Abstract
This study investigated the effect of acute systemic hypotension, induced by pericardial tamponade, on intestinal hemodynamics and oxygenation in 3- and 35-d-old swine. To delineate intrinsic versus systemic responses, the effects of tamponade were compared with those noted after isolated pressure reduction to an innervated in vivo gut loop, achieved by local arterial constriction. Younger subjects demonstrated 16 and 58% increases in vascular resistance during constriction and tamponade, respectively, whereas older subjects exhibited an increase in resistance (27%) only during tamponade. Intestinal oxygen uptake decreased ≈30% during both constriction and tamponade in the younger group, despite the greater effect of tamponade on gut perfusion. Older subjects exhibited no change in gut oxygenation during either perturbation. In a separate series of experiments, vasopressin, phenylephrine, and angiotensin II, each an element of the systemic pressor response, were infused into in vitro gut loops from 3- and 35-d-old swine. Vasopressin caused sustained vasoconstriction in both age groups; however, phenylephrine and angiotensin II caused greater sustained increases in intestinal vascular resistance in 3- than in 35-d-old intestine. We conclude that systemic hypotension compromises intestinal perfusion to a greater extent in younger subjects, although this effect is not associated with overwhelming tissue hypoxia. The pronounced rise in gut vascular resistance in 3-d-old intestine may reflect the additive effects of intrinsic and systemic vasoactive forces engaged during acute systemic hypotension.
Similar content being viewed by others
Main
Acute systemic hypotension should have two significant effects on intestinal hemodynamics. First, the fall in perfusion pressure, blood flow, and oxygen delivery to the intestine should activate local vascular effector systems within the intestinal vasculature. These systems, such as the metabolic(1, 2) and myogenic(3) mechanisms, are intrinsic to the gut and its attendant circulation and operate independently of central neurohumoral vascular control systems. These intrinsic mechanisms would be expected to induce intestinal vasodilation in response to cardiac output reduction in an effort to preserve intestinal oxygenation(1, 2) and restore the microvasculature environment within the gut(3, 4); stated otherwise, they are designed to protect the intestine in the face of systemic cardiovascular instability. Second, acute systemic hypotension should elicit a systemic pressor response which includes increased adrenergic tone and elevation of plasma renin, angiotensin, and vasopressin(1). This pressor response is designed to restore systemic cardiovascular homeostasis by enhancing preload, improving arterial blood pressure, and redirecting cardiac output; stated otherwise, it serves to protect the whole organism, even at the expense of regional perfusion(1). Each of the elements of the pressor response can increase intestinal vascular resistance, as vasoconstriction of the splanchnic circulations are an essential part of the pressor response, even in the newborn(5, 6).
The intrinsic vascular response of postnatal intestine to acute pressure reduction is age-dependent(7, 8). Denervated loops of small intestine from 3-d-old swine perfused in vitro by means of an extracorporeal reservoir system demonstrate vasoconstriction in response to pressure reduction. In contrast, gut loops from 35-d-old swine exhibit little or no change in vascular resistance under similar circumstances; thus, pressure reduction has a significantly greater impact on intestinal blood flow in younger subjects. These in vitro responses may not entirely duplicate the effect of acute hypotension on gut hemodynamics in vivo, inasmuch as the systemic pressor response which might accompany acute hypotension in vivo is eliminated under in vitro experimental conditions. Indeed, it might be predicted that acute arterial pressure reduction in vivo would have a significantly greater impact on gut hemodynamics in younger subjects as vasoconstriction mediated by the systemic pressor response would combine with that mediated by intrinsic vascular control mechanisms.
The principal goal of this investigation was to determine the effect of acute arterial pressure reduction on postnatal intestinal hemodynamics and oxygenation in vivo. To this end, the pericardial tamponade model of cardiac output reduction described by Bulkley et al.(9) was used to create acute systemic hypotension and elicit the systemic pressor response in 3- and 35-d-old swine. The same experimental subjects were also instrumented so that the arterial pressure delivered to a segment of bowel could be reduced without altering systemic hemodynamics; this arrangement facilitated comparison of the intrinsic and systemic components of the intestinal vascular response to pressure reduction. Finally, in a separate group of subjects, the effects of intra-arterial infusion of phenylephrine, angiotensin II and vasopressin on intestinal hemodynamics and oxygenation were compared between age groups. These agents were selected inasmuch as they represent the major elements of the systemic pressor response.
METHODS
Animal acquisition and handling. Swine were obtained from a local breeder the day before use. Subjects in the 3-d-old group had an age range of 2 to 4 d, whereas those in the 35-d-old group ranged from 30 to 38 d old. Animals were fed age-appropriate diets until 12 h before use. The experimental protocols were approved by the Institutional Animal Care and Use Committee (protocol no. 01093AR). Surgical procedures and subsequent study were performed under pentobarbital anesthesia (induction, 35 mg/kg intraperitoneally; maintenance, 5 mg/kg i.v. every 30 min thereafter). Euthanasia was carried out by i.v. injection of Uthol, 1 ml/kg.
In vivo gut loop preparation. Subjects were fasted for 12 h, anesthetized, intubated, and ventilated to maintain normal blood gas tensions. Vascular catheters were placed in the right carotid and jugular vein, and into a femoral artery-vein pair. An infusion of 0.9% saline in 5% dextrose was run into the femoral vein catheter during surgery and subsequent study to replace evaporative fluid loss (5 mL/kg/h). A segment of proximal ileum-distal jejunum approximately 25 cm long was isolated from the remainder of the gut and cleansed by luminal instillation of warm saline, followed by air. After heparinization (500 u/kg) the mesenteric vein draining the isolated segment was cannulated and this catheter was led to a venous reservoir. Blood from the venous reservoir was pumped back to the animal via the jugular vein catheter at a rate equal to venous outflow and the height of this reservoir was adjusted to keep pressure in the venous circuit at 0 mm Hg. A circuit was established between the femoral artery and the mesenteric artery perfusing the gut segment. Cannulation of the mesenteric artery was completed after careful dissection of the perivascular nerve bundle, so that minimal damage to these nerves occurred. The extracorporeal circuits and venous reservoir were primed with age-matched swine blood to assure preservation of euvolemia. The abdominal incision was covered with plastic wrap. The pericardium was exposed via a left thoracotomy. A narrow gauge soft plastic catheter was introduced into the pericardial cavity and fixed in place by pursestring suture; thereafter, the chest wound was closed and the lung reinflated. Temperature of the animal and gut loop were monitored continuously and maintained at 38°C by means of an overhead servo-controlled heating element.
In vitro gut loop preparation. Subjects were anesthetized, intubated, ventilated, and heparinized as described previously. A segment of proximal ileum-distal jejunum approximately 25 cm in length was isolated from the remainder of the gut. The artery-vein pair serving this segment were cannulated and attached to the extracorporeal perfusion circuit; thereafter, the gut segment was removed from the study subject and placed in a plexiglass chamber maintained at 38°C. Arterial perfusion was achieved by an extracorporeal circuit consisting of a collecting flask, arterial and venous reservoirs, and a membrane oxygenator (Scimed, 0.6 m2). Blood for this apparatus was obtained from a second animal, approximately 120 d old (30-40 kg). To this end, blood donor subjects were anesthetized, intubated and ventilated, and heparinized (500 U/kg); thereafter, approximately 1000 mL of whole blood were removed while simultaneously infusing swine plasma, obtained from other experiments, at a rate equal to blood withdrawal. This action was taken to delay initiation of a systemic pressor response in the donor subjects during blood removal as this circumstance might alter the humoral composition of withdrawn blood. The blood was filtered (40 μm mesh) and placed in the collecting flask, which in turn was placed in a water bath situated over a stirplate. Blood was continuously pumped from the collecting flask through a membrane oxygenator gassed with 21% O2-5% CO2-balance N2 at a rate sufficient to maintain normal blood gas tensions. A small volume of blood (≈20 mL/min) was continuously pumped from the collecting flask to the arterial reservoir. Flow from the arterial reservoir to the gut loop could be achieved in two ways: by pressurizing the reservoir (controlled-pressure perfusion), or by directing the arterial circuit through a Gilson Miniplus roller pump (controlled-flow perfusion). The venous effluent from the gut loop was collected in the venous reservoir and thereafter returned to the collecting flask for recirculation. During infusion of agonists venous blood could be diverted to a second reservoir so that agonist recirculation was avoided.
Measurement techniques. In both preparations gut blood flow was measured by a cannulating electromagnetic flowmeter (Gould, Glen Burnie, MD; Inc., inside diameter, 2.0 mm) placed within the mesenteric vein circuit. Zero flow was established in each study by distal occlusion and the probe was calibrated weekly with swine blood. Vascular pressures were measured by standard pressure transducers attached by T-tube to the arterial and venous circuits; in addition, systemic arterial pressure was monitored in thein vivo preparation by a pressure transducer placed in-line with the carotid artery catheter. Blood gas tensions and blood oxygen content were measured with a Corning 168 (Corning Inc., Corning, NY) gas analyzer and Lex-O2-Con, respectively.
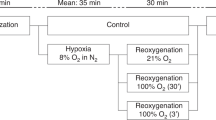
Cardiac tamponade protocol. After initial stabilization and acquisition of baseline data, a screw-clamp was placed on the femoral-mesenteric artery circuit and tightened until arterial pressure was reduced to approximately 70% of baseline. This action had no effect on systemic arterial pressure measured in the carotid artery inasmuch as the rate of flow through this circuit was small. Pressure reduction was sustained for 15 min, and then repeat measurements were taken. The clamp was removed, and the subject was left undisturbed for 30 min. After a second set of baseline data was obtained, cardiac tamponade was induced by infusing warm saline into the pericardial catheter. This infusion was continued until pressure noted in the femoral-mesenteric artery circuit was reduced to 70% of baseline,i.e. until it duplicated the level achieved previously by the clamp. The tamponade was maintained for 15 min, and then repeat measurements were taken. Reduction and maintenance of arterial pressure by induction of tamponade proved simple and reproducible.
Drug infusion protocol: controlled-flow studies. This protocol was carried out using the in vitro gut loop preparation. Arterial perfusion was initially established by increasing pressure in the arterial reservoir to an age-appropriate level, i.e. 70 mm Hg in 3-d-old intestine and 85 mm Hg in 35-d-old intestine. Perfusion was continued for 30 min or until blood flow achieved a steady-state level; thereafter, the arterial circuit was directed through a roller pump, and the pump rate was set to duplicate the existing gut flow rate. Controlled flow perfusion was incorporated into the experimental design to eliminate variation in concentration of the agonist in arterial blood, as would occur if flow increased or decreased during drug infusion. Each drug was administered separately to achieve the following concentrations (in whole blood): angiotensin 1.06 × 10-4 mg/mL (10-7 M); vasopressin 1.18× 10-6 mg/mL (10-9 M); phenylephrine 2.04 × 10-4 mg/mL (10-6 M). These doses were chosen as they are at or near the ED50 for these agents. Drugs were diluted in saline on the day of use and the vehicle infusion rate was 0.5 mL/min for each agent in every subject. During each drug infusion the venous effluent from the gut loop was diverted to a separate reservoir and thereafter discarded to eliminate drug recirculation. At least 30 min were allowed between each drug infusion, and in all instances hemodynamics were restored to pre-drug baseline before infusion of the next agonist. Vasopressin was always administered last inasmuch as the effect of this agent on vascular resistance was sustained for several hours after the infusion was stopped; administration of phenylephrine and angiotensin-II was randomized for each experiment.
Drug infusion protocol: controlled-pressure studies. This protocol was also carried out using the in vitro gut loop preparation. Sustained infusion of angiotensin often results in vasoconstriction, followed by vasodilation; this latter response appears to be mediated by angiotensin-induced stimulation of vasodilator prostaglandins(10, 11). To determine if a similar phenomenon occurs in postnatal intestine, intra-arterial infusion of angiotensin II was carried out in a separate group of study subjects under controlled pressure perfusion. Some subjects received indomethacin (5 mg/kg) delivered i.v.(jugular vein) 30 min before intra-arterial angiotensin infusion. To this end, indomethacin was initially dissolved in an equimolar solution of NaHCO3 and brought to final volume in saline; control subjects received the same volume of NaHCO3 + saline vehicle. This dose of indomethacin has been previously reported to effect nearly complete cyclooxygenase blockade in postnatal swine. Arterial perfusion was established at age-appropriate levels,i.e. 70 mm Hg in 3-d-old intestine and 85 mm Hg in 35-d-old intestine. Perfusion was continued for 30 min or until blood flow achieved a steady-state level. Baseline arterial and mesenteric vein blood samples were obtained. Angiotensin II was infused into the arterial circuit at a rate designed to provide an initial arterial concentration of 1.06 × 10-4 mg/mL (10-7 M); the drug infusion rate was not adjusted to compensate for subsequent changes in gut flow rate. A repeat set of blood samples were obtained when steady-state conditions were achieved.
Statistical methods. Data from the tamponade protocol were analyzed by means of a three-way ANOVA which incorporated age group (3- versus 35-d), condition (clamp versus tamponade) and time (baseline pressure versus reduced pressure) as main effects. Data from the controlled flow drug infusion study were analyzed by means of a three-way ANOVA for repetitive measures which incorporated group, agent (phenylephrineversus angiotensin II versus vasopressin) and time(baseline versus peak constriction versus steady-state) as main effects. To this end, steady-state was identified as preservation of pressure and flow ±5% during sustained drug infusion. Data from the controlled-pressure drug infusion study were also analyzed by three-way ANOVA for repetitive measures which incorporated group, condition (indomethacinversus vehicle), and time (baseline versus peak constriction versus steady-state) as main effects. In all analyses, post hoc Newman-Keuls tests were carried out if the F statistic for the ANOVA was p < 0.05; significance of the post hoc tests was accepted for p < 0.01.
RESULTS
Hemodynamic conditions noted within postnatal intestine were age-dependent, but not dependent on the mode of gut perfusion (Table 1). Conversion of in vitro gut perfusion from the controlled-pressure to controlled-flow mode caused a slight increase in vascular resistance in both age groups, a difference which did not attain statistical significance. Values for blood gas tension, blood oxygen content, and hematocrit were also similar in both age groups under all experimental conditions (Table 2).
Clamp constriction and pericardial tamponade caused equivalent reductions in mean perfusion pressure delivered to the gut, and also narrowed the pulse pressure to a similar extent. Clamp constriction had no effect on systemic arterial pressure (Table 3). The intestinal vascular response to hypotension was contingent on postnatal age as well as the means used to induce hypotension. Intestine from 3-d-old subjects demonstrated a 16% increase in vascular resistance during clamp constriction and a 58% increase during cardiac tamponade (Fig. 1). This difference occurred despite the fact that perfusion pressure delivered to 3-d-old gut loops were virtually identical during both experimental perturbations. Intestine from 35-d-old subjects demonstrated a modest increase in vascular resistance during tamponade, but not during clamp constriction.
The effect of acute reduction in perfusion pressure on intestinal vascular resistance in 3-d-old (open circles) and 35-d-old (closed circles) swine. Perfusion pressure was reduced by constricting a clamp leading to an innervated in vivo gut loop or by induction of cardiac tamponade; in both cases, the final pressure delivered to the gut loop was similar. Measurements were made before pressure reduction(baseline, B) and 15 min after pressure had been reduced to 70% of baseline (P). Data are shown as mean ± SEM, n = 7 for all observations. The data were analyzed by a three-way ANOVA and thereafter by post hoc tests; *p < 0.01 vs B;†p < 0.01 vs clamp.
The effect of hypotension on intestinal oxygenation was also age-dependent. Intestinal oxygen uptake was unaffected by hypotension in the 35-d-old group inasmuch as the (a-v)O2 across the gut rose in proportion to the fall in blood flow (Fig. 2). Younger subjects, however, demonstrated compromise of intestinal oxygenation during hypotension. Intestinal oxygen uptake decreased 21% during clamp constriction and 24% during tamponade, despite a modest increase in (a-v)O2 under both circumstances.
The effect of acute reduction in perfusion pressure on intestinal oxygen uptake in 3-d-old (open circles) and 35-d-old(closed circles) swine. Perfusion pressure was reduced by constricting a clamp leading to an innervated in vivo gut loop or by induction of cardiac tamponade; in both cases, the final pressure delivered to the gut loop was similar. Measurements were made before pressure reduction(baseline, B) and 15 min after pressure had been reduced to 70% of baseline (P). Data are shown as mean ± SEM, n = 7 for all observations. The data were analyzed by a three-way ANOVA and thereafter by post hoc tests, *p < 0.01 vs B.
Vasopressin, phenylephrine and angiotensin II each had significant effects on gut vascular resistance when infused to in vitro gut loops under controlled-flow conditions. Vasopressin increased intestinal vascular resistance 58% in 3-d-old and 53% in 35-d-old swine at its peak constrictive effect (Fig. 3). In both age groups this constrictive effect was sustained for the duration of drug infusion; in fact, resistance fell only very slowly toward baseline when the vasopressin infusion was discontinued. Vasopressin reduced the (a-v)O2 in both groups(Table 4). Phenylephrine increased intestinal vascular resistance 46% in 3-d-old and 57% in 35-d-old swine at its peak constrictive effect. However, in both groups resistance declined despite continued drug infusion. This reduction was greater in older subjects, so that when steady-state conditions were restored during drug infusion vascular resistance in 3-d-old intestine was not significantly different than that noted at peak constriction (Fig. 3). Phenylephrine also caused a modest reduction in (a-v)O2 in both age groups (Table 4). Angiotensin II increased intestinal vascular resistance 26% in 3-d-old and 39% in 35-d-old subjects at its peak constrictive effect (Fig. 3). Older subjects then demonstrated a profound fall in vascular resistance, so that when steady-state conditions were restored during drug infusion vascular resistance was 21% below pre-infusion baseline. In contrast, younger subjects displayed only a modest fall in vascular resistance: the steady-state value was not significantly different from the peak constrictive effect. Duplication of this experiment under controlled-pressure conditions yielded similar findings (Fig. 4). Of note, however, is that pretreatment with indomethacin attenuated the angiotensin-induced fall in vascular resistance in older subjects only. Indomethacin had no effect on the response of 3-d-old intestine to angiotensin II. Unlike vasopressin or phenylephrine, angiotensin II caused a modest rise in (a-v)O2(Table 4).
The effects of vasopressin (AVP), phenylephrine (PE), and angiotensin II (ANG-II) on vascular resistance in 3-d-old (open symbols) and 35-d-old(closed symbols) swine. Data were collected in denervated in vitro gut loops perfused from an arterial reservoir under controlled-flow conditions. Drugs were infused into the arterial circuit until steady-state hemodynamic conditions were restored. Data were collected before drug infusion(B), at the peak constrictive effect of the agent (M) and during after steady-state was restored during infusion (SS). Data are shown as mean ± SEM, n = 5 for all observations. Data were analyzed by three-way ANOVA and thereafter by post hoc tests;*p < 0.01 vs B, †p < 0.01vs M.
The effects of angiotensin II (ANG-II) alone(circles) or angiotensin II preceded by indomethacin(squares) on vascular resistance in 3-d-old (open symbols) and 35-d-old (closed symbols) swine. Data were collected in denervated in vitro gut loops perfused from an arterial reservoir under controlled-pressure conditions. Angiotensin II was infused into the arterial circuit until steady-state hemodynamic conditions were restored. Data were collected before drug infusion (B), at the peak constrictive effect of the agent (M) and during after steady-state was restored during drug infusion (SS). Data are shown as mean ± SEM,n = 5 for all observations. Data were analyzed by three-way ANOVA and thereafter by post hoc tests; *p < 0.01vs B, †p < 0.01 vs M, p < 0.01 vs angiotensin II alone.
DISCUSSION
The first new finding of this investigation was the age-dependent effect of systemic hypotension, induced by pericardial tamponade, on postnatal hemodynamics. Younger subjects demonstrated a 58% increase in gut vascular resistance during tamponade, whereas older subjects exhibited a more modest 27% rise. Two observations suggest that these different responses were consequent to intrinsic and systemic vascular control systems. First, clamp constriction resulted in an increase in gut vascular resistance in younger, but not in older subjects, indicating that the intrinsic vascular response to acute hypotension was age-dependent. This observation is consistent with previous reports from this laboratory; thus, in vitro gut loops from 3-d-old swine respond to perfusion pressure reduction with significant vasoconstriction, whereas gut loops from older subjects demonstrate a modest degree of vasodilation(8). The mechanism responsible for vasoconstriction in younger intestine remains an enigma. Clearly, this response is not mediated by intrinsic metabolic(1) or myogenic(3) mechanisms, inasmuch as these effector systems should cause vasodilation in response to acute hypotension. A very modest degree of vasoconstriction might be anticipated on the basis of passive elastic recoil of the vessel wall in response to reduced intravascular pressure(1). However, the degree of constriction noted in younger intestine suggests the presence of an active constrictor mechanism, not simply passive recoil. One candidate for this role might be endothelin, a potent constrictor peptide produced by the vascular endothelium in response to a variety of perturbations(12). Although entirely speculative at this point, endothelin seems a reasonable choice for two reasons: first, it is produced within the gut circulation (i.e. it is an intrinsic effector system), and second, endothelial production of this peptide is enhanced in response to hypotension or hypoxia(13). Clamp constriction had no significant effect on vascular resistance in older subjects. This lack of responsiveness may indicate that the magnitude of the pressure perturbation was insufficient to engage the metabolic(1) or myogenic(3) mechanisms which govern intrinsic vascular reactivity. Local reduction of gut perfusion pressure had no effect on intestinal oxygenation in older subjects, a circumstance necessary to elicit metabolic vasodilation(1); furthermore, the myogenic range of most blood vessels is extremely narrow for step reductions in pressure, in contrast to step-increases in pressure(14).
Second, the response of postnatal intestine to intra-arterial infusion of constrictor agents known to participate in the systemic pressor response was age-dependent. Angiotensin II caused a sustained increase in gut vascular resistance in 3-d-old but not in 35-d-old intestine. Older subjects demonstrated a secondary fall in vascular resistance which was significantly attenuated by pretreatment with indomethacin. Thus, it is most likely that angiotensin II stimulates production of dilator prostaglandins in older intestine, as has been previously described in other circulation(10, 11), so that the steady-state effect of this peptide is actually vasodilation. This finding is in sharp contrast to that of Bailey et al.(15) who reported sustained vasoconstriction during angiotensin II infusion in swine. However, this work was conducted in adolescent swine, the drug was given systemically and was preceded by rapid withdrawal of 10% of the subjects blood volume; as such, these data are not directly comparable to those reported here. The secondary vasodilation did not occur in younger subjects; thus, intestinal vascular resistance remained elevated during angiotensin II infusion in 3-d-old subjects and indomethacin had no effect on this response. If the systemic pressor response elicited by pericardial tamponade included activation of the reninangiotensin system, then the more pronounced vasoconstriction noted in younger subjects could have been mediated, in part, by angiotensin II. Intra-arterial phenylephrine also caused a greater sustained increase in gut vascular resistance in 3-d-old than in 35-d-old subjects. This age-dependent response seems inconsistent with earlier work from our laboratory, which demonstrated that sustained electrical stimulation of periarterial nerves surrounding the mesenteric artery led to similar hemodynamic responses in 3- and 35-d-old swine intestine(16). However, phenylephrine is a pure α1-agonist, whereas generalized stimulation of the mesenteric nerve likely caused release of several different neurotransmitters.
The second new finding of this investigation was the effect of cardiac tamponade on oxygenation in 3-d-old intestine. Thus, the reductions in tissue oxygen uptake noted during tamponade and clamp constriction were similar, despite the substantially greater reduction of gut blood flow noted during tamponade. In part, this effect might reflect passive adjustments in oxygen transport made at the cellular level. If all else is held constant, blood flow reduction will compromise capillary Po2. This effect would compromise the capillary-to-cell Po2 gradient which drives the diffusive flux of oxygen, and so impair tissue oxygenation(17). However, cell Po2 generally rests at a level well above that necessary to achieve mitochondrial respiration(18). Reduction in capillary Po2 can thus be countered by a fall in cell Po2, preserving the diffusion gradient without compromising cell function(17). These changes represent an intrinsic cellular buffer against hypoxia and do not require active vasoregulation to occur.
The limited effect of tamponade on newborn gut oxygenation might also be explained by a selective effect of angiotensin II within the gut microvasculature. It is generally accepted that gut oxygen transport is regulated at two key sites within the microvasculature: resistance vessels and precapillary sphincters(2, 19). Resistance vessels govern the delivery of blood, and thus oxygen into the microvasculature; this action regulates capillary Po2, the driving force for oxygen diffusion from capillary-to-cell. Precapillary sphincters dictate perfusion of individual capillaries. This action alters the perfused capillary density, which in turn determines capillary surface area available for oxygen diffusion and capillary-cell distance. Independent regulation of these microvascular elements can occur; thus, an agent might cause vasoconstriction but have little or no effect on capillary surface area(19–21). In this context, it is interesting to note that infusion of exogenous angiotensin II caused sustained elevation in gut vascular resistance in 3-d-old intestine, but also increased(a-v)O2. It is thus possible that angiotensin II permits newborn intestine to participate in the systemic pressor response to cardiac output reduction without further compromise of intestinal oxygenation. Such an arrangement makes teleologic sense as it facilitates preservation of both the organism and its intestine during circulatory crisis.
In 1969 Lloyd(22) postulated that selective intestinal ischemia occurred during systemic cardiovascular compromise and that this event led to tissue hypoxia, and eventual tissue necrosis. This notion, later termed the diving reflex theory, has remained a mainstay in the putative pathogenic mechanisms of necrotizing enterocolitis. Was Lloyd correct? Clearly, acute reduction of cardiac output has a substantial impact on intestinal perfusion, especially in the newborn. However, the effect of this flow reduction on tissue oxygenation is less overwhelming: flow reduction in excess of 50% during pericardial tamponade was associated with a more modest 24% fall in tissue oxygen uptake, possibly because this pressor response is accomplished selectively, without significant impairment of gut oxygen transport processes. It remains, however, that simultaneous impairment of cardiac output and arterial Po2, which was the circumstance described by Lloyd, would have a more pronounced effect on gut oxygenation.
Abbreviations
- ANOVA:
-
analysis of variance
- (a-v)O2:
-
arteriovenous O2 content difference
References
Granger HJ, Shepherd AP 1979 Dynamics and control of the microcirculation. Adv Biomed Eng 7: 1–62
Granger DN, Granger HJ 1983 Systems analysis of intestinal hemodynamics and oxygenation. Am J Physiol 245:G786–G796
Meninger GA, Davis MJ 1992 Cellular mechanisms involved in the vascular myogenic response. Am J Physiol 263:H647–H659
Davis MJ 1988 Microvascular control of capillary pressure during increases in local arterial and venous pressure. Am J Physiol 254:H722–H784
Buckley NM, Brazeau P, Frasier ID, Gootman PM 1985 Circulatory effects of splanchnic nerve stimulation in developing swine. Am J Physiol 248:H69–H74
Buckley NM, Gootman Pm, Gootman N, Reddy GD, Weaver LC, Crane LA 1976 Age dependent cardiovascular effects of afferent stimulation in neonatal pigs. Biol Neonate 30: 269–279
Nowicki PT, Miller CE, Edwards RC 1991 Effects of hypoxia and ischemia on autoregulation in postnatal intestine. Am J Physiol 261:G152–G157
Nowicki PT, Miller CE 1993 Regulation of capillary exchange capacity in postnatal swine intestine. Am J Physiol 265:G1090–G1097
Bulkley GB, Kvietys PR, Perry MA, Granger DN 1983 Effects of cardiac tamponade on colonic hemodynamics and oxygen uptake. Am J Physiol 244:G604–G612
Fleming JT, Joshua IG 1984 Mechanism of the biphasic arteriolar response to angiotensin II. Am J Physiol 247:H88–H94
Toda N, Ayaziki K, Okmura T 1990 Modifications by endogenous prostaglandins of Angiotensin II induced contractions in dog and monkey cerebral and mesenteric arteries. J Pharmacol Exp Ther 252: 374–379
Tabuchi Y, Nakamaru M, Rakugi H, Nagano M, Ogihara T 1989 Endothelin enhances adrenergic vasoconstriction in perfused rat mesenteric arteries. Biochem Biophys Res Commun 159: 1304–1307
Kourembanas S, Marsden P, McQuillan L, Faller D 1991 Hypoxia induces endothelin gene expression and secretion in cultured human endothelium. J Clin Invest 88: 1054–1057
Osol G, Halpern W 1985 Myogenic properties of cerebral blood vessels from normotensive and hypertensive rats. Am J Physiol 249:H914–H921
Bailey RW, Gulkley GB, Hamilton SR, Morris JB, Haglund UH 1987 Protection of the small intestine from nonocclusive mesenteric ischemia due to cardiogenic shock. Am J Surg 153: 108–115
Nowicki PT, Miller CE, Hayes JR 1991 Effect of sustained mesenteric nerve stimulation on intestinal oxygenation in developing swine. Am J Physiol 260:G333–G339
Granger HJ, Nyhof RA 1982 Dynamics of intestinal oxygenation: interactions between oxygen supply and uptake. Am J Physiol 243:G91–G96
Bohlen HG 1980 Intestinal tissue pO2 and microvascular responses during glucose exposure. Am J Physiol 238:H164–H171
Kvietys PR, Perry MA, Granger DN 1983 Intestinal capillary exchange capacity and oxygen delivery-to-demand ratio. Am J Physiol 245:G635–G640
Granger DN, Kvietys PR, Perry MA 1982 Role of exchange vessels in the regulation of intestinal oxygenation. Am J Physiol 242:G570–G574
Kvietys PR, Granger DN 1982 Relation between intestinal blood flow and oxygen uptake. Am J Physiol 242:G202–G208
Lloyd JR 1969 The etiology of gastrointestinal perforations in the newborn. J Pediatr Surg 4: 77–84
Acknowledgements
The authors thank Mary Smith for secretarial support in preparation of the manuscript.
Author information
Authors and Affiliations
Additional information
Supported by award HD25256 from the National Institute of Child Health and Human Development.
Rights and permissions
About this article
Cite this article
Nowicki, P., Miller, C. The Effects of Systemic Hypotension on Postnatal Intestinal Hemodynamics and Oxygenation. Pediatr Res 39, 105–111 (1996). https://doi.org/10.1203/00006450-199601000-00015
Received:
Accepted:
Issue Date:
DOI: https://doi.org/10.1203/00006450-199601000-00015