Abstract
The safety, tolerability, and efficacy of a 12-wk treatment with pravastatin, 5, 10, and 20 mg/d, was evaluated in 72 children with heterozygous familial hypercholesterolemia (FH) in a double-blind, randomized, and placebo-controlled study. The results show that pravastatin was well tolerated and that adverse events were mild and equally distributed among the three treatment groups. Plasma total and LDL cholesterol levels were significantly reduced in all pravastatin treatment groups, in comparison with the control group; -24.6% (-28.1 to 21.0) and -32.9% (-37.0 to -28.6), for mean change and 95% confidence interval, respectively. In four children plasma LDL cholesterol levels were reduced within normal limits for sex and age. HDL cholesterol increased in the pravastatin 20-mg group, +10.8% (+3.4 to +18.8), whereas plasma apo B100 and very LDL (VLDL) cholesterol levels were reduced within all pravastatin-treated groups -26.8% (-13.2 to -21.7) and-24.5% (-35.0 to -12.3). These data show that short-term pravastatin treatment of children with FH is safe and effective, although long-term dose titration studies with 3-hydroxy-3-methylglutaryl-CoA reductase inhibitors need to be performed, to reduce plasma LDL cholesterol levels below a predefined level. The results of these studies have to be awaited before new treatment strategies are to be considered in these children.
Similar content being viewed by others
Main
FH(1), an autosomal dominantly inherited defect in cholesterol clearance, affects approximately one out of 450 individuals in western countries(2). There is general agreement that adults with FH should receive aggressive diet and drug treatment to lower their substantially increased risk of cardiovascular morbidity and mortality(3).
The onset of coronary artery disease in FH patients can be as premature as the third decade of life, and early initiation of drug treatment in these patients seems warranted. The necessity and benefit of lowering cholesterol in children with FH, however, is debated, and furthermore, treatment may be associated with unwanted side effects. Growth and maturation of (pre)-pubertal children could be negatively affected by modifying cholesterol synthesis. Moreover, results of recent trials suggest that, when treatment is postponed until adulthood, progression of atherosclerotic lesions can still be influenced(4–6).
On the other hand, it is well documented that, within the cohort of FH patients, some exhibit rapid disease progression with clinical manifestations of atherosclerosis, whereas others will develop CVD much later. Probably, additional and largely unknown, either acquired or congenital, risk factors may explain this difference(7). Therefore, it seems likely that the effects of early initiation of cholesterol-lowering treatment in younger individuals will have to be evaluated one time or another.
At the present time, the recommended therapeutic regimen for children with FH is restricted to bile acid binding resins in conjunction with a lipid-lowering diet(8). Long-term studies, however, reported modest reductions of approximately 12% of plasma total cholesterol with this regimen(9, 10), only slightly more effective than diet alone(11, 12), and essentially insufficient to modify the process of vessel wall damage. Although HMG-CoA reductase inhibitors, the drugs of choice in the treatment of adults with FH, have proven to be safe and effective in large scale clinical studies(3, 13), only a few small observational studies, concerning the use of these drugs in children, have been reported(10, 14). Although in these studies children were treated for more than 1 y, neither of these investigations included control patients or were large enough to address safety.
In the present placebo-controlled study, we investigated the 3-mo safety, tolerability, and efficacy of pravastatin in 72 randomly selected children, aged 8 to 16 y, with heterozygous FH.
METHODS
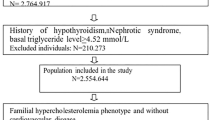
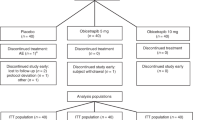
Study design. The aim of this double-blind, randomized, placebo-controlled study was to evaluate safety, tolerability, and efficacy of 12-wk pravastatin treatment in 72 children with FH. Children were stratified for age(15) into three groups of equal number;i.e. 8 to 10, 11 to 13, and 14 to 16 y. After a diet and placebo run-in period of 8 wk, patients were randomized to four treatment arms,i.e. daily pravastatin, 5, 10, or 20 mg, or placebo, and were seen monthly.
Prestudy diet was evaluated for a period of 5 d, using a computer questionnaire, and adjusted, if necessary, to comply with an intake of carbohydrate 50% energy, protein 20% energy, and fat 30%, with a unsaturated:saturated ratio of 2:1. The daily intake of cholesterol was less than 300 mg.
Written informed consent was obtained from one of the parents or guardians and from all children when they were 12 y or older. The protocol was approved by the Institutional Review Board.
Patients. Children with known heterozygous FH were eligible for the study. Heterozygous FH was defined as a plasma LDL cholesterol level above the 95th percentile for age and sex, during lipid-lowering diet. Moreover, hypercholesterolemia had to be present in siblings, parents, or grandparents, or clinical manifestations of premature atherosclerosis had to be present before the age of 50 y in first or second degree relatives. Children were excluded if they had undergone major surgery in the past 3 mo or when they used medication interfering with lipid metabolism (such as anticonvulsants, oral contraceptives, corticosteroids, fibric acid derivatives, or immunosuppressants). Furthermore, children with hepatic or renal dysfunction were not included in the study.
Safety and efficacy measurement. A physical examination was performed at entry and at the final visit. During the other visits adverse events and vital signs were recorded by physicians unaware of treatment allocation. At each visit, blood samples were drawn after an overnight fast. Laboratory safety parameters included routine hematology, biochemistry, and urinalysis. Also TSH, cortisol, and ACTH were measured before and after the treatment period. Plasma total and LDL cholesterol, triglycerides, HDL cholesterol, apo A1, apo B100, Lp(a), and VLDL cholesterol were measured to assess efficacy. Plasma LDL cholesterol was calculated using the Friedewald equation(16). Apo A1 and B100 were determined by an immuno-rate-nephelometric procedure using a polyclonal goat-anti-human antiserum and were calibrated on World Health Organization proposed international reference material(17). Lp(a) was determined by an electroimmunodiffusion procedure using a monospecific polyclonal goat antiserum and calibrated on immunostandard human serum(18). VLDL cholesterol was determined after separation by ultracentrifugation in a Cs-chloride solution, and cholesterol was quantified enzymatically in the supernatant(19). Treatment compliance was evaluated by tablet count.
Statistical analysis. Analyses of variance and covariance were used for between-group comparisons. Paired t tests were used to assess significance of changes from baseline within each treatment group. Baseline values as well as age were included as covariates in the analysis. For frequency data, Fisher's exact test was used. All results were analyzed on the basis of intention to treat.
RESULTS
Seventy-two children were randomized to the four treatment groups. Baseline characteristics were comparable with respect to sex, age, ethnicity, and lipoprotein profiles (Table 1). All patients completed the study according to protocol. Overall compliance with intake of study medication was excellent (93%) and comparable among the groups. Four children belonging to one family showed a poor compliance; they were equally distributed over the treatment groups.
Safety results. Pravastatin was well tolerated. Adverse events, whether or not considered to be related to therapy, were equally distributed among the four treatment groups (Table 2). One patient, treated with pravastatin 5 mg had a rash, which spontaneously disappeared after a few days, while drug treatment was continued. Five children, two in the placebo and three in the pravastatin 10-mg group, reported a single episode of headache during the active treatment period, of which none was considered to be serious. In the placebo group, one headache occurred during a period of rhinitis, and one appeared to be related to school examinations. Similar reasons were reported by the children in the pravastatin 10-mg group, who experienced headaches. All headaches resolved spontaneously after 1 to 3 d. The gastrointestinal complaints all resolved without a change in medication. Finally, laboratory safety measurements, including plasma TSH, ACTH, cortisol, creatine phosphokinase, and liver enzyme levels, did not show significant changes in any of the groups between the end of the treatment period and baseline (data are shown in Table 3).
Efficacy results. At week 12, both plasma total and LDL cholesterol levels were significantly reduced in all pravastatintreated groups (Fig. 1,A and B). The curves show that maximum effect was reached within 8 wk, regardless the dosage used. The plasma LDL cholesterol levels were not reduced below the 95th percentile for sex and age (Fig. 2), except for two children in the pravastatin 20-mg group and one child each in the 5- and 10-mg groups, respectively. Plasma HDL cholesterol and triglyceride levels did not change as compared from baseline, except for a mean HDL cholesterol level increase of 11% in the pravastatin 20-mg group (p < 0.01). Plasma VLDL cholesterol and apo B100 levels were reduced within all pravastatin-treated groups(p < 0.05 and p < 0.001; data shown for all lipid and lipoprotein parameters in Table 4). Plasma levels of apo A1 showed a trend toward improvement in the pravastatin 20-mg group. Lp(a) levels were not influenced by pravastatin treatment.
DISCUSSION
Our study demonstrates that 12 wk of pravastatin treatment in children with FH is well tolerated and does not affect routine biochemical parameters or hormonal status, as reflected by TSH, ACTH, or cortisol. The latter is in agreement with previous studies in adults(20, 21). As expected, plasma total and LDL cholesterol levels showed a significant reduction, which appeared to be dose-related. In the pravastatin 20-mg group, mean plasma LDL cholesterol decreased by 33%, whereas in the 5- and 10-mg groups plasma LDL cholesterol was reduced by 23%. A similar dose-related response was observed in the relative reduction of plasma total cholesterol.
It should be noted that, in only a few children, plasma LDL cholesterol levels did fall below the 95th percentile for age and sex, which could be considered a minimum level for slowing down the atherosclerotic process. In fact, there is suggestive evidence from studies in adults that arrest or regression of atherosclerosis is obtained only when plasma LDL cholesterol levels are reduced below 2.5 mmol/L(3, 10). Although the children in the present study were treated for a relatively short period of time, it can be assumed that the decrease observed would remain constant, especially because a convenient once daily regimen favors compliance.
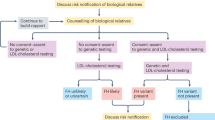
What would be the preferred strategy in children with FH? It is premature to suggest a general course of treatment in children with FH, because it is not yet known whether all subjects with FH need to be treated in childhood, to prevent premature CVD. There is indeed reason to believe that, among subjects with FH, specific high risk groups exist, with, for example very high cholesterol levels or an extensive family history of premature CVD,i.e. determinants of FH itself. Additional genetic risk factors for the development of CVD, such as hyperhomocysteinemia or high levels of Lp(a), might contribute to the high risk status of these subjects with FH(7). It will be necessary to identify these high risk subgroups at an early point in time and to demonstrate that these subjects have a more progressive atherosclerotic disease of their arteries and subsequently that plasma LDL cholesterol lowering to a predefined level results in the arrest or regression of atherosclerosis(22).
At present, the international recommended treatment for children with FH consists of a lipid-lowering diet in combination with bile acid-binding resins(8), which has been shown to be safe and effective. However, long-term experience with this regimen is very disappointing with respect to effective cholesterol lowering, due to a sharp decrease in drug intake compliance over time(23). Our study demonstrates that pravastatin, in an once daily dosage regimen, may be a useful agent in the treatment of high risk children with FH. Albeit, long-term safety and efficacy studies with HMG-CoA reductase inhibitors using dose titration, to reduce plasma LDL cholesterol levels below a predefined level, need to be performed. Furthermore, the role of combination therapy in these subjects should be assessed.
In conclusion, cholesterol-lowering treatment with pravastatin is safe, well tolerated, and effective in children with FH. However, before new treatment strategies in these children are to be considered, results of long-term studies have to be awaited.
Note: After acceptance of this manuscript we became aware of an independently performed study in which three statins (simva-, lova- and pravastatin) were compared in young rats(24). Clinical signs (myopathy, walking, body weight), plasma creatine kinase activity (as a measure of muscle damage), and histologic validation of muscle damage were used as parameters. It appeared that the lipophilic statins (simva- and lovastatin) caused a strong reduction in body weight, very high plasma creatine kinase activity, and myopathy, in a dose-dependent fashion. Simvastatin was most potent in this respect (15 mg/kg/d), whereas lovastatin produced these effects at higher doses (40-55 mg/kg/d). Pravastatin, a hydrophilic compound, did not produce any of these symptoms, except some loss in body weight. Even at extremely high doses (1000 mg/kg/d) no signs of a myopathy were observed. The conclusion is that young animals are more susceptible to adverse effects of simva- and lovastatin. These results and ours collectively suggest that for long-term safety studies in young children pravastatin may be the most suitable candidate.
Abbreviations
- CVD:
-
coronary vascular disease
- C.I.:
-
confidence interval
- FH:
-
familial hypercholesterolemia
- HMG-:
-
3-hydroxy-3-methylglutaryl-
- Lp(a):
-
lipoprotein (a)
- VLDL:
-
very LDL
- TSH:
-
thyroid stimulating hormone
References
Goldstein JL, Hobbs HH, Brown MS 1995 Familial hypercholesterolemia. In: Scriver CR, Beaudet AL, Sly WS, Valle D (eds) The Metabolic Basis of Inherited Disease, 7th Ed. McGraw-Hill, New York, pp 1981–2030.
Lansberg PJ, Van der Ree MA, Kastelein JJP, Van den Ende A, Wille C, Bakker S, Pannekoek WG, Wolsak FW, Aldenhuizen M, Ten Cate JW 1993 Prevalence and characteristics of major hereditary disorders of lipoprotein metabolism identified in general practice in Hoofddorp, the Netherlands. The molecular basis and treatment of familial hypercholesterolemia. Thesis, Joep Defesche and Peter Lansberg, Amsterdam, pp 199–222.
Illingworth DR 1993 How effective is drug therapy in heterozygous familial hypercholesterolemia. Am J Cardiol 72: 54D–58D.
Pitt B, Mancini GBJ, Ellis SG, Rosman HS, McGovern ME 1994 Pravastatin limitation of atherosclerosis in the coronary arteries (PLAC I). J Am Coll Cardiol 131a: 739–732.
Byington RP, Furberg CD, Crouse JR, Bond MG, Espeland MA 1993 PLAC-2: effects of pravastatin on progression of carotid atherosclerosis and clinical events. Eur Heart J 14: 11-iv
Watts GF, Lewis B, Brunt JNH, Lewis ES, Coltart LDR, Mann JL, Swan AV 1992 Effects on coronary artery disease of lipid-lowering diet, or diet plus cholestyramine, in the St. Thomas' Atherosclerosis Regression Study(STARS). Lancet 339: 563–569.
Ross R 1993 The pathogenesis of atherosclerosis: a perspective for the 1990s. Nature 362: 801–809.
National Cholesterol Education Program: Report of the Expert Panel on Blood Cholesterol Levels in Children and Adolescents 1992 Pediatrics 89( suppl): 525–584.
Glueck CJ, Mellies MJ, Dine M, Perry T, Laskarzewski P 1986 Safety and efficacy of long-term diet and diet plus bile acid binding resin cholesterol-lowering therapy in 73 children heterozygous for familial hypercholesterolemia. Pediatrics 78: 338–348.
Stein EA 1989 Treatment of familial hypercholesterolemia with drugs in children. Arteriosclerosis 9( Suppl. I): I145–I151.
Connor WE, Connor SL 1993 Importance of diet in the treatment of familial hypercholesterolemia. Am J Cardiol 72: 42D–53D.
Kwiterovich PO 1989 Pediatric implications of heterozygous familial hypercholesterolemia. Screening and dietary treatment. Arteriosclerosis 9: I111–I120.
Grundy SM 1988 HMG-CoA reductase inhibitors for treatment of hypercholesterolemia. N Engl J Med 319: 24–33.
Ducobu J, Brasseur D, Chaudron J-M, Deslypere JP, Harvengt C, Muls E, Thomson M 1992 Simvastatin use in children. Lancet 339: 1488
Pediatric clinical chemistry: reference (normal) values 1994 AACC Press, Washington DC
Friedewald WT, Levy RI, Fredrickson DS 1972 Estimation of the concentration of low-density lipoprotein cholesterol in plasma, without use of the preparative ultracentrifugation. Clin Chem 18: 499–502.
Marcovina S, Albers JJ, Dati F 1991 International federation of clinical chemistry standardization project for measurements of apolipoproteins A-I and B. Clin Chem 37: 1676–1682.
Molinaari E, Pichler P, Krempler F, Kostner G 1983 A rapid screening method for pathological lipoprotein (a) concentrations by counterimmunoelectrophoresis. Clin Chem 128: 373–378.
Kupke IR, Worz-Zeugner S 1986 Sequential microultracentrifugation of lipoproteins in 100 L of serum. J Lipid Res 27: 988–995.
Jay RH, Sturley RH, Stirling C, McGarrigle HHG, Katz M, Reckless JPD, Betteridge DJ 1991 Effects of pravastatin and cholestyramine on gonadal and adrenal steroid production in familial hypercholesterolaemia. Br J Clin Pharmacol 32: 417–422.
Purvis K, Tollefsrud A, Rui H, Haug E, Norseth E, Viksmoen L, Ose L, Lund H 1992 Short-term effects of treatment with simvastatin on testicular function in patients with heterozygous familial hypercholesterolaemia. Eur J Clin Pharmacol 42: 61–64.
Spengel FA, Kaess B, Keller C, Kroner KK, Schreiber M, Schuster H, Zollner N 1988 Atherosclerosis of the carotid arteries in young patients with familial hypercholesterolemia. Klin Wochenschr 66: 65–68.
West RJ, Lloyd JK, Leonard JV 1980 Long-term follow-up of children with familial hypercholesterolemia treated with cholestyramine. Lancet 2: 873–875.
Reijneveld JC, Koot RW, Bredman JJ, Joles JA, Bär PR 1996 Differential effects of HMG-CoA reductase inhibitors on the development of myopathy in young rats. Pediatr Res 39 ( June issue)
Acknowledgements
The authors thank Bristol-Myers Squibb Netherlands for financial support and coordination (Dr. I. Hoogendam and Dr. P. A. Leijten).
Author information
Authors and Affiliations
Rights and permissions
About this article
Cite this article
Knipscheer, H., Boelen, C., Kastelein, J. et al. Short-Term Efficacy and Safety of Pravastatin in 72 Children with Familial Hypercholesterolemia. Pediatr Res 39, 867–871 (1996). https://doi.org/10.1203/00006450-199605000-00021
Received:
Accepted:
Issue Date:
DOI: https://doi.org/10.1203/00006450-199605000-00021
This article is cited by
-
Prävention von Herz-Kreislauf-Erkrankungen im Kindes- und Jugendalter
Herz (2020)
-
Efficacy and safety of statin use in children and adolescents with familial hypercholesterolaemia: a systematic review and meta-analysis of randomized-controlled trials
Endocrine (2020)
-
Cholesterol screening and statin use in children: a literature review
Irish Journal of Medical Science (1971 -) (2019)
-
Risks and Benefits of Statin Use in Young People with Type 1 Diabetes
Current Diabetes Reports (2014)
-
Chapter 4: Pharmacological cholesterol-lowering treatment in children
Kidney International Supplements (2013)