Key Points
-
The ability of modern multiparametric MRI to detect clinically significant prostate cancer has provided clinicians with relevant targets to be sampled and ablated using novel image-guided medical devices
-
Compared with the standardized pathways for evaluation of pharmaceutical agents, medical devices follow a less structured pathway to approval, and many key differences exist between Europe and the USA
-
European residents benefit from earlier adoption of new technologies; however, European device regulatory pathways have been criticised for allowing new devices to be used on patients without robust evaluation
-
By contrast, the regulatory pathway in the USA is more rigid, and the manner in which 'grandfathering' of similar devices can occur seems too heavily weighted against the introduction of novel medical devices
-
In this article, we discuss these issues and offer some perspective on the potentially safe, effective and compliant evaluation of novel image-guided devices for use in patients with prostate cancer
Abstract
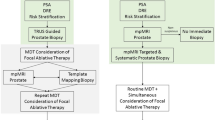
Findings of research using modern multiparametric MRI have provided clinicians with reliable targets for guiding prostate biopsy sampling and directing targeted therapy, often termed focal therapy, to specific areas of the prostate. This emerging shift in treatment strategy from a whole-gland approach to a lesion-specific or region-specific approach requires novel medical devices. The rules regulating the approval and clinical use of such new devices often differ between the USA and Europe, and these differences can affect the treatments that patients receive. Current regulatory pathways for approval of various image-guided biopsy and focal therapy devices intended to be used in patients with prostate cancer are discussed in detail. Finally, we offer some perspective on the current status of research in the field, and propose a potential roadmap towards the establishment of timely, safe and standardized criteria for optimal evaluation of novel image-guided devices for treatment of patients with localized prostate cancer.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$209.00 per year
only $17.42 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout

Similar content being viewed by others
References
Loeb, S. et al. Overdiagnosis and overtreatment of prostate cancer. Eur. Urol. 65, 1046–1055 (2014).
Shaw, G. L. et al. Identification of pathologically insignificant prostate cancer is not accurate in unscreened men. Br. J. Cancer 110, 2405–2411 (2014).
Lecornet, E. et al. The accuracy of different biopsy strategies for the detection of clinically important prostate cancer: a computer simulation. J. Urol. 188, 974–980 (2012).
Barentsz, J. O. et al. ESUR prostate MR guidelines 2012. Eur. Radiol. 22, 746–757 (2012).
Moore, C. M. et al. Image-guided prostate biopsy using magnetic resonance imaging-derived targets: a systematic review. Eur. Urol. 63, 125–140 (2013).
Valerio, M. et al. Detection of clinically significant prostate cancer using magnetic resonance imaging-ultrasound fusion targeted biopsy: a systematic review. Eur. Urol. 68, 8–19 (2014).
Logan, J. K. et al. Current status of magnetic resonance imaging (MRI) and ultrasonography fusion software platforms for guidance of prostate biopsies. BJU Int. 114, 641–652 (2014).
Sonn, G. A., Margolis, D. J. & Marks, L. S. Target detection: magnetic resonance imaging-ultrasound fusion-guided prostate biopsy. Urol. Oncol. 32, 903–911 (2014).
Eggener, S. et al. Focal therapy for prostate cancer: possibilities and limitations. Eur. Urol. 58, 57–64 (2010).
Valerio, M. et al. The role of focal therapy in the management of localised prostate cancer: a systematic review. Eur. Urol. 66, 732–751 (2014).
Wilt, T. J. et al. Radical prostatectomy versus observation for localized prostate cancer. N. Engl. J. Med. 367, 203–213 (2012).
Resnick, M. J. et al. Long-term functional outcomes after treatment for localized prostate cancer. N. Engl. J. Med. 368, 436–445 (2013).
Ahmed, H. U., Arya, M., Freeman, A. & Emberton, M. Do low-grade and low-volume prostate cancers bear the hallmarks of malignancy? Lancet Oncol. 13, e509–e517 (2012).
Eggener, S. E. et al. Predicting 15-year prostate cancer specific mortality after radical prostatectomy. J. Urol. 185, 869–875 (2011).
Ross, H. M. et al. Do adenocarcinomas of the prostate with Gleason score (GS) ≤6 have the potential to metastasize to lymph nodes? Am. J. Surg. Pathol. 36, 1346–1352 (2012).
Rud, E. et al. Detection of the index tumor and tumor volume in prostate cancer using T2-weighted and diffusion-weighted MRI alone. BJU Int. 114, E32–E42 (2014).
Arumainayagam, N. et al. Multiparametric MR imaging for detection of clinically significant prostate cancer: a validation cohort study with transperineal template prostate mapping as the reference standard. Radiology 268, 761–769 (2013).
Thompson, J. E. et al. Multiparametric magnetic resonance imaging guided diagnostic biopsy detects significant prostate cancer and could reduce unnecessary biopsies and over detection: a prospective study. J. Urol. 192, 67–74 (2014).
Kramer, D. B., Xu, S. & Kesselheim, A. S. Regulation of medical devices in the United States and European Union. N. Engl. J. Med. 366, 848–855 (2012).
Jugo, R. The FDA PMA versus the EU CE mark filing and approval experience: an empirical and descritive analysis. JMDR 18, 18–30 (2008).
Kaplan, A. V. et al. Medical device development: from prototype to regulatory approval. Circulation 109, 3068–3072 (2004).
Directive 98/79/EC of the European Parliament and of the Council of 27 October 1998 on in vitro diagnostic medical devices. OJ 41, L331 (1998).
Basu, S. & Hassenplug, J. C. Patient access to medical devices — a comparison of U.S. and European review processes. N. Engl. J. Med. 367, 485–488 (2012).
U.S. Department of Health and Human services. Food and drugs. U.S. Food and Drug Administration [online], (2015).
Jarow, J. P. et al. Drug and device development for localized prostate cancer: report of a Food and Drug Administration/American Urological Association public workshop. Urology 83, 975–979 (2014).
Valerio, M. et al. Re: Jarow et al.: drug and device development for localized prostate cancer: report of a Food and Drug Administration/American Urological Association public workshop (Urology 2014;83: 975-979). Urology 84, 732–733 (2014).
Marks, L., Young, S. & Natarajan, S. MRI-ultrasound fusion for guidance of targeted prostate biopsy. Curr. Opin. Urol. 23, 43–50 (2013).
Logan, J. K. et al. Current status of MRI and ultrasound fusion software platforms for guidance of prostate biopsies. BJU Int. 114, 641–652 (2014).
Siddiqui, M. M. et al. Comparison of MR/ultrasound fusion-guided biopsy with ultrasound-guided biopsy for the diagnosis of prostate cancer. JAMA 313, 390–397 (2015).
Puech, P. et al. Prostate cancer diagnosis: multiparametric MR-targeted biopsy with cognitive and transrectal US-MR fusion guidance versus systematic biopsy — prospective multicenter study. Radiology 268, 461–469 (2013).
Wysock, J. S. et al. A prospective, blinded comparison of magnetic resonance (MR) imaging-ultrasound fusion and visual estimation in the performance of MR-targeted prostate biopsy: the PROFUS trial. Eur. Urol. 66, 343–351 (2014).
Valerio, M. et al. Visually directed versus software-based targeted biopsy compared to transperineal template mapping biopsy in the detection of clinically significant prostate cancer. Urol. Oncol. 33, 424 (2015).
Jordan, W. P. Jr, Walker, D., Miller, G. H. Jr & Drylie, D. M. Cryotherapy of benign and neoplastic tumors of the prostate. Surg. Gynecol. Obstet. 125, 1265–1268 (1967).
Lau, B. et al. Technological aspects of delivering cryotherapy for prostate cancer. Expert Rev. Med. Devices 12, 183–190 (2015).
Ward, J. F. & Jones, J. S. Focal cryotherapy for localized prostate cancer: a report from the national cryo on-line database (COLD) registry. BJU Int. 109, 1648–1654 (2012).
Al-Qaisieh, B. et al. Dosimetry modeling for focal low-dose-rate prostate brachytherapy. Int. J. Radiat. Oncol. Biol. Phys. 92, 787–793 (2015).
Marshall, D. T. Options and recent advances in permanent brachytherapy for prostate cancer. Can. J. Urol. 14, S28–S31 (2007).
Ahmed, H. U. et al. Focal therapy for localized prostate cancer: a Phase I/II trial. J. Urol. 185, 1246–1254 (2011).
Ahmed, H. U. et al. Focal therapy for localised unifocal and multifocal prostate cancer: a prospective development study. Lancet Oncol. 13, 622–632 (2012).
Dickinson, L. et al. A multi-centre prospective development study evaluating focal therapy using high intensity focused ultrasound for localised prostate cancer: the INDEX study. Contemp. Clin. Trials 36, 68–80 (2013).
The European Association of Urology. Guidelines on prostate cancer [online], (2015).
US Department of Health and Human services. U.S. Food and Drug Administration [online], (2015).
US Department of Health and Human services. U.S. Food and Drug Administration [online], (2014).
Nguyen, P. L., D'Amico, A. V., Lee, A. K. & Suh, W. W. Patient selection, cancer control, and complications after salvage local therapy for postradiation prostate-specific antigen failure: a systematic review of the literature. Cancer 110, 1417–1428 (2007).
Moore, C. M. et al. Photodynamic therapy using meso tetra hydroxy phenyl chlorin (mTHPC) in early prostate cancer. Lasers Surg. Med. 38, 356–363 (2006).
Azzouzi, A. R. et al. TOOKAD(®) soluble vascular-targeted photodynamic (VTP) therapy: determination of optimal treatment conditions and assessment of effects in patients with localised prostate cancer. BJU Int. 112, 766–774 (2013).
Moore, C. M. et al. Determination of optimal drug dose and light dose index to achieve minimally invasive focal ablation of localized prostate cancer using WST11-vascular targeted photodynamic (VTP) therapy. BJU Int. 116, 888–896 (2014).
US National Library of Medicine. Efficacy and safety study of TOOKAD® soluble for localised prostate cancer compared to active surveillance. (PCM301). ClinicalTrials.gov [online], (2015).
Eikermann, M. et al. Commentary: Europe needs a central, transparent, and evidence based regulation process for devices. BMJ 346, f2771 (2013).
Curfman, G. D. & Redberg, R. F. Medical devices — balancing regulation and innovation. N. Engl. J. Med. 365, 975–977 (2011).
Giannarini, G., Gandaglia, G., Montorsi, F. & Briganti, A. Will focal therapy remain only an attractive illusion for the primary treatment of prostate cancer? J. Clin. Oncol. 32, 1299–1301 (2014).
van den Bos, W. et al. Focal therapy in prostate cancer: international multidisciplinary consensus on trial design. Eur. Urol. 65, 1078–1083 (2014).
Ahmed, H. U. et al. Can we deliver randomized trials of focal therapy in prostate cancer? Nat. Rev. Clin. Oncol. 11, 482–491 (2014).
Craig, P. et al. Developing and evaluating complex interventions: the new Medical Research Council guidance. BMJ 337, a1655 (2008).
Acknowledgements
M.V. gratefully acknowledges financial support from the SICPA foundation. M.E. and H.U.A. gratefully acknowledge financial support from the Medical Research Council (UK), the Pelican Cancer Foundation charity, Prostate Cancer UK, National Institute of Health Research-Health Technology Assessment and i4i programmes, St Peters Trust charity, Prostate Cancer Foundation, the Wellcome Trust and the US National Institute of Health-National Cancer Institute. M.E. also receives funding in part from the UK National Institute of Health Research UCLH/UCL Comprehensive Biomedical Research Centre. S.E.E. gratefully acknowledges funding from the US Department of Defense and National Cancer Institute. The authors would like to thank Mr Mark Duval and Mr Sew-Wah Tay for their comments on a previous draft of this manuscript.
Author information
Authors and Affiliations
Contributions
M.V. and H.U.A. researched data for this article. All authors made a substantial contribution to discussions of content, writing the manuscript and reviewing and/or editing of the manuscript before submission.
Corresponding author
Ethics declarations
Competing interests
M.E. and H.U.A. have received funding for clinical trials from Advanced Medical Diagnostics, GSK, Hitachi, Immodulon, Sonacare, Sophiris Biocorp and Trod Medical and have previously acted as consultants for Oncura/GE Healthcare and Steba Biotech. M.E. is a consultant of Sonacare and Steba Biotech, has share options in Nuada Medical and is a director on the board of this company. S.E.E. has received research support from Myriad and is a consultant of Myriad, NxThera and Profound Medical. M.V. declares no competing interests.
PowerPoint slides
Rights and permissions
About this article
Cite this article
Valerio, M., Emberton, M., Eggener, S. et al. The challenging landscape of medical device approval in localized prostate cancer. Nat Rev Urol 13, 91–98 (2016). https://doi.org/10.1038/nrurol.2015.289
Published:
Issue Date:
DOI: https://doi.org/10.1038/nrurol.2015.289