whole, these subjects with the N314D allele had a 2-h CUMPCD (7.31 ± 25.81) that overlapped with the normal range. They have erythrocyte GALT activity easily detectable in a range of 10 to 25% of normal, which usually but not always distinguishes them from the first variant group. The mean ± SD CUMPCD 13CO2 was 16.72 ± 7.82 (n = 9).
The results for the 20 normal subjects that included 11 children, four adolescents, and five adults are shown in Table 4. Their range of elimination of 8.47 to 28.23% (mean ± SD, 15.75 ± 5.60;n = 26) at 120 min overlaps with both groups of patients with a variant phenotype.
Time-dependent elimination of [1-13C]galactose as13CO2 in patients with classic versus variant phenotypes.
The clear distinction between the whole body oxidative capacity of patients with a severe and a variant phenotype as identified in Tables 2 and 3 is further illustrated in Table 5. This Table shows the summary of the PO and i.v. breath-test results for severe and variant patients at 50 to 300 min in comparison with normal subjects. The mean ± SD CUMPCD 13CO2 at 50, 60, 120, 180, and 300 min for the severe patients was 0.10 ± 0.07, 0.07 ± 0.08, 0.43 ± 0.41, 0.95 ± 0.64, and 3.72 ± 1.88, whereas the comparable results for the variants and normal subjects were 1.45 ± 0.38, 2.17 ± 0.40, 15.44 ± 6.50, 21.13 ± 8.40, 32.99 ± 6.92 and 3.57 ± 1.39, 4.88 ± 1.93, 15.75 ± 5.60, 22.74 ± 5.73, 40.58 ± 7.65, respectively. The means for the severe patients were significantly lower than the means for variants (p < 0.05) and normal subjects (p < 0.05). At the early time points of 50 and 60 min, there may be kinetic differences in metabolic rates between the normal subjects and variant patients, particularly for certain groups such as Q188R/other, but a larger number of patients are required for meaningful statistical analyses.
DISCUSSION
We have shown that the PO [1-13C]galactose breath test is useful in the delineation of the metabolic phenotype in a patient with GALT deficiency. It allows one to establish the degree of impaired total body galactose oxidation in a patient and to evaluate the severity of a given mutation. The latter use is important because some patients with no erythrocyte GALT activity have total body galactose oxidative rates that overlap with normal controls. This is probably related to residual GALT activity in organs such as the liver in which synthesis and degradation of mutant GALT protein reaches a different equilibrium than in erythrocytes that are anucleate (11). The erythrocyte GALT activity, vis-à-vis the black variant with an S135L mutation, is not a reliable predictor of galactose oxidative reserve. Patients with at least one S135L allele can have zero erythrocyte GALT activity but a normal breath test. One would predict that black patients have residual GALT activity in other tissues, and this is indeed the case: they have 10% residual GALT activity in liver (17) and intestine (22). Because of newborn screening, infants with uncommon genotypes can be detected before the advent of overt clinical disease and are placed on a lactose-free formula. The utility of diet therapy for some of these patients has not been established. Because of the plethora of new genotypes in galactosemia, counseling for the parents regarding lifelong diet therapy, prognosis, and the risk of complications will be enhanced by a knowledge of the infant's ability to oxidize galactose. Because the breath test results yield no overlap between the patients with a variant and a severe galactose oxidation deficiency phenotype, a relatively simple 2-h breath test will allow the physician to determine whether an infant with a poorly defined genotype has an oxidative phenotype comparable to the most severe group of galactosemic patients. This should enable some prediction of outcome in infants given early dietary intervention, but further prospective studies related to outcome will be necessary to test this postulate.
Our data show that the PO breath test provides results comparable to the i.v. [1-13C]galactose breath test. After a lag of 50 min or less, the percent of the dose of galactose eliminated in air as 13CO2 increases linearly with time at least up to 300 min whether the dose was given by mouth or i.v. We chose the 2-h time point for study because it both provides delineation of the oxidative phenotype and allows for the execution of a practical test in the clinic setting. The data suggest that multiple time point analyses may allow for a better metabolic characterization of the variant group, but this work is clearly experimental and will require a large number of patients with different genotypes.
The patients with severe or classic galactosemia eliminate <2% of the bolus of [1-13C]galactose as 13CO2 in expired air in 120 min. As we previously reported (14, 15), these are individuals with Q188R/Q188R or Q188R/other genotypes, in which the other allele also represents a severe mutation. With our new studies, we now show that some of the other severe mutations include the L195P, E308K, V151A, M142K, and the Q344K alleles. Whether a homoallelic genotype for one or more of these mutations would also result in a severe metabolic phenotype, let alone a classic disease phenotype, remains to be determined. Given the previously published data on whole body oxidation of either [1-14C]galactose and [1-13C]galactose in subjects with variant conditions (6, 14–16, 23), it is not surprising that genotypes such as the Q188R/N314D, N314D/N314D, K285N/N314D, and S135L/S135L result in normal oxidative capacities at 2 h. Other relatively unique combinations such as the Q188R/S135L, Q188R/D113N, S135L/F171S, R258C/Y209C, E203 K/IVSC-N314D, and the K285N/T138M gave similar 13CO2 elimination rates. The K285N mutation prevalent in Eastern Europe has as severe an expression of impaired galactose oxidation as the Q188R mutation and may produce as severe clinical disease in the neonatal period when present in the homoallelic state.
Whole body galactose oxidative capacity at 2 h does not predict the clinical outcome for all genotypes. For example, the patient with an S135L allele and breath-test results at 2 h that overlap with controls may have evidence of clinical disease in infancy depending on the state of lactose ingestion (4–7). The 2-h breath test could be most useful in establishing which patient will manifest or is capable of manifesting disease similar to the classic patients with a Q188R/Q188R genotype. It will not reveal which patient with a normal oxidative capacity at 2 h after a 7-mg/kg galactose dose manifests abnormal galactose tolerance with ingestion of gram quantities of lactose and clinical disease in early infancy. It may also not serve as a reliable predictor of outcome for some patients exposed to gram quantities of milk lactose during infancy. Because a markedly abnormal galactose tolerance test is associated with classic galactosemia and, thus, potential life-threatening disease, a 120-min breath test result of <2% is probably indicative of a severe impairment in galactose tolerance and accumulation of galactose and its metabolites sufficient to induce disease. The amount and duration of lactose ingestion required to induce clinical disease in a patient with the genotypes associated with a variant oxidative phenotype are unknown. More detailed tracer kinetic studies with [1-13C]galactose in patients may prove helpful in the delineation of the variant phenotype as the simple 2-h breath test does not discriminate between normals and variants.
Abbreviations
- GALT:
-
galactose-1-phosphate uridyltransferase
- BMR:
-
basal metabolic rate
- CUMPCD:
-
cumulative percent of the dose, PO, oral
References
Segal S, Berry GT 1995 Disorders of galactose metabolism. In: Scriver CH, Beaudet AL, Sly WS, Valle D (eds) The Metabolic and Molecular Bases of Inherited Diseases, 7th Ed, Vol I. McGraw-Hill, New York, 967–1000.
Elsas LJ, Langley S, Steele E, Evinger J, Fridovich-Keil JL, Brown A, Singh R, Fernhoff P, Hjelm LN, Dembure PP 1995 Galactosemia: a strategy to identify new biochemical phenotypes and molecular genotypes. Am J Hum Genet 56: 630–639.
Elsas LJ, Langley S, Paulk EM, Hjelm LN, Dembure PP 1995 A molecular approach to galactosemia. Eur J Pediatr 154: S21
Baker L, Mellman WJ, Tedesco TA, Segal S 1966 Galactosemia: symptomatic and asymptomatic homozygotes in one Negro sibship. J Pediatr 68: 551–558.
Mason HH, Turner ME 1935 Chronic galactosemia, report of case with studies on carbohydrates. Am J Dis Child 50: 359–374.
Lai K, Langley SD, Singh RH, Dembure PP, Hjelm LN, Elsas LJ 1996 A prevalent mutation for galactosemia among black Americans. J Pediatr 128: 89–95.
Landt M, Ritter D, Lai K, Benke PJ, Elsas LJ, Steiner RD 1997 Black children deficient in galactose-1-phosphate uridyltransferase: correlation of activity and immunoreactive protein in erythrocytes and leukocytes. J Pediatr 130: 972–980.
Beutler E, Baluda MC, Sturgeon P, Day RW 1965 A new genetic abnormality resulting in galactose-1-phosphate uridyltransferase deficiency. Lancet 1: 353
Elsas LJ, Dembure PP, Langley S, Paulk EM, Hjelm LN, Fridovich-Keil JL 1994 A common mutation associated with the Duarte galactosemia allele. Am J Hum Genet 54: 1030–1036.
Lin HC, Kirby LT, Ng WG, Reichardt JKV 1994 On the molecular nature of the Duarte variant of galactose-1-phosphate uridyltransferase (GALT). Hum Genet 93: 167–169.
Lai K, Langley SD, Dembure PP, Hjelm LN, Elsas LJ 1998 Duarte allele impairs biostability of galactose-1-phosphate uridyltransferase in human lymphoblasts. Hum Mutat 11: 28–38.
Langley SD, Lai K, Dembure PP, Hjelm LN, Elsas LJ 1997 Molecular basis for Duarte and Los Angeles variant galactosemia. Am J Hum Genet 60: 366–372.
Elsas LJ, Lai K 1998 The molecular biology of galactosemia. Genetics Med 1: 40–48.
Berry GT, Nissim I, Mazur AT, Elsas LJ, Singh RH, Klein PD, Gibson JB, Lin Z, Segal S 1995 In vivo oxidation of [1-13C]galactose in patients with galactose-1-phosphate uridyltransferase deficiency. Biochem Mol Med 56: 158–165.
Berry GT, Nissim I, Gibson JB, Lin Z, Elsas LJ, Singh RH, Klein PD, Segal S 1997 Quantitative assessment of whole body galactose metabolism in galactosemic patients. Eur J Pediatr 156: S43
Segal S, Cuatrecasas P 1968 The oxidation of 14C-galactose by patients with congenital galactosemia: evidence for a direct oxidative pathway. Am J Med 44: 340–347.
Segal S, Rogers S, Holtzapple PG 1971 Liver galactose-1-phosphate uridyltransferase: activity in normal and galactosemic subjects. J Clin Invest 50: 500–506.
Schoeller DA, Klein PD 1979 A microprocessor controlled mass spectrometer for the fully automated purification and isotopic analysis of breath carbon dioxide. Biomed Mass Spectrom 6: 350–355.
Schofield WN 1985 Predicting basal metabolic rate, new standards and review of previous work. Hum Nutr Clin Nutr 39C: 5
de Weir JR 1949 New methods for calculating metabolic rate with special reference to protein metabolism. J Physiol 109: 1–9.
Elsas LJ, Ellerine NP, Klein PD 1993 Practical methods to estimate whole body leucine oxidation in maple syrup urine disease. Pediatr Res 33: 445–451.
Rogers S, Holtzapple PG, Mellman WJ, Segal S 1970 Characteristics of galactose-1-phosphate uridyltransferase in intestinal mucosa of normal and galactosemic humans. Metabolism 19: 701–708.
Segal S, Blair A, Topper YJ 1962 Oxidation of 14C labeled galactose by subjects with congenital galactosemia. Science 136: 150–151.
Acknowledgements
The authors thank S.D. Langley, L.N. Hjelm, P.P. Dembure, and K. Muvaledharan for molecular screening and sequencing of GALT genes and the nursing staff of the GCRC of both institutions.
Author information
Authors and Affiliations
Additional information
Supported by grants from the National Institutes of Health, PO1-HD29847, MO1 RR 00240, and MO1 RR 0039, and by the Diasorin-Meretek Breath Test Group.
Rights and permissions
About this article
Cite this article
Berry, G., Singh, R., Mazur, A. et al. Galactose Breath Testing Distinguishes Variant and Severe Galactose-1-Phosphate Uridyltransferase Genotypes. Pediatr Res 48, 323–328 (2000). https://doi.org/10.1203/00006450-200009000-00010
Received:
Accepted:
Issue Date:
DOI: https://doi.org/10.1203/00006450-200009000-00010
This article is cited by
-
Arginine does not rescue p.Q188R mutation deleterious effect in classic galactosemia
Orphanet Journal of Rare Diseases (2018)
-
Galactosemia in the Turkish population with a high frequency of Q188R mutation and distribution of Duarte-1 and Duarte-2 variations
Journal of Human Genetics (2013)
-
Introduction to the Maastricht workshop: lessons from the past and new directions in galactosemia
Journal of Inherited Metabolic Disease (2011)
-
Negative screening tests in classical galactosaemia caused by S135L homozygosity
Journal of Inherited Metabolic Disease (2009)
-
The clinical and molecular spectrum of galactosemia in patients from the Cape Town region of South Africa
BMC Pediatrics (2002)