Abstract
IgA nephropathy is one of the most common forms of glomerular disease. Nearly 25% of affected patients progress to end-stage renal disease over a 20-25-y follow-up period. IgA-containing immune complexes stimulate oxygen-free radical production by mesangial cells in vitro. The excessive oxidant stress may mediate glomerular injury in this disorder. Therefore, we studied whether dietary supplementation with the antioxidant agent, vitamin E, attenuates renal disease in an experimental model of incipient IgA nephropathy with mild kidney inflammation. IgA nephropathy was induced in male Lewis rats by oral immunization with 0.1% bovineγ-globulin (BGG)-containing drinking water for 8 wk. At the completion of this period, animals received BGG, 1 mg/dose i.v., on three successive days. Experimental rats (n = 10) received a specially formulated diet containing 100 IU of vitamin E/kg of chow, whereas control animals(n = 10) were fed chow containing 30 IU of vitamin/kg of chow. The BGG immunization regimen induced mesangial IgA deposition in all rats. Vitamin E supplementation resulted in a nearly 5-fold increase in the serum vitamin E concentration. Vitamin E-treated rats gained more weight and had a lower incidence of hematuria, 20% versus 80% (p < 0.03). Moreover, proteinuria was decreased by 50%, and reduced renal plasma flow was restored to normal, compared with untreated rats with IgA nephropathy. Glomerular hypertrophy occurred in animals with IgA nephropathy, but less so in those receiving vitamin E supplementation. Renal cortical malondialdehyde content was reduced from 1.55 ± 0.10 to 1.22 ± 0.09 nmol/mg of protein (p < 0.01) in rats fed the vitamin E-enriched diet. Finally, renal transforming growth factor-β1 gene expression was reduced by 34% in rats with IgA nephropathy receiving vitamin E treatment (p< 0.05). We conclude that experimental IgA nephropathy is associated with increased renal oxidant injury. Dietary treatment with the antioxidant agent, vitamin E, attenuated renal functional and structural changes in this experimental glomerulopathy. These studies support the importance of clinical trials for the evaluation of the efficacy of antioxidant therapy in patients with IgA nephropathy.
Similar content being viewed by others
Main
IgA nephropathy is among the most common glomerular disorders(1, 2). This diagnosis is made in 10-20% of renal biopsies that are performed for the evaluation of hematuria and/or proteinuria(3, 4). IgA nephropathy was originally considered to be a benign disorder that posed minimal risk for the development of chronic renal failure. However, it is now acknowledged that approximately 1 in 4 affected patients slowly progress to end-stage renal disease over a 20-25-y follow-up period(1–6). There are no proven therapies that reverse the immunologic abnormalities or that consistently retard the course in those patients with IgA nephropathy who manifest progressive loss of kidney function(7).
The pathogenesis of IgA nephropathy remains unclear(1, 2, 8, 9). In a wide variety of renal diseases, excessive oxidant injury contributes to glomerular damage(10). Recent studies indicate that IgA-containing immune complexes stimulate production of oxygen free radicals by mesangial cellsin situ(11). Peripheral polymorphonuclear leukocytes isolated from patients with IgA nephropathy generate increased amounts of superoxide radicals. In parallel with enhanced superoxide production, aggregated IgA induces Fcα receptor expression in leukocytes(12). Both of these findings were correlated with the amount of proteinuria in patients with IgA nephropathy(12). In view of these findings, we conducted experiments to determine: 1) whether there is increased renal lipid peroxidation in an experimental model of IgA nephropathy and 2) if dietary vitamin E supplementation could attenuate glomerular injury in this disease state.
METHODS
Animals. Male Lewis rats, purchased from Harlan (Indianapolis, IN), were maintained in standard cages at 25 °C with a 12-h light-dark cycle. Animals were provided chow and water to drink ad libitum for 1 wk before initiation of the studies. Rats weighed 130-155 g at the start of the experiments.
Experimental model of IgA nephropathy. IgA nephropathy was induced according to the procedure of Gesualdo et al.(13). Briefly, rats were orally immunized for 8 wk with a 6 mM HCl solution, containing 0.1% BGG, as the drinking water. Animals were then challenged with 1 mg of BGG, infused i.v. on three successive days.
Rats with IgA nephropathy were randomly assigned to an experimental group fed a vitamin E-enriched diet containing 100 IU of the antioxidant/kg of chow. The pelleted diet was custom made (ICN Biomedical, Cleveland, OH) and was stored at 4 °C. Control animals received food containing 30 IU of vitamin E/kg of chow. Except for the vitamin E content, the composition and protein content (22%) of the two diets was identical. Periodic testing of vitamin E-supplemented chow indicated that there was no alteration in the nutritional composition, bacterial or fungal contamination, or increased rancidity(Pharmichem Testing Services, Inc., Tinley Park, IL).
The following groups of animals were included in this study; group I, IgA nephropathy + standard chow (n = 10); group II, IgA nephropathy + vitamin E-enriched chow (n = 10); group III, normal rats + standard chow (n = 6); and group IV, normal rats + vitamin E-enriched chow(n = 4).
The experimental vitamin E-supplemented diet and the oral BGG immunization regimen were begun at the same time. Because weight gain was similar in the two groups of rats with IgA nephropathy, pair feeding was not used in these studies. Because rats consumed an average of 20 g of chow/d, the vitamin E-enriched diet provided 5-10 IU of vitamin E/kg of BW in excess of the daily intake on the standard formulation.
The normal animals were provided the 6 mM HCl solution but without BGG for drinking water.
Rats were weighed, and blood pressure was measured at the onset of the study and after 8 wk in the awake conscious state using a tail cuff plethysmography apparatus (Narco BioSystems, Houston, TX). Animals were placed in individual metabolic cages (Nalge, Rochester, NY) and timed urine samples were collected for determination of osmolality, protein, albumin, and creatinine concentrations before induction of IgA nephropathy, and 8 wk later, after completion of the 3-d i.v. immunization protocol. Rats were given free access to water but not food while they were in the metabolic cages. A fasting blood sample was obtained at the end of the urine collection for measurement of hematocrit, serum Na+, creatinine, cholesterol, triglyceride, and albumin concentrations.
Inulin and PAH clearances. At the conclusion of the 8-wk observation period, rats were anesthetized with Inactin (100 mg/kg BW) and placed on a heated animal operating table. Body temperature was monitored with a YSI telethermometer and maintained at 36.5-37.5 °C throughout the study. A tracheostomy was performed, and the left external jugular vein was cannulated with PE-50 polyethylene tubing for infusion of [3H]inulin and [14C]PAH. A suprapubic cystotomy was performed for collection of urine into tared test tubes. After preparation of the animal, 0.2 mL of a 0.9% saline solution containing 12.5 mCi [3H]inulin/mL and 12.5 mCi[14C]-PAH/mL was injected as a priming dose, followed by infusion of the same solution at a rate of 0.02 mL/min. After a 30-min equilibration period, three timed 30-min urine collections were made, and midpoint blood specimens were obtained via the cut tail vein. Serum and urinary activities of[3H]inulin and [14C]PAH were determined with a liquid scintillation counter (LKB Rackbeta). Inulin and PAH clearances were calculated from the standard equation, and the data are expressed as milliliters/min/100 g of BW(14).
Histopathology examination. Rats were killed at the completion of the clearance studies by injection of pentobarbital, 50 mg/kg of BW, and exsanguination. Kidneys were immersion-fixed in buffered 10% formalin solution and stained with hematoxylin-eosin and periodic acid-Schiff reagents. Segmental sclerosis was defined as localized collapse of capillary lumina and replacement with eosinophilic hyalinized material, occasionally accompanied by adhesions to Bowman's capsule. The number of glomeruli with segmental sclerosis was expressed as a percentage of the total number of glomeruli which exceeded 250 in each sample. The tubules and interstitium throughout the kidney were examined for dilatation, intratubular casts and tubular atrophy, interstitial infiltration with mononuclear cells, and replacement with fibrosis. The degree of tubulointerstitial changes was graded on a scale from 0 to 3+ as follows: 0, normal kidney; 1+, mild abnormalities affecting <25% of the renal parenchyma; 2+, moderate, 25-50% involvement; and 3+, severe,>50% of the kidney manifested abnormalities. The pathologist who examined the specimens was unaware of the group assignments of the individual animals.
Glomerular planar area was determined by surveying 40-50 glomeruli in each kidney specimen with a computerized digitizing pad (Micro-plan II, Laboratory Computer Systems, Inc., Natick, MA). Glomeruli throughout the cortex with clear delineation of the hilar region were included in this analysis.
Immunofluorescence examination of the renal tissue was performed by staining snap frozen sections with FITC-labeled anti-rat IgA antibodies (1:100 dilution) (Bethyl Laboratories, Montgomery, TX).
mRNA isolation and Northern blotting. Total RNA was isolated from renal cortical tissue using the Trizol reagent (Life Technologies, Inc.), quantitated spectrophotometrically at OD 260/280, and 20-μg aliquots were applied to a denaturing 0.8% agarose gel. The integrity of the RNA and the comparable sample loading was assessed by ethidium bromide staining of the gels and visual inspection of the 28 and 18 S RNA bands. The abundance of the TGF-β1 mRNA was determined using an RNase protection assay(15) with a rat TGF-β1 probe (catalog no. 63197, ATCC, Rockville, MD). A rat glyceraldehyde-3-phosphate dehydrogenase probe(catalog no. 7432, Ambion, Austin, TX) was used as an internal standard.
Analytic methods. Serum Na+, glucose, creatinine, cholesterol, and triglyceride concentrations and urinary Na+ and creatinine determinations were made using an automated analyzer (Beckman, Fullertown, CA). Serum and urinary albumin concentrations were assayed with the bromcresol green binding reagent (Sigma Chemical Co., St. Louis, MO). Hematuria was determined and quantitated by dipstick testing of the timed urine samples (Ames Labstix, Miles, Elkhart, IN).
Serum vitamin E concentrations were determined using an HPLC method(16). Briefly, 250-μL samples were mixed with 750μL of a 1% (wt/vol) solution of sodium ascorbate and 2 mL of absolute ethanol. Five milliliters of n-hexane were added to extract fat-soluble vitamins and the n-hexane phase was removed and evaporated under N2. The residue was dissolved in 1 mL of the mobile phase, 80:20 methanol:toluene, and 200 μL were injected into an HPLC system consisting of a Waters model 510 pump and 490 programmable multiwavelength detector at 292 nm at a flow rate of 1.5 mL/min. Data were collected with a Shimadzu integrator. Separation was performed on Supercosil LC-18 25 cm column with a Waters Guard-Pak μ-Bondapak precolumn module. Results are reported as μg of α-tocopherol/dl serum.
Urinary protein concentration was measured using the Coomassie Blue binding reagent (Bio-Rad, Richmond, CA). Urinary osmolality was determined with a vapor pressure osmometer (Wescor, Logan UT).
Portions of renal cortex and liver were homogenized in 1.15% KCl solution(1:9 wt/vol) for assay of malondialdehyde content as described by Ohkawaet al.(17). A reaction mixture containing 0.2 mL of sample, 0.2 mL of 8.1% SDS, 1.5 mL of 20% acetic acid adjusted to pH 3.5 with NaOH, and 1.5 mL of 0.8% aqueous solution of thiobarbituric acid was brought up to 4 mL with distilled water. The mixture was heated for 60 min at 95 °C and then cooled with tap water, after which 1 mL of water and 5 mL of a mixture of n-butanol and pyridine (15:1, vol/vol) were added. The sample was shaken vigorously and centrifuged at 4,000 rpm for 10 min, and the organic layer was removed. Absorbance was measured at 532 nm, using 1,1,3,3-tetramethoxypropane as a standard. The tissue lipid peroxide level was expressed as nanomoles/mg of protein.
The level of conjugated dienes was determined using the procedure of Massey and Burton(18). Renal tissue was homogenized in 5 mL of PBS containing 0.01 M EDTA and 5% trichloroacetic acid. Samples were centrifuged at 2000 × g for 10 min, and the pellets were extracted twice with 3 mL of chloroform:methanol (2:1, vol/vol). Two milliliters of distilled water were added, samples were vortexed, and the aqueous phases were aspirated. The lipid extracts were dried under a N2 stream and redissolved in 1-2 mL of acetonitrile. Absorbance was monitored at 235 nm, and the amount of conjugated dienes was expressed as AU/mg of protein.
Statistical analysis. The differences between groups were analyzed using the t test and analysis of variance where appropriate. The experimental findings were considered statistically significant if p < 0.05.
RESULTS
There were no differences between the two pairs of experimental groups,i.e. groups I and II and groups III and IV, in body weight, blood pressure, hematocrit, serum albumin, BUN, creatinine, or triglyceride concentrations at the onset of the study (Tables 1 and 2). Rats with IgA nephropathy treated with vitamin E (group II) had a lower cholesterol concentration before initiating the experimental diet, 105± 6 mg/dL versus 137 ± 3 mg/dL (p < 0.05) than animals fed standard chow (group I) (Table 2).
One rat in each group of animals with IgA nephropathy had more than trace hematuria when the BGG immunization regimen was started. Urinary protein excretion was also similar in the two groups at the start of the study, 0.40± 0.02 in group I versus 0.48 ± 0.04 mg/mg creatinine in group II.
After 8 wk, vitamin E-treated rats with IgA nephropathy gained 18% more weight than animals fed standard chow (p < 0.01)(Table 1). There was no difference in kidney weight among rats with IgA nephropathy fed standard chow (group I), 2.57 ± 0.08 g or vitamin E-enriched food (group II), 2.52 ± 0.05 g. Dietary vitamin E supplementation resulted in a nearly 5-fold elevation in serum vitamin E concentration, 351 ± 63, group I versus 1571 ± 209μg/dL, group II, p < 0.01. After 8 wk, vitamin E-supplemented rats with IgA nephropathy had a higher hematocrit; in addition, BUN and serum cholesterol and triglyceride concentrations were within the normal range but elevated compared with animals in group I (Tables 1 and 2). Examination of freshly voided urine samples indicated that the incidence of greater than trace hematuria was decreased from 80% in untreated rats with IgA nephropathy to 20% in vitamin E-treated animals with IgA nephropathy, p < 0.03. Moreover, urinary protein excretion was lowered from 0.97 ± 0.09 (group I) to 0.48 ± 0.04 mg/mg creatinine in animals given the high vitamin E diet (group II), p< 0.002 (Fig. 1). Proteinuria increased above the initial value in all 10 rats fed standard chow; in contrast, among the animals in group II, urinary protein excretion increased slightly in three rats and remained the same or declined in the other seven.
At the completion of the study period, indices of renal function were 16-18% higher in vitamin E-treated animals and comparable to values in normal rats (Fig. 2, see below). Clearance measurements of GFR and RPF indicated that the increase in RPF, but not GFR, was statistically significant (p < 0.03). These findings were similar regardless of whether renal function was expressed per 100 g of BW or per g of kidney weight.
Renal malondialdehyde content was significantly higher in untreated rats with IgA nephropathy (group I) compared with normal animals fed standard chow(group III) (p < 0.01) (Table 3). Provision of vitamin E-enriched chow for 8 wk reduced lipid peroxidation in both the kidney and liver of rats with IgA nephropathy. Thus, renal cortical malondialdehyde content was 21% lower and hepatic malondialdehyde was 31% lower in rats in group II versus group I, p < 0.01(Table 3). To confirm that the decreased renal malondialdehyde content reflected changes in lipid peroxidation, the amount of conjugated dienes was measured in the lipid extract of kidney specimens obtained from the two groups of rats with IgA nephropathy. Dietary vitamin E supplementation was associated with a 25% reduction in conjugated diene content from 20.1 ± 1.9 AU/mg of protein in group I to 15.1 ± 0.9 AU/mg of protein in group II, p < 0.05.
Immunohistopathologic examination of renal tissue indicated comparable intensity of IgA deposits, ranging from trace to 2+, in mesangial regions of rats in groups I and II. Provision of the vitamin E-enriched diet did not alter the amount of Ig deposition in the glomeruli. In addition, the degree of mesangial hypercellularity, segmental glomerulosclerosis, and interstitial fibrosis was similar among all animals with IgA nephropathy. However, there was significantly more glomerular hypertrophy in group I, 69 ± 2versus group II, 62 ± 1 × 10-3 mm2,p < 0.001 (Fig. 3).
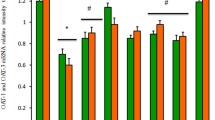
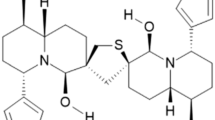
There was an inverse relationship between serum vitamin E concentrations and the amount of proteinuria (r = -0.69, p < 0.005)(Fig. 4). Although there was no correlation between serum vitamin E concentration and renal cortical malondialdehyde content, there was a direct relationship between lipid peroxidation of the kidney tissue and the degree of glomerular hypertrophy (r = 0.49, p < 0.02). The abundance of renal mRNA for TGF-β1 was increased in rats with IgA nephropathy (n = 10) compared with normal rats (n = 3). Administration of the vitamin E-enriched diet for 8 wk to rats with IgA nephropathy reduced steady state renal gene expression of TGF-β1 by 34% to the level observed in normal animals, 14.9 ± 2.3 in untreated (group I) versus 9.9 ± 0.2 AU in vitamin E-treated (group II),p < 0.05 (Fig. 5).
Feeding the high vitamin E diet to normal rats raised the serum vitamin E concentration from 1152 ± 29 (group III) to 1774 ± 98 μg/dL(group IV), p < 0.05. Except for a higher serum glucose concentration in the vitamin E supplemented rats after 8 wk, the dietary treatment had no effect on somatic or renal growth, serum biochemical values, or the various measures of renal function and structure(Tables 1 and 2; Figs. 1 and 3). In the normal rats, hematuria was not detected in those fed standard chow and was trace in one of the four animals fed the vitamin E-enriched food. Dietary vitamin E supplementation did not change GFR, 1.09 ± 0.04 (group III) and 1.13 ± 0.06 mL/min/100 g of BW (group IV) or RPF, 3.24 ± 0.13 (group III) and 3.26 ± 0.15 mL/min/100 g of BW (group IV). Administration of vitamin E did not alter renal content of TGF-β1 mRNA in normal animals (n = 3, each group) (Fig. 5). The only change induced by the dietary manipulation in normal rats was a reduction in renal and hepatic malondialdehyde content(Table 3). However, there was no effect of vitamin E supplementation on renal conjugated diene content in normal rats, 16.7± 0.4 (group III) versus 17.9 ± 0.2 AU/mg of protein(group IV).
DISCUSSION
Our findings indicate that administration of a diet that is modestly enriched in vitamin E ameliorates renal function and prevents structural changes in an experimental model of incipient IgA nephropathy. This protective effect was associated with a reduction in renal cortical malondialdehyde content and decreased abundance of TGF-β1 mRNA in the kidney. To the best of our knowledge, this is the first demonstration that oxygen free radical injury probably contributes to the pathogenesis of experimental IgA nephropathy and that antioxidant therapy can decrease glomerular dysfunction.
The model of IgA nephropathy used in these experiments takes advantage of protracted mucosal immunization to induce mesangial abnormalities in rats. Unlike other models of IgA nephropathy that require injection of IgA immune complexes or other antigens(19–21), this one may be more relevant to human disease in which mucosal stimulation of IgA synthesis and secretion have been documented(8, 9). Treatment with vitamin E had no effect on the extent of mesangial IgA deposition. Therefore, it is unlikely that antioxidant therapy altered the immunologic basis of the disease; instead, it inhibited the subsequent inflammation in glomeruli.
The renal dysfunction observed in this model is characteristic of the initial stages of IgA nephropathy. The glomerular injury is mild and is manifested as hematuria, low grade proteinuria, and a modest reduction in GFR and RPF. Our findings suggest that vitamin E treatment attenuates oxidant-mediated inflammation in this early phase of the disease. Additional studies are required to discern if antioxidant therapy can prevent progressive renal damage.
At present, there is only in vitro or indirect in vivo evidence in favor of a role of reactive oxygen molecules in the development of IgA nephropathy. Exposure of cultured mesangial cells to IgA-containing immune complexes results in increased production of superoxide radicals(11). Polymorphonuclear leukocytes isolated from patients with IgA nephropathy have increased superoxide production, which correlates with the level of proteinuria(12). In addition, the induction of the Fcα receptor on leukocytes after incubation with aggregated IgA is related to cellular superoxide production and proteinuria(12). Our findings demonstrate increased malondialdehyde content in the renal parenchyma in rats with experimental IgA nephropathy compared with normal rats. The alteration in renal malondialdehyde content in the rats with IgA nephropathy was confirmed by an alternative method of assessing lipid peroxidation namely, conjugated diene content. These data suggest that there is excessive production of oxygen free radicals in the pathogenesis of kidney injury in experimental IgA nephropathy. Despite enhanced renal oxidant stress in this model of IgA nephropathy, dietary vitamin E supplementation was equally effective in lowering renal malondialdehyde content in experimental and control animals. The biologic capacity of vitamin E to act as a chain breaking agent and prevent the propagation of lipid peroxidative reactions is not specific to this renal disease state. However, even in the face of experimental evidence of a role of oxygen free radicals in the pathogenesis of renal disease, efficacy of antioxidant therapy must be proven. Our data indicate that rats with immunologically mediated IgA nephropathy manifest preservation of renal structure function when treated with the antioxidant, vitamin E. We did not separate glomeruli from tubules; however, because this disease affects primarily glomeruli early in its course, it is likely that the degree of oxidant injury would be even greater in isolated glomeruli.
Direct lipid peroxidation of cultured rat mesangial induced by high glucose is reversed by addition of vitamin E to the external media(22). The in vitro efficacy ofα-tocopherol as an antioxidant for mesangial cells is confirmed by ourin vivo studies of IgA nephropathy. We wish to emphasize that the test diet contained only a 3-fold higher vitamin E content than standard chow. However, ingestion of the special formulation resulted in a 4-5-fold rise in the mean plasma vitamin E concentration. The magnitude of this increment may be a determining factor in assessing the potential benefit of vitamin E treatment of kidney disease(23).
Protection against glomerular injury with a vitamin E-enriched diet has also been observed in chronic puromycin aminonucleoside nephropathy, a much more severe glomerulopathy(24). The degree of preservation of GFR and RPF achieved by vitamin E supplementation is comparable to the protection elicited by administration of a thromboxane receptor antagonist and/or a thromboxane synthesis inhibitor in experimental IgA nephropathy(13).
The association of increased renal lipid peroxidation and glomerular hypertrophy has been observed in other experimental kidney diseases such as chronic streptozocin-induced diabetes(25) and puromycin aminonucleoside nephropathy(24, 26). Oxidant stress may stimulate mesangial cell proliferation and extracellular matrix production, yielding glomerular hypertrophy. Reversal of glomerular enlargement by vitamin E occurred in the absence of increased kidney size. The protective effect of vitamin E in the face of improved GFR and RPF (only the difference in RBF was statistically significant), suggests that in the setting of this mild glomerulopathy, glomerular hypertrophy may be a more important factor in determining progressive loss of renal function(27, 28).
Intraglomerular activation of various cytokines, paracrine, and autocrine factors probably contributes to glomerular dysfunction in IgA nephropathy, and interference with the production of any of these mediators is likely to be beneficial in the kidney. For example, it has recently been shown that TGF-β1 gene expression in the glomeruli is enhanced in patients with IgA nephropathy(29). In the model of experimental IgA nephropathy presented here, increased renal gene expression of TGF-β1 was reversed by feeding the vitamin E-supplemented diet. This is consistent with previous studies documenting an important role for TGF-β1 in promoting intrarenal fibrosis and glomerulosclerosis in experimental kidney disease(30). The failure to document changes in interstitial fibrosis or glomerulosclerosis in these studies despite increased renal expression of TGF-β probably reflects the mild nature and relatively short duration of the immunologic insult to the kidney. We speculate that in this model of IgA nephropathy, oxidant stress increases the renal activity of TGF-β1 which, in turn, augments glomerular scarring. Feeding a vitamin E-enriched diet interrupts this process and protects against glomerular injury.
IgA nephropathy is a very common lesion in clinical nephrology. Although most patients with this disease do very well, nearly 25% will progress to end-stage renal disease over 20-25 y. There are no immunosuppressive or cytotoxic agents that have been demonstrated to safely and effectively reduce the morbidity of this glomerulopathy. A recent report by Donadio et al.(31) demonstrated that fish oil supplements retarded the rate of progression in patients with IgA nephropathy and persistent proteinuria; however, this benefit has not been universally confirmed(32). The availability of a safe and highly effective treatment such as dietary supplementation with antioxidants like vitamin E would represent a major advance in the care of patients with IgA nephropathy. Our data support consideration of a clinical trial to evaluate the effect of long term vitamin E administration on the course of IgA nephropathy.
Abbreviations
- BGG:
-
bovine γ-globulin
- BW:
-
body weight
- PAH:
-
p-aminohippuric acid
- RPF:
-
renal plasma flow
- TGF-β:
-
transforming growth factor-β;
- AU:
-
arbitrary units
REFERENCES
Emancipator SN, Gallo GR, Lamm ME 1985 IgA nephropathy: perspectives on pathogenesis and classification. Clin Nephrol 24: 161–179
Rodicio JL 1984 Idiopathic IgA nephropathy. Kidney Int 25: 717–729
Schena FP 1990 A retrospective analysis of the natural history of primary IgA nephropathy worldwide. Am J Med 89: 209–215
Wyatt RJ, Julian BA, Bhathena DB, Mitchell BL, Holland NH, Malluche HH 1984 IgA nephropathy: presentation, clinical course and prognosis in children and adults. Am J Kidney Dis 4: 192–200
D'Amico G, Imbasciati E, DiBelgioioso GB, Bertoli S, Fogazzi G, Ferrario F, Fellin G, Ragni A, Colasanti G, Minetti L, Ponticelli C 1985 Idiopathic IgA mesangial nephropathy: clinical and histological study of 374 patients. Medicine 64: 49–60
Alamartine E, Sabatier JC, Guerin C, Berliet JM, Berthoux F 1991 Prognostic factors in mesangial IgA glomerulonephritis: an extensive study with univariate and multivariate analysis. Am J Kidney Dis 18: 12–19
Clarkson AR, Woodroffe AJ, Bannister KM 1993 Therapy in IgA nephropathy. Contrib Nephrol 104: 189–197
Emancipator SN 1990 Immunoregulatory factors in the pathogenesis of IgA nephropathy. Kidney Int 38: 1216–1229
Van Es LA 1992 Pathogenesis of IgA nephropathy. Kidney Int 41: 1720–1729
Schrier RW, Harris DCH, Chan L, Shapiro JI, Caramelo C 1988 Tubular hypermetabolism as a factor in the progression of chronic renal failure. Am J Kidney Dis 12: 243–249
Chen A, Chen WP, Sheu LF, Lin CY 1994 Pathogenesis of IgA nephropathy: in vitro activation of human mesangial cells by IgA immune complexes. J Pathol 173: 119–126
Kashem A, Endoh M, Nomoto Y, Sakai H, Nakazawa H 1994 FcαR expression on polymorphonuclear leukocyte and superoxide generation in IgA nephropathy. Kidney Int 45: 868–875
Gesualdo L, Emancipator SN, Kesselheim C, Lamm ME 1992 Glomerular hemodynamics in a rat model of IgA nephropathy. Kidney Int 42: 106–114
Trachtman H, el Pizzo R, Futterweit S, Levine D, Rao PS, Valderrama E, Sturman JA 1992 Taurine attenuates renal disease in chronic puromycin aminonucleoside nephropathy. Am J Physiol 262:F117–F123
Chan W, Valerie KC, Chan JCM 1993 Expression of insulin-like growth factor-1 in uremic rats: growth hormone resistance and nutritional intake. Kidney Int 43: 790–795
Brandt RB, Gutheim WG, Dezzuti EP, Sica DA, Gehr TW, Hain JM 1991 Effect of multivitamins on plasma vitamin A and E levels in renal dialysis patients. VA J Sci 42: 100
Ohkawa H, Ohishi N, Yagi K 1979 Assay for lipid peroxides in animal tissues by thiobarbituric acid reaction. Anal Biochem 95: 351–358
Massey KD, Burton KP 1990 Free radical damage in neonatal rat cardiac myocyte cultures: effects of α-tocopherol, trolox, and phytol. Free Radic Biol Med 8: 449–458
Emancipator SN, Gallo GR, Razaboni R, Lamm ME 1983 Experimental cholestasis promotes the deposition of glomerular IgA immune complexes. Am J Pathol 113: 19–26
Imai H, Nakamoto Y, Asakura K, Miki K, Yasuda T, Miura AB 1985 Spontaneous glomerular IgA deposition in ddY mice: an animal model of IgA nephritis. Kidney Int 27: 756–761
Rifai A, Chen A, Imai H 1987 Complement activation in experimental IgA nephropathy: an antigen-mediated process. Kidney Int 32: 838–844
Trachtman H 1994 Vitamin E prevents glucose-induced lipid peroxidation and increased collagen production in cultured rat mesangial cells. Microvasc Res 47: 232–239
Hainonen OP, Albanes D 1994 The α-tocopherol,β-carotene cancer prevention study group: the effect of vitamin E andβ-carotene on the incidence of lung cancer in male smokers. N Engl J Med 330: 1029–1035
Trachtman H, Schwob N, Maesaka J, Valderrama E 1995 Dietary vitamin E supplementation ameliorates renal injury in chronic puromycin aminonucleoside nephropathy. J Am Soc Nephrol 5: 1811–1819
Trachtman H, Futterweit S, Maesaka J, Ma C, Valderrama E, Fuchs A, Tarectecan A, Rao PS, Sturman JA, Boles TH, Fu MX, Baynes JB 1995 Long term taurine administration ameliorates the severity of diabetic nephropathy. Am J Physiol 269:F429–F438
Trachtman H, Futterweit S, Schwob N, Maesaka J, Valderrama E 1993 Recombinant human growth hormone exacerbates chronic puromycin aminonucleoside nephropathy in rats. Kidney Int 44: 1281–1288
Yoshida Y, Fogo A, Ichikawa I 1989 Glomerular hemodynamic changes vs. hypertrophy in experimental glomerular sclerosis. Kidney Int 35: 654–660
Brenner BM 1985 Nephron adaptation to renal injury or ablation. Am J Physiol 249:F324–F337
Naka R, Suzki D, Miyazaki M, Yagame M, Endoh M, Nomoto Y, Sakai H 1993 TGF-β mRNA and tissue damage in glomeruli from patients with IgA nephropathy. J Am Soc Nephrol 4: 685A
Border WA, Noble NA 1994 Transforming growth factorβ in tissue fibrosis. N Engl J Med 331: 1286–1292
Donadio JV Jr, Bergstralh EJ, Offord KP, Spencer DC, Holley KE 1994 A controlled trial of fish oil in IgA nephropathy. N Engl J Med 331: 1194–1199
Pettersson EE, Rekola S, Berglund L, Sundqvist KG, Angelin B, Diczfalusy U, Bjorkhem I, Bergstrom J 1994 Treatment of IgA nephropathy with omega-3-polyunsaturated fatty acids: a prospective, double-blind, randomized study. Clin Nephrol 41: 183–189
Acknowledgements
The authors thank Antonio Tarectecan for his assistance in performing the renal immunofluorescence studies.
Author information
Authors and Affiliations
Additional information
Portions of this work were presented at the 27th Annual Meeting of the American Society of Nephrology, Orlando, FL, October 1994.
Rights and permissions
About this article
Cite this article
Trachtman, H., Chan, J., Chan, W. et al. Vitamin E Ameliorates Renal Injury in an Experimental Model of Immunoglobulin A Nephropathy. Pediatr Res 40, 620–626 (1996). https://doi.org/10.1203/00006450-199610000-00018
Received:
Accepted:
Issue Date:
DOI: https://doi.org/10.1203/00006450-199610000-00018
This article is cited by
-
Vitamin E in renal therapeutic regimens
Pediatric Nephrology (2006)