Abstract
Antenatal administration of glucocorticoids has been shown to improve postnatal lung function after preterm birth in the ovine fetus. Mechanisms of steroid-induced lung maturation include increased surfactant production and altered parenchymal lung structure. Whether steroid treatment also affects lung vascular function is unclear. Because nitric oxide contributes to the fall in pulmonary vascular resistance at birth, we hypothesized that the improvement of postnatal lung function of preterm lambs after treatment with prenatal glucocorticoids may be in part caused by an increase in endothelial nitric oxide synthase (eNOS) activity. To determine whether glucocorticoid treatment increases lung eNOS expression, we measured eNOS protein content by Western blot analysis of distal lung homogenates and immunostaining of formalin-fixed lungs from ovine fetuses delivered at preterm and term gestation after prenatal administration of glucocorticoids. Treatment protocols were followed in which ewes were treated with intramuscular betamethasone (0.5 mg/kg) at single or multiple doses at weekly intervals, and fetuses were delivered at 125, 135, or 145 d gestation. All groups were compared with saline-treated controls. Western blot analysis of whole lung homogenates demonstrated a 4-fold increase in eNOS protein content in lambs treated with repetitive doses of glucocorticoids and delivery at term (145 d;p < 0.002). In addition, a small increase in lung eNOS protein content was seen in lambs treated with a single dose of betamethasone at 128 d gestation with delivery at 135 d gestation. In comparison with control animals, there were no differences in lung eNOS content from the remaining lambs treated with glucocorticoids when delivery occurred at preterm ages (125 and 135 d). Immunostaining showed eNOS predominantly in the vascular endothelium in all vessel sizes. Pattern of staining was not altered by treatment with antenatal glucocorticoids. We conclude that maternal treatment with glucocorticoids increases lung eNOS content after multiple doses and delivery at term gestation. We speculate that antenatal glucocorticoids may up-regulate eNOS but that the timing and duration of steroid administration appears to be critical to this response.
Similar content being viewed by others
Main
RDS contributes significantly to morbidity and mortality in the preterm neonate. Causes of RDS include incomplete structural development of the lung, reduced surfactant production, and the effects of lung injury superimposed on the preterm lung (1, 2). Mortality from RDS has been dramatically reduced during the past 20 y (3), related in part to new therapies such as exogenous surfactant replacement (4–7), new ventilator strategies (8, 9), and maternal antenatal steroid treatment (10). Antenatal steroids have been shown to reduce both the incidence and severity of RDS by up to 50% in preterm infants (11, 12). Other benefits of antenatal steroids include a reduced risk of severe intraventricular hemorrhage (13) and necrotizing enterocolitis (14). Prenatal steroids improve postnatal lung function by altering both lung mechanics and gas exchange, leading to improved compliance and oxygenation (15, 16) and resulting in fewer ventilator days and lower oxygen requirements (17). However, steroids can also alter lung structure, causing decreases in alveolarization and septal wall thickness (15). In addition, although many effects of prenatal steroids have been shown on surfactant production and clearance and on epithelial and airspace maturation in the developing lung, the effect on lung vascular function is unclear.
In newborn infants, survival depends in part on the successful transition of the pulmonary circulation at birth. Persistent pulmonary hypertension of the newborn is a clinical syndrome characterized by sustained elevations of pulmonary vascular resistance after birth, leading to right-to-left shunting of blood across the ductus arteriosus or foramen ovale and resulting in severe hypoxemia (18). Although most preterm infants do not show evidence of pulmonary hypertension, sustained pulmonary hypertension in preterm newborns with severe RDS is associated with high mortality (19). Antenatal steroids have been shown to improve gas exchange through multiple mechanisms; however, it is not known whether they may act in part through altering eNOS expression and NO production. NO release modulates fetal pulmonary vascular tone (20–22) and contributes to the fall in pulmonary vascular resistance at birth in preterm and term lambs (20, 21, 23–26). NOS is an enzyme that exists in three isoforms: neuronal NOS, inducible NOS, and eNOS (27). eNOS is present in the fetal lung (28–30), but mechanisms that regulate eNOS expression are incompletely understood. Because little is known about the mechanisms of pulmonary vasoregulation and postnatal pulmonary adaptation in premature newborns, we propose that steroids may affect both by altering eNOS expression. We hypothesized that the improvement of postnatal gas exchange in preterm lambs after treatment with prenatal glucocorticoids may be in part caused by an up-regulation of eNOS.
METHODS
Animals.
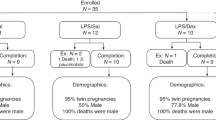
Animal studies were performed in Western Australia using singleton Merino ewes bred by the Western Australia Department of Agriculture according to previously published methods (31), and the studies were approved by the animal care and use committees in Australia and at Children's Hospital Medical Center, Cincinnati. The ewes were date mated for the three protocols and randomized to each protocol and to the groups within each protocol to receive the injection protocols outlined in Figure 1.
For protocol 1, ewes were randomized to receive three doses of saline solution at 104, 111, and 118 d gestation (control;n = 8) or 0.5 mg/kg betamethasone (Celestone Chronodose; Schering, New South Wales, Australia) by intramuscular maternal injection at 104, 111, and 118 d gestation (three doses;n = 7). All animals were delivered of fetuses at 146 d gestation (spontaneous delivery occurs at about 150 d gestation). These animals were studied to confirm that repetitive maternal glucocorticoid treatments cause growth retardation at term (32) and to evaluate lung function after delivery at 146 d gestation.
For protocol 2, ewes were randomized to time of betamethasone treatment to evaluate whether the growth retardation and maturation effects occurred at gestations later than 104 d and after delivery at 135 d gestation. The control group received saline solution by maternal intramuscular injection at 114, 121, and 128 d gestation (n = 7). The single treatment groups received maternal intramuscular injections with 0.5 mg/kg betamethasone at 114 d gestation (one dose, 114 d;n = 8), 121 d gestation (one dose, 121 d;n = 11), or 128 d gestation (one dose, 128 d;n = 5). A fifth group received three repetitive betamethasone doses at 114, 121, and 128 d gestation (three doses;n = 7), and all groups were delivered of fetuses at 135 d gestation.
For protocol 3, one group of ewes received intramuscular saline solution injections at 104, 111, and 118 d gestation (n = 7). A second group of ewes received 0.5 mg/kg betamethasone by intramuscular injection at 104 d gestation and saline solution at 111 and 118 d gestation (one dose maternal;n = 7). A third group received betamethasone at 104, 111, and 118 d gestation (three doses maternal;n = 8). All animals were delivered of fetuses at 125 d gestation for evaluation of the effects of single versus repetitive betamethasone treatments on preterm lung function and growth.
Delivery and postnatal assessments.
Fetal lambs were tracheotomized, delivered, and ventilated according to previously published methods (31). Arterial blood samples were drawn from the placental cord for pH and blood gas analysis. Personnel caring for the lambs after delivery were blinded to the treatments the animals had received before delivery. An arterial catheter was advanced into the descending aorta through an umbilical artery, and lambs received supplemental pentobarbital (15 mg/kg) by slow arterial infusion if spontaneous respirations were noted. The body temperature of each lamb was maintained at approximately 39°C with a radiant warmer.
After a final arterial blood sample 40 min after birth, each lamb was given pentobarbital (30 mg/kg), the tracheal tube was clamped for 3 min to achieve atelectasis for the static lung volume measurement, and the body weight was recorded. The chest of each lamb was opened, the lung was filled with air to 40 cm H2O, which was maintained for 1 min, and the static lung volume was recorded (33). The lungs were removed from the chest, and each lung was weighed. The right lung was inflated and fixed with 10% formaldehyde to a pressure of 30 cm H2O. Tissue was left overnight in 10% formaldehyde at 4°C. Sections were removed from the right upper lobe and transferred to 70% ethanol solution for storage. The left lung was lavaged five times by infusing and withdrawing by syringe sufficient saline solution at 4°C to fully fill the lungs (16). Pieces of the left lung were snap frozen with liquid nitrogen and stored at −70°C until the time of assay.
Western blot analysis for lung eNOS protein.
Western blot analysis was performed using 25 μg of lung protein according to a previously published method (26). Briefly, lung tissue was homogenized, and protein assay was performed by the Bradford method (34). Twenty-five micrograms of lung protein was subjected to SDS-PAGE. After electrophoresis, proteins in the gel were transferred to nitrocellulose membrane. Membranes were blocked in 5% nonfat dry milk, and immunodetection was performed with a MAb to eNOS (Transduction Laboratories, Lexington, KY, U.S.A.), diluted 1:500, a donkey anti-mouse horseradish peroxidase-conjugated secondary antibody, diluted 1:17,000, and ECL Plus (Amersham, Arlington Heights, IL, U.S.A.) detection. Luminescence was determined by exposure to x-ray film for 12–60 s. Densitometry was performed with a scanner and National Institutes of Health Image software.
Western blot analysis with increasing amounts of lung protein from a control sheep showed that the amount of protein (25 μg) used for comparison of control and treatment groups fell within the linear range of the Western blot analysis. Western blot analysis was also performed to examine the reproducibility of replicate samples. The samples for each treatment protocol were analyzed on multiple Western blots, with a standard curve of bovine endothelial cell lysate used for comparisons among the blots. The endothelial cell lysate was loaded at increasing amounts, and all treatment samples fell within the linear range of the standard curve. A developmental analysis was also performed to compare the relative amounts of eNOS protein content among the control groups of the three treatment protocols.
Western blot analysis for KDR/Flk-1.
Western blot analysis was performed for KDR/Flk-1, an endothelial cell marker, to evaluate changes in lung endothelial cell content. Western blot analysis was performed using 50 μg of lung protein as described above. Immunodetection was performed with a rabbit polyclonal antibody to KDR/FlK-1 (Santa Cruz Biotechnology, Santa Cruz, CA, U.S.A.), diluted 1:200, and anti-rabbit horseradish peroxidase secondary antibody, diluted 1:5000.
Histology and immunohistochemical staining for eNOS protein.
Histology and immunohistochemistry for eNOS protein was performed according to a previously published method (35). Briefly, formalin-fixed lung tissue was paraffin-embedded. Hematoxylin and eosin staining was performed on paraffin sections from the lungs of three to seven animals in each study group. At least three sections per lung were assessed for histologic changes. For eNOS immunostaining, slides were dewaxed and then rehydrated. Antigen retrieval was performed. Endogenous biotin in the tissue sections was blocked by glucose/glucose oxidase treatment; sections were blocked with Super Block (Sky Tek, Logan, UT, U.S.A.) and were then incubated with anti-eNOS MAb (Transduction Laboratories) diluted 1:10,000, or an IgG1 negative control (Jackson Laboratories, West Grove, PA, U.S.A.) diluted 1:10,000. Sections were incubated with biotin-labeled anti-mouse secondary antibody (Vector Laboratories, Inc., Burlingame, CA, U.S.A.) at a dilution of 1:200 and then with streptavidin-biotin-horseradish peroxide solution and developed with diaminobenzidine–nickel chloride.
Data analysis.
All data are presented as mean ± SEM. Statistical analysis was performed with the Statview 4.5 software package (Abacus Concepts Inc, Berkeley, CA, U.S.A.). Unpaired t tests were performed on the quantitative data to test for statistical differences between the groups. One-way ANOVA was performed to test for statistical differences between treatment groups within protocols 2 and 3. Data groups were considered as significantly different if p < 0.05.
RESULTS
Lung eNOS protein content.
For each of the Western blots, a single band for eNOS was detected at 140 kD. In protocol 1, lambs treated with repetitive doses of betamethasone at 104, 111, and 118 d gestation with delivery near term at 146 d gestation showed a 4-fold increase in lung eNOS protein content when compared with saline-treated control animals (p < 0.002 versus control;Fig. 2).
In protocol 2, lambs treated with a single dose of betamethasone at 128 d gestation with delivery at 135 d gestation showed a 1.5-fold increase in eNOS protein content when compared with age-matched controls (p < 0.03 versus control). However, there was no difference in lung eNOS protein content in lambs treated with single doses of betamethasone at either 114 or 121 d gestation, or with repetitive doses of betamethasone at 114, 121, and 128 d gestation when compared with control animals (Fig. 3). All animals in this group were delivered at 135 d gestation.
Quantitation of lung eNOS protein content in protocol 2. Lung eNOS protein content of control lambs (n = 7), single-dose treatment with betamethasone at 114 d gestation (114 d;n = 8), single-dose treatment at 121 d gestation (121 d;n = 11), single-dose treatment at 128 d gestation (128 d;n = 5), and multiple-dose treatment (mult. dose n = 7), with delivery at 135 d gestation. *p < 0.03 vs control.
In protocol 3, there was no difference in lung eNOS protein content in lambs treated with either a single dose of betamethasone at 104 d gestation or with repetitive doses of betamethasone at 104, 111, and 118 d gestation with delivery at 125 d gestation when compared with control animals (Fig. 4).
As an alternative method of expressing differences in lung eNOS content, protein content as determined by Western blot was studied relative to whole lung weights. Lung weights for each study group were as follows: protocol 1: control, 168.5 ± 11.2 g; multiple-dose betamethasone, 135.3 ± 8.9 g (*p < 0.05 versus control); protocol 2: control, 131.9 ± 7.1 g; single-dose betamethasone at 114 d, 125.5 ± 3.2 g; single-dose betamethasone at 121 d, 114.7 ± 4.1 g (*p < 0.05 versus control); single dose at 128 d, 129.2 ± 5.2 g; multiple dose, 113.6 ± 8.3 g; protocol 3: control, 110.8 ± 7.5 g; single dose, 81.2 ± 2.9 g (*p < 0.05 versus control); multiple dose, 89.2 ± 5.8 g (*p < 0.05 versus control). Protein content when expressed relative to whole lung weights demonstrated a 3-fold increase in expression after multiple weekly doses of betamethasone with delivery at term (*p < 0.05 versus control), and a 1.5-fold increase after multiple doses of betamethasone with delivery at 135 d gestation (*p < 0.05 versus control).
Total lung protein content.
Total protein content (in grams) was also determined for each lung, and was as follows: protocol 1: control, 4.20 ± 0.44 g; multiple dose, 3.34 ± 0.39 g; protocol 2: control, 4.19 ± 0.23 g; single-dose betamethasone at 114 d, 3.31 ± 0.26 g (*p < 0.05 versus control); single dose at 121 d, 3.18 ± 0.20 g (*p < 0.05 versus control); single dose at 128 d, 2.48 ± 0.29 g (*p < 0.05 versus control); multiple-dose betamethasone, 2.87 ± 0.39 g (*p < 0.05 versus control); protocol 3: control, 4.07 ± 0.36 g; single-dose betamethasone, 2.61 ± 0.25 g (*p < 0.05 versus control); multiple-dose betamethasone, 2.78 ± 0.38 g (*p < 0.05 versus control). Total protein content was decreased after single- or multiple-dose treatment with betamethasone when delivery occurred at preterm gestation, but did not affect total lung protein content when delivery occurred at term gestation.
Developmental analysis.
Relative lung eNOS protein content among control animals delivered according to each of the three protocols was examined. We found no significant difference in lung eNOS protein content among control lambs when delivery occurred at 125, 135, or 145 d gestation.
KDR protein content.
In animals treated with repetitive doses of betamethasone according to protocol 1, Western blot analysis revealed no difference in lung KDR/Flk-1 protein content in steroid-treated animals when compared with control animals. A single band was detected on each Western blot at 220 kD.
Histology and immunohistochemical staining for eNOS protein.
Immunostaining for eNOS was performed on lung tissue for each protocol in both glucocorticoid-treated and control animals. The immunostaining for eNOS was seen exclusively in vascular endothelium, with no apparent staining of airway epithelial cells in any of the study groups. The pattern of staining was similar in all groups, with no differences seen in the glucocorticoid-treated animals when compared with control animals (Figs. 5–7).
Immunostaining for eNOS in control and betamethasone-treated lung tissues with delivery at 145 d gestation. A, hematoxylin and eosin (H&E) staining of control lung. B, H&E staining of lung tissue after repetitive doses of betamethasone. C, immunostaining for eNOS in control lung tissue. D, immunostaining for eNOS in lung tissue after repetitive doses of betamethasone.
Immunostaining for eNOS in control and betamethasone-treated lung tissues with delivery at 125 d gestation. A, H&E staining of control lung. B, H&E staining of lung tissue after repetitive doses of betamethasone. C, immunostaining for eNOS in control lung tissues. D, immunostaining for eNOS in lung tissue after repetitive doses of betamethasone.
Gross histologic examination of tissue samples revealed a marked decrease in alveolar number and secondary septae formation after exposure to antenatal betamethasone, particularly in lambs delivered at preterm gestation (Figs. 6,7).
Immunostaining for eNOS in control and betamethasone-treated lung tissues with delivery at 135 d gestation. A, H&E staining of control lung. B, H&E staining of lung tissue after repetitive doses of betamethasone. C, immunostaining for eNOS in control lung tissue. D, immunostaining for eNOS in lung tissue after repetitive doses of betamethasone.
DISCUSSION
We found that eNOS is increased 4-fold in ovine fetal lungs after repetitive doses of maternal antenatal glucocorticoids and delivery at term. In addition, we found a small increase in lung eNOS protein content in lambs receiving a single dose of betamethasone shortly before delivery occurred at 135 d gestation. In contrast to this marked increase in eNOS content seen in lambs delivered at term, the remaining animals receiving either single or repetitive doses of glucocorticoids and then delivered at preterm gestation (125 and 135 d) showed no increase in lung eNOS protein content. Immunostaining for eNOS demonstrated intense staining of vascular endothelium, with no change in the pattern of staining after antenatal glucocorticoid treatment compared with controls.
These findings are interesting because little is known about the effects of maternal antenatal glucocorticoids on the pulmonary vascular bed. Repetitive doses of glucocorticoids with delivery near term have previously been shown to improve lung compliance and gas exchange (ventilation efficiency index) when compared with controls (31). Although repetitive doses of antenatal glucocorticoids have also been shown to improve arterial Po2 values in fetal lambs after delivery (31), these findings could not be explained purely on the basis of improvement in oxygenation because single doses of glucocorticoids did not improve arterial Po2 values despite an improvement in lung function. These data support the hypothesis that antenatal glucocorticoids improve postnatal lung function in part through an up-regulation of eNOS and therefore increased NO production.
The rationale for repeated doses of antenatal glucocorticoids in women at risk for preterm birth is based on the observation that the changes in pulmonary function after antenatal betamethasone treatment appear to be transient, and persist only for 7 d (36). However, some effects on lung structure (37), somatic growth, and adrenocorticoid function (38) after repeated glucocorticoid treatments can persist until delivery at term. It is interesting to note that in our current study, an up-regulation of eNOS was seen most dramatically in the animals that had received multiple doses of betamethasone during early gestation but with delivery near term. There was a lag period of 28 d after the final dose of betamethasone until delivery at 145 d in the group showing the most striking up-regulation of eNOS.
Lung eNOS protein content was also increased in the lambs receiving a single dose of betamethasone 7 d before delivery at 135 d gestation. It is conceivable that eNOS was also up-regulated in the other animals delivered at preterm gestation, but that this effect, like many of the pulmonary effects seen with antenatal glucocorticoids, was transient and had reversed before delivery. These results suggest that although certain effects of glucocorticoids may be seen early and either reverse or persist until term, still other effects may not be evident until late in gestation.
Previous studies have demonstrated that maternal administration of antenatal glucocorticoids alters lung structure by decreasing alveolarization, decreasing septal wall thickness, and increasing surfactant pools (15). However, few studies have evaluated the effects of glucocorticoids on the pulmonary circulation under normal or pathologic conditions. Initial in vitro studies demonstrated that glucocorticoids increase soluble guanylate cyclase activation in the renal glomeruli of rats (39) and potentiate NO-mediated cGMP production in isolated coronary arteries of preterm fetal lambs (40). In addition, augmentation of NO-mediated relaxation of isolated pulmonary veins from preterm lambs has been demonstrated after treatment with antenatal betamethasone (41). Many of the effects of antenatal glucocorticoids on the pulmonary circulation remain to be studied.
The effects of antenatal glucocorticoids on the pulmonary circulation have been examined in relation to pathologic conditions such as CDH. A recent in vivo study concluded that antenatal treatment with glucocorticoids enhanced the expression of eNOS in the lungs of fetal rats with CDH (42). Untreated rats with CDH had depressed levels of lung eNOS compared with controls. However, after treatment with antenatal dexamethasone, rats with CDH had lung eNOS levels equal to those of normal control animals. Furthermore, antenatal glucocorticoid treatment prevents pulmonary artery structural changes found in experimental models of CDH (43, 44) and diminishes pulmonary immaturity in CDH. Although the effect on the incidence of persistent pulmonary hypertension of the newborn is unknown, this suggests that antenatal glucocorticoid treatment can alter eNOS expression in vivo and may play a role in postnatal pulmonary adaptation.
Although repetitive doses of antenatal betamethasone before delivery near term gestation clearly can up-regulate lung eNOS protein expression, the mechanisms underlying this response are unclear. It is possible that antenatal glucocorticoid treatment exerts a direct effect by dramatically altering lung growth and structure, and that with time, stimulation of endothelial cell growth and proliferation increases endothelial expression of eNOS (45, 46). However, Western blot analysis for lung expression of an endothelial cell marker, KDR, showed no change in protein content in steroid-treated animals when compared with controls. The results of immunostaining for eNOS showed no change in the pattern of staining after glucocorticoid treatment, suggesting that the up-regulation is not explained by stimulation of other cell types within the lung, such as airway epithelium, to express eNOS. Previous studies have demonstrated that isolated systemic vessels incubated in betamethasone also show NO-mediated vasodilation (40), suggesting that glucocorticoids may have direct effects on vascular smooth muscle cells. Whether glucocorticoids increase eNOS expression directly or through indirect mechanisms is unknown.
Antenatal glucocorticoids may potentially affect the pulmonary vascular bed by indirect means through an up-regulation of specific growth factors. Antenatal glucocorticoids have been shown to alter expression of pulmonary epidermal growth factor receptors (47), transforming growth factor β (48, 49), insulin growth factor binding protein (50), and basic fibroblast growth factor (51). At least two of those growth factors susceptible to glucocorticoid modulation, transforming growth factor β and basic fibroblast growth factor, have the capability to increase eNOS protein and mRNA expression in vitro (52, 53). Whether glucocorticoids increase eNOS expression indirectly by altering production or activity of other autocrine or paracrine factors is unknown.
One of the potential limitations of this study is the effect of ventilation and exposure of fetal lambs to hyperoxic conditions at the time of delivery on eNOS expression. Previous studies have shown that both shear stress from ventilation and exposure to oxygen are potent stimulators of NOS (20, 23, 54). Although both glucocorticoid-treated and control animals had exposure to these conditions, levels of eNOS may have been altered from baseline conditions. Cortisol levels gradually rise during late fetal life, and the stress of delivery alone has also been shown to cause a dramatic rise in cortisol levels in human infants (55). The effect of mechanical ventilation on cortisol levels in the ovine fetus is unknown. This alteration in serum cortisol levels may have affected eNOS levels during the study, although control animals were subjected to identical conditions.
We conclude that maternal antenatal glucocorticoids increase lung eNOS protein content 4-fold in the ovine fetus after repetitive weekly doses and with delivery at term gestation. Additionally, lung eNOS protein content is increased in ovine fetuses treated with a single dose of glucocorticoid 1 wk before delivery at 135 d gestation. These findings support our hypothesis that improvement in postnatal lung function and gas exchange after treatment with antenatal glucocorticoids may be in part caused by increased NOS activity. The timing of betamethasone administration during gestation appears to have a critical role in this response. We speculate that antenatal glucocorticoids can up-regulate lung eNOS content, but the mechanism underlying this response and its physiologic implications are uncertain.
Abbreviations
- NO:
-
nitric oxide
- NOS:
-
nitric oxide synthase
- eNOS:
-
endothelial nitric oxide synthase
- RDS:
-
respiratory distress syndrome
- CDH:
-
congenital diaphragmatic hernia
References
Avery ME 1959 Surface properties in relation to atelectasis and hyaline membrane disease. Am J Dis Child 97: 517–523
Stahlman MT 1964 Pathophysiology of respiratory distress in newborn lambs. Am J Dis Child 108: 375–393
Richardson DK, Gray JE, Gortmaker SL, Goldmann DA, Pursley DM, McCormick MC 1998 Declining severity adjusted mortality: evidence of improving neonatal intensive care. Pediatrics 102: 893–899
Jobe AH 1993 Pulmonary surfactant therapy. N Engl J Med 328: 861–868
Horbar JD, Wright LL, Soll RF 1993 A multicenter randomized trial comparing two surfactants for the treatment of neonatal respiratory distress syndrome. J Pediatr 123: 757–766
Vermont-Oxford Neonatal Network. 1996 A multicenter, randomized trial comparing synthetic surfactant with modified bovine surfactant extract in the treatment of neonatal respiratory distress syndrome. Pediatrics 97: 1–6
Schwartz RM, Luby AM, Scanlon JW, Kellogg RJ 1994 Effect of surfactant on morbidity, mortality, and resource use in newborn infants weighing 500 to 1500 g. N Engl J Med 330: 1476–1480
Clark RH, Yoder BA, Sell MS 1994 Prospective randomized comparison of high-frequency oscillation and conventional ventilation in candidates for extracorporeal membrane oxygenation. J Pediatr 124: 447–454
Clark RH, Gerstmann DR, Null DM Jr, deLemos RA 1992 Prospective randomized comparison of high-frequency oscillatory and conventional ventilation in respiratory distress syndrome. Pediatrics 89: 5–12
NIH Consensus Development Panel on the Effect of Corticosteroids for Fetal Maturation on Perinatal Outcomes. 1995 Effect of corticosteroids for fetal maturation on perinatal outcomes. JAMA 273: 413–418
Liggins GC, Howie RN 1972 A controlled trial of antepartum glucocorticoid treatment for the prevention of the respiratory distress syndrome in premature infants. Pediatrics 50: 515–525
Crowley P, Chalmers I, Keirse MJNC 1990 The effects of corticosteroid administration before preterm delivery: an overview of the evidence from controlled trials. Br J Obstet Gynaecol 97: 11–25
Garite TJ, Rumney PJ, Briggs GC, Harding JA, Nageotte MP, Towers CV, Freeman RK 1992 A randomized, controlled trial of betamethasone for the prevention of respiratory distress syndrome at 24 to 28 weeks' gestation. Am J Obstet Gynecol 166: 646–651
Bauer CR, Morrison JC, Poole K, Korones SB, Boehm JJ, Rigatto H, Zachman RD 1984 A decreased incidence of necrotizing enterocolitis after prenatal glucocorticoid therapy. Pediatrics 73: 682–688
Polk DH, Ikegami M, Jobe AH, Sly P, Kohan R, Newnham J 1997 Preterm lung function after retreatment with antenatal betamethasone in preterm lambs. Am J Obstet Gynecol 176: 308–315
Ikegami M, Jobe AH, Newnham J, Polk DH, Willet KE, Sly P 1997 Repetitive prenatal glucocorticoids improve lung function and decrease growth in preterm lambs. Am J Respir Crit Care Med 156: 178–184
Doyle LW, Kitchen WH, Ford GW, Rickards AL, Lissenden JV, Ryan MM 1986 Effects of antenatal steroid therapy on mortality and morbidity in very low birth weight infants. J Pediatr 108: 287–292
Levin DL, Heymann MA, Kitterman JA, Gregory GA, Phibbs RH, Rudolph AM 1976 Persistent pulmonary hypertension of the newborn. J Pediatr 89: 626–633
Walther FJ, Benders MJ, Leighton JO 1992 Persistent pulmonary hypertension in premature neonates with severe respiratory distress syndrome. Pediatrics 90: 899–904
Cornfield DN, Chatfield BA, McQueston JA, McMurtry IF, Abman SH 1992 Effects of birth-related stimuli on l-arginine-dependent pulmonary vasodilation in the ovine fetus. Am J Physiol 262: H1474–H1481
Abman SH, Chatfield BA, Hall SL, McMurtry IF 1990 Role of endothelium-derived relaxing factor during transition of pulmonary circulation at birth. Am J Physiol 259: H1921–H1927
Davidson D, Eldemerdash A 1991 Endothelium-derived relaxing factor: evidence that it regulates pulmonary vascular resistance in the isolated newborn guinea pig lung. Pediatr Res 29: 538–542
Tiktinsky MH, Morin FC III 1993 Increasing oxygen tension dilates fetal pulmonary circulation via endothelium-derived relaxing factor. Am J Physiol 265: H376–H380
Abman SH, Chatfield BA, Rodman DM, Hall SL, McMurtry IF 1991 Maturational changes in endothelium-derived relaxing factor activity of ovine pulmonary arteries in vitro. Am J Physiol 260: L280–L285
Fineman JR, Wong J, Morin FC III, Wild LM, Soifer SJ 1994 Chronic nitric oxide inhibition in utero produces persistent pulmonary hypertension in newborn lambs. J Clin Invest 93: 2675–2683
Le Cras TD, Xue C, Rengasamy A, Johns RA 1996 Chronic hypoxia upregulates endothelial and inducible NO synthase gene and protein expression in rat lung. Am J Physiol 260: L164–L170
Forstermann U, Kleinert H 1995 Nitric oxide synthase: expression and expressional control of the three isoforms. Naunyn-Schmiedebergs Arch Pharmacol 352: 351–364
Halbower AC, Tuder RM, Franklin WA, Pollack JS, Forstermann Abman SH 1994 Maturation-related changes in endothelial NOS immunolocalization in the developing ovine lung. Am J Physiol 267: L585–L591
North AJ, Star RA, Brannon TS, Ujiie K, Wells LB, Lowenstein CJ, Snyder SH, Shaul PW 1994 NOS type I and type III gene expression are developmentally regulated in rat lung. Am J Physiol 266: L635–L641
Kinsella JP, Ivy DD, Abman SH 1994 Ontogeny of NO activity and response to inhaled NO in the developing ovine pulmonary circulation. Am J Physiol 267: H1955–H1961
Jobe AH, Newnham J, Willet K, Sly P, Ikegami M 1998 Fetal versus maternal and gestational age effects of repetitive antenatal glucocorticoids. Pediatrics 102: 1116–1125
Jobe AH, Wada N, Berry LM, Ikegami M, Ervin MG 1998 Single and repetitive maternal glucocorticoid exposures reduce fetal growth in sheep. Am J Obstet Gynecol 178: 880–885
Jobe AH, Polk D, Ikegami M, Newnham J, Sly P, Kohen R, Kelly R 1993 Lung responses to ultrasound-guided fetal treatments with corticosteroids in preterm lambs. J Appl Physiol 75: 2099–2105
Bradford MA 1976 A rapid and sensitive method for the quantitation of microgram quantities of protein utilizing the principle of protein-dye binding. Anal Biochem 72: 248–254
LeCras TD, Tyler RC, Horan MP, Morris KG, Tuder RM, McMurtry IF, Johns RA, Abman SH 1998 Effects of chronic hypoxia and altered hemodynamics on endothelial nitric oxide synthase expression in the adult rat lung. J Clin Invest 101: 795–801
Ikegami M, Polk DH, Jobe AH, Newnham J, Sly P, Kohan R 1996 Effect of interval from corticosteroid treatment to delivery on postnatal lung function in preterm lambs. J Appl Physiol 80: 591–597
Liley H, White RT, Warr RG, Benson BJ, Hawgood S, Ballard PL 1989 Regulation of messenger RNAs for the hydrophobic surfactant proteins in human lung. J Clin Invest 83: 1191–1197
Bradley BS, Kumar SP, Mehta PN, Ezhuthachan SG 1994 Neonatal cushingoid syndrome resulting from serial courses of antenatal betamethasone. Obstet Gynecol 83: 869–872
Lewko B, Wendt U, Stepinski J, Angielski S 1993 Dexamethasone sensitizes soluble guanylate cyclase in the rat renal glomeruli. Biochem Biophys Res Commun 197: 826–832
Gao Y, Zhou H, Raj JU 1996 Antenatal betamethasone therapy potentiates nitric oxide-mediated relaxation of preterm ovine coronary arteries. Am J Physiol 270: H538–H544
Zhou H, Gao Y, Raj JU 1996 Antenatal betamethasone therapy augments nitric oxide-mediated relaxation of preterm ovine pulmonary veins. J Appl Physiol 80: 390–396
Okoye BO, Losty PD, Fisher MJ, Wilmott I, Lloyd DA 1998 Effect of dexamethasone on endothelial nitric oxide synthase in experimental congenital diaphragmatic hernia. Arch Dis Child Fetal Neonatal Ed 78: F204–F208
Taira Y, Miyazaki E, Ohshiro K, Yamataka T, Puri P 1998 Administration of antenatal glucocorticoids prevents pulmonary artery structural changes in nitrofen-induced congenital diaphragmatic hernia in rats. J Pediatr Surg 33: 1052–1056
Okoye BO, Losty PD, Lloyd DA, Gosney JR 1998 Effect of prenatal glucocorticoids on pulmonary vascular muscularisation in nitrofen-induced congenital diaphragmatic hernia. J Pediatr Surg 33: 76–80
Arnal J-F, Yamin J, Dockery S, Harrison DG 1994 Regulation of endothelial NO synthase mRNA, protein, and activity during cell growth. Am J Physiol 267: C1381–C1388
Ziche M, Morbidelli L, Masini E, Amerini S, Granger HJ, Maggi CA, Geppetti P, Ledda F 1994 NO mediates angiogenesis in vivo and endothelial cell growth and migration in vitro promoted by substance P. J Clin Invest 94: 2036–2044
Sadiq HF, Devaskar UP 1984 Glucocorticoids increase pulmonary epidermal growth factor receptors in female and male fetal rabbit. Biochem Biophys Res Commun 119: 408–414
Jaskoll T, Choy H, Melnick M 1996 The glucocorticoid-glucocorticoid receptor signal transduction pathway, transforming growth factor-beta, and embryonic mouse lung development in vivo. Pediatr Res 39: 749–759
Wang J, Kuliszewski M, Yee W, Sedlackova L, Xu J, Tseu I, Post M 1995 Cloning and expression of glucocorticoid-induced genes in fetal rat lung fibroblasts. J Biol Chem 270: 2722–2728
Mouhieddine OB, Cazals V, Kuto E, LeBouc Y, Clement A 1996 Glucocorticoid-induced growth arrest of lung alveolar epithelial cells is associated with increased production of insulin-like growth factor binding protein-2. Endocrinology 137: 287–295
Mesinger C, Zeschnigk C, Grothe C 1996 In vivo and in vitro effect of glucocorticoids on fibroblast growth factor (FGF)-2 and FGF receptor 1 expression. J Biol Chem 271: 16520–16525
Inoue N, Venema RC, Sayegh HS, Ohara Y, Murphy TJ, Harrison DG 1995 Molecular regulation of the bovine endothelial cell nitric oxide synthase by transforming growth factor-beta 1. Arterioscler Thromb Vasc Biol 15: 1255–1261
Kostyk SK, Kourembanas S, Wheeler EL, Medeiros D, McQuillan LP, D'Amore PA, Braunhut SJ 1995 Basic fibroblast growth factor increases nitric oxide synthase production in bovine endothelial cells. Am J Physiol 269: H1583–H1589
McQueston JA, Cornfield DN, McMurtry IF, Abman SH 1993 Effects of oxygen and exogenous l-arginine on endothelium-derived relaxing factor activity in the fetal pulmonary circulation. Am J Physiol 264: H865–H871
Murphy BE 1982 Human fetal serum cortisol levels related to gestational age: evidence of a midgestational fall and a steep late gestational rise, independent of sex or mode of delivery. Am J Obstet Gynecol 144: 276–282
Author information
Authors and Affiliations
Rights and permissions
About this article
Cite this article
Grover, T., Ackerman, K., le Cras, T. et al. Repetitive Prenatal Glucocorticoids Increase Lung Endothelial Nitric Oxide Synthase Expression in Ovine Fetuses Delivered at Term. Pediatr Res 48, 75–83 (2000). https://doi.org/10.1203/00006450-200007000-00014
Received:
Accepted:
Issue Date:
DOI: https://doi.org/10.1203/00006450-200007000-00014
This article is cited by
-
Effect of perinatal glucocorticoids on vascular health and disease
Pediatric Research (2017)
-
Factors relating caesarean section to persistent pulmonary hypertension of the newborn
World Journal of Pediatrics (2017)
-
Antenatal betamethasone improves postnatal transition in late preterm lambs with persistent pulmonary hypertension of the newborn
Pediatric Research (2013)