Abstract
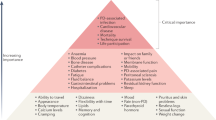
Long-term peritoneal dialysis can lead to morphological and functional changes in the peritoneum. Although the range of morphological alterations is known for the peritoneal dialysis population as a whole, these changes will not occur in every patient in the same sequence and to the same extent. Longitudinal studies are therefore required to help identify which patients might develop the changes. Although longitudinal studies using peritoneal biopsies are not possible, analyses of peritoneal effluent biomarkers that represent morphological alterations could provide insight. Longitudinal studies on peritoneal transport have been performed, but follow-up has often been too short and an insufficient number of parameters have been investigated. This Review will firstly describe peritoneal morphology and structure and will then focus on peritoneal effluent biomarkers and their changes over time. Net ultrafiltration will also be discussed together with the transport of small solutes. Data on the peritoneal transport of serum proteins show that serum protein levels do not increase to the same extent as levels of small solutes with long-term peritoneal dialysis. Early alterations in peritoneal transport must be distinguished from alterations that only develop with long-term peritoneal dialysis. Early alterations are related to vasoactive mediators, whereas later alterations are related to neoangiogenesis and fibrosis. Modern peritoneal dialysis should focus on the early detection of long-term membrane alterations by biomarkers—such as cancer antigen 125, interleukin-6 and plasminogen activator inhibitor 1—and the improved assessment of peritoneal transport.
Key Points
-
Studies have provided information regarding peritoneal morphological changes occurring with long-term peritoneal dialysis on a population scale, but this information cannot be used to identify changes occurring in individual patients
-
Longitudinal studies—investigating peritoneal effluent biomarkers and peritoneal fluid and solute transport—are required to investigate the development of alterations in individual patients
-
Promising biomarkers include cancer antigen 125, interleukin-6 and plasminogen activator inhibitor 1
-
Early ultrafiltration failure is often reversible and is usually associated with fast transport rates of low molecular weight solutes, which result in a rapid disappearance of the osmotic gradient
-
Long-term ultrafiltration failure develops over time and is often characterized by impaired osmotic conductance to glucose and reduced free water transport; in the absence of residual urine production, it can easily lead to overhydration
-
Peritoneal clearances of serum proteins increase less with peritoneal dialysis duration than do clearances of small solutes
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$209.00 per year
only $17.42 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout
Similar content being viewed by others
References
Fenton, S. S. et al. Hemodialysis versus peritoneal dialysis: a comparison of adjusted mortality rates. Am. J. Kidney Dis. 30, 334–342 (1997).
Liem, Y. S., Wong, J. B., Hunink, M. G., de Charro, F. T. & Winkelmayer, W. C. Comparison of hemodialysis and peritoneal dialysis survival in The Netherlands. Kidney Int. 71, 153–158 (2007).
Rodrigues, A. S. et al. Long-term peritoneal dialysis experience on Portugal. Int. J. Artif. Organs. 29, 1109–1116 (2006).
Kolesnyk, I., Dekker, F. W., Boeschoten, E. W. & Krediet, R. T. Time-dependent reasons for PD technique failure and mortality. Perit. Dial. Int. 30, 170–177 (2010).
Flessner, M. F. et al. Peritoneal inflammation after twenty-week exposure to dialysis solution: effect of solution versus catheter-foreign body reaction. Perit. Dial. Int. 30, 284–293 (2010).
Flessner, M. F., Li, X., Potter, R. & He, Z. Foreign-body response to sterile catheters is variable over 20 weeks. Adv. Perit. Dial. 26, 101–104 (2010).
Zareie, M. et al. Immunopathological changes in a uraemic rat model for peritoneal dialysis. Nephrol. Dial. Transplant. 20, 1350–1361 (2005).
Combet, S. et al. Chronic uremia induces permeability changes, increased nitric oxide synthase expression, and structural modifications in the peritoneum. J. Am. Soc. Nephrol. 12, 2146–2157 (2001).
Vrtovsnik, F. et al. Induction of chronic kidney failure in a long-term peritoneal exposure model in the rat: effects on functional and structural peritoneal alterations. Perit. Dial. Int. 30, 558–569 (2010).
Schambye, H. T. et al. Bicarbonate- versus lactate-based CAPD fluids: a biocompatibility study in rabbits. Perit. Dial. Int. 12, 281–286 (1992).
Krediet, R. T., Zweers, M. M., van Westrhenen, R., Zegwaard, A. & Struijk, D. G. Effects of reducing the lactate and glucose content of PD solutions on the peritoneum. Is the future GLAD? NDT Plus 1 (Suppl. 4), iv56–iv62 (2008).
Zweers, M. M., Splint, L. J., Krediet, R. T. & Struijk, D. G. Ultrastructure of basement membranes of peritoneal capillaries in a chronic peritoneal infusion model in the rat. Nephrol. Dial. Transplant. 16, 651–654 (2001).
Dobbie, J. W., Zaki, M. & Wilson, L. Ultrastructural studies on the peritoneum with special reference to chronic ambulatory peritoneal dialysis. Scott. Med. J. 26, 213–223 (1981).
Pollock, C. A. et al. Peritoneal morphology on maintenance dialysis. Am. J. Nephrol. 9, 198–204 (1989).
Williams, J. D. et al. Morphologic changes in the peritoneal membrane of patients with renal disease. J. Am. Soc. Nephrol. 13, 470–479 (2002).
Vlahu, C. A. et al. Damage of the endothelial glycocalyx in dialysis patients. J. Am. Soc. Nephrol. 23, 1900–1908 (2012).
Yanez-Mo, M. et al. Peritoneal dialysis and epithelial-to-mesenchymal transition of mesothelial cells. N. Engl. J. Med. 348, 403–413 (2003).
Del Peso, G. et al. Epithelial-to-mesenchymal transition of mesothelial cells is an early event during peritoneal dialysis and is associated with high peritoneal transport. Kidney Int. 73, S26–S33 (2008).
Aroeira, L. S. et al. Epithelial to mesenchymal transition and peritoneal membrane failure in peritoneal dialysis patients: pathologic significance and potential therapeutic interventions. J. Am. Soc. Nephrol. 18, 2004–2013 (2007).
Dobbie, J. W. Morphology of the peritoneum in CAPD. Blood Purif. 7, 74–85 (1989).
Di Paolo, N. et al. Morphology of the peritoneal membrane during continuous ambulatory peritoneal dialysis. Nephron 44, 204–211 (1986).
Mateijsen, M. A. et al. Vascular and interstitial changes in the peritoneum of CAPD patients with peritoneal sclerosis. Perit. Dial. Int. 19, 517–525 (1999).
Honda, K. et al. Morphological changes in the peritoneal vasculature of patients on CAPD with ultrafiltration failure. Nephron 72, 171–176 (1996).
Di Paolo, N. & Sacchi, G. Peritoneal vascular changes in continuous ambulatory peritoneal dialysis (CAPD): an in vivo model for the study of diabetic microangiopathy. Perit. Dial. Int. 9, 41–45 (1989).
Krediet, R. T., Van Westrhenen, R., Zweers, M. M. & Struijk, D. G. Clinical advantages of new peritoneal dialysis solutions. Nephrol. Dial. Transplant. 17 (Suppl. 3), 16–18 (2002).
Lee, T.-C., Yang, J.-Y., Wang, H.-P., Tsai, T.-J. & Yang, Y. Peritoneal thickening is not inevitable in long-term peritoneal dialysis and is associated with peritoneal transport characteristics: a two-centre sonographic study. Nephrol. Dial. Transplant. 23, 1005–1010 (2008).
Sampimon, D. E., Coester, A. M., Struijk, D. G. & Krediet, R. T. The time course of peritoneal transport parameters in peritoneal dialysis patients who develop encapsulating peritoneal sclerosis. Nephrol. Dial. Transplant. 26, 291–298 (2011).
Korte, M. R., Sampimon, D. E., Betjes, M. G. & Krediet, R. T. Encapsulating peritoneal sclerosis: the state of affairs. Nat. Rev. Nephrol. 7, 528–539 (2011).
Davies, M. et al. Proteoglycans of CAPD-dialysate fluid and mesothelium. Contr. Nephrol. 85, 134–141 (1990).
Yung, S. et al. Source of peritoneal proteoglycans. Am. J. Pathol. 146, 520–529 (1995).
Yung, S. & Chan, T. M. Pathophysiology of the peritoneal membrane during peritoneal dialysis: the role of hyaluronan. J. Biomed. Biotechnol. http://dx.doi.org/10.1155/2011/180594.
Osada, S. et al. Alterations in proteoglycan components and histopathology of the peritoneum in uraemic and peritoneal dialysis patients. Nephrol. Dial. Transplant. 24, 3504–3512 (2009).
Yamada, K. et al. Immunohistochemical study of human advanced glycosylation end-products (AGE) in chronic renal failure. Clin. Nephrol. 42, 354–361 (1994).
Nakayama, M. et al. Immunohistochemical detection of advanced glycosylation end-products in the peritoneum and its possible pathophysiological role in CAPD. Kidney Int. 51, 182–186 (1997).
Weiss, M. F. et al. Mechanisms for the formation of glyoxidation products in end-stage renal disease. Kidney Int. 57, 2571–2585 (2000).
Combet, S. et al. Vascular proliferation and enhanced expression of endothelial nitric oxide synthase in human peritoneum exposed to long-term peritoneal dialysis. J. Am. Soc. Nephrol. 11, 717–728 (2000).
Kihm, L. P. et al. RAGE expression in the human peritoneal membrane. Nephrol. Dial. Transplant. 23, 3302–3306 (2008).
Makita, Z. et al. Reactive glycosylation endproducts in diabetic uraemia and treatment of renal failure. Lancet 343, 1519–1522 (1994).
Raj, D. S., Choudhury, D., Welbourne, T. C. & Levi, M. Advanced glycation end products: a nephrologist's perspective. Am. J. Kidney Dis. 35, 365–380 (2000).
Friedlander, M. A., Wu, Y.-C., Schulak, J. A., Monnier, V. M. & Hricik, D. E. Influence of dialysis modality on plasma and tissue concentrations of pentosodine in patients with end-stage renal disease. Am. J. Kidney Dis. 25, 445–451 (1995).
Hartog, J. W. et al. Accumulation of advanced glycation end products, measured as skin autofluorescence, in renal disease. Ann. NY Acad. Sci. 1043, 299–307 (2005).
Jiang, J. et al. Accumulation of tissue advanced glycation end products correlated with glucose exposure and associated with cardiovascular morbidity in patients on peritoneal dialysis. Atherosclerosis 224, 187–194 (2012).
McIntyre, N. J. et al. Tissue-advanced glycation end product concentration in dialysis patients. Clin. J. Am. Soc. Nephrol. 5, 51–55 (2010).
Brown, E. et al. Guidelines on encapsulating peritoneal sclerosis (EPS). Perit. Dial. Int. 29, 595–602 (2009).
Dulaney, J. T. & Hatch, F. E. Peritoneal dialysis and loss of proteins: a review. Kidney Int. 26, 253–262 (1984).
Lopes Barreto, D. & Krediet, R. T. Current status and practical use of effluent biomarkers in peritoneal dialysis patients. Am. J. Kidney Dis. (in press).
Cuccurullo, M. et al. Proteomic analysis of peritoneal fluid of patients treated by peritoneal dialysis: effect of glucose concentration. Nephrol. Dial. Transplant. 26, 1990–1999 (2011).
Raaijmakers, R. et al. Proteomic profiling and identification in peritoneal fluid of children treated by peritoneal dialysis. Nephrol. Dial. Transplant. 23, 2402–2405 (2008).
Lin, W. T. et al. Proteomic analysis of peritoneal dialysate fluid in patients with dialysis-related peritonitis. Ren. Fail. 30, 772–777 (2008).
Wang, H. Y. et al. Differential proteomic characterization between normal peritoneal fluid & diabetic dialysate. Nephrol. Dial. Transplant. 25, 1955–1963 (2010).
Sritippayawan, S. et al. Proteomic analysis of peritoneal dialysate fluid in patients with different types of peritoneal membranes. J. Proteome Res. 6, 4356–4362 (2007).
Krediet, R. T. et al. Biological markers in the peritoneal dialysate effluent: are they useful. Contrib. Nephrol. 163, 54–59 (2009).
Zemel, D. et al. Appearance of tumor necrosis factor-α and soluble TNF-receptors I and II in peritoneal effluent of CAPD. Kidney Int. 46, 1422–1430 (1994).
Zweers, M. M., De Waart, D. R., Smit, W., Struijk, D. G. & Krediet, R. T. The growth factors VEGF and TGFβ-1 in peritoneal dialysis. J. Lab. Clin. Med. 134, 124–132 (1999).
Krediet, R. T. Dialysate cancer antigen concentration as marker of peritoneal membrane status in patients treated with chronic peritoneal dialysis. Perit. Dial. Int. 21, 560–567 (2001).
Visser, C. E. et al. Cancer antigen 125: a bulk marker for mesothelial mass in stable peritoneal dialysis patients. Nephrol. Dial. Transplant. 10, 64–69 (1995).
Breborowicz, A., Breborowicz, M., Pyda, M., Polubinska, A. & Oreopoulos, D. Limitations of CA 125 as an index of peritoneal mesothelial cell mass. Nephron Clin. Pract. 100, c46–c51 (2005).
Koomen, G. C. et al. Dialysate cancer antigen (CA) 125 is a reflection of peritoneal cell mass in CAPD patients. Perit. Dial. Int. 14, 132–136 (1994).
Ho-dac-Pannekeet, M. M., Hiralall, J. K., Struijk, D. G. & Krediet, R. T. Longitudinal follow-up of CA125 in peritoneal effluent. Kidney Int. 51, 888–893 (1997).
Lopes-Barreto, D. et al. Variability of effluent cancer antigen 125 and interleukin-6 determination in dialysis patients. Nephrol. Dial. Transplant. 26, 3739–3744 (2011).
Coester, A. M., Zweers, M. M., De Waart, D. E. & Krediet, R. T. The relationship between effluent potassium due to cellular release, free water transport and CA125 in peritoneal dialysis patients. NDT Plus 1, iv41–iv45 (2008).
Sampimon, D. E. et al. Early diagnostic markers for encapsulating peritoneal sclerosis: a case-control study. Perit. Dial. Int. 30, 163–169 (2010).
Goldman, M. et al. Intraperitoneal secretion of interleukin-6 during continuous ambulatory peritoneal dialysis. Nephron 56, 277–280 (1990).
Zemel, D. et al. Interleukin-6 in CAPD patients without peritonitis: relationship to the intrinsic permeability of the peritoneal membrane. Clin. Nephrol. 37, 97–103 (1992).
Pecoits-Filho, R. et al. Plasma and dialysate Il-6 and VEGF concentrations are associated with high peritoneal solute transport rate. Nephrol. Dial. Transplant. 17, 1480–1486 (2002).
Oh, K. H. et al. Intra-peritoneal interleukin-6 system is a potent determinant of the baseline periritoneal solute transport in incident peritoneal dialysis. Nephrol. Dial. Transplant. 25, 1639–1646 (2010).
Rodrigues, A. S. et al. Peritoneal fast transport in incident peritoneal dialysis patients is not consistently associated with systemic inflammation. Nephrol. Dial. Transplant. 21, 763–769 (2006).
Van Esch, S. et al. Determinants of peritoneal solute transport rates in newly started nondiabetic peritoneal dialysis patients. Perit. Dial. Int. 24, 554–561 (2004).
Pecoits-Filho, R., Carvalho, M. J., Stenvinkel, P., Lindholm, B. & Heimburger, O. Systemic and intraperitoneal interleukin-6 system during the first year of peritoneal dialysis. Perit. Dial. Int. 26, 53–63 (2006).
Rodrigues, A. S. et al. Evaluation of peritoneal transport and membrane status in peritoneal dialysis: focus on incident fast transporters. Am. J. Nephrol. 27, 84–91 (2007).
Dvorak, H. F., Brown, L. F., Detmar, M. & Dvorak, A. M. Vascular permeability factor/vascular endothelial growth factor, microvascular hyperpermeability, and angiogenesis. Am. J. Pathol. 146, 1029–1039 (1995).
Tanaka, Y., Katoh, S., Hori, S., Miura, M. & Yamashita, H. Vascular endothelial growth factor in diabetic retinopathy. Lancet 349, 1520 (1997).
Aiello, L. P., Avary, R. L. & Arrigg, P. G. Vascular endothelial growth factor in ocular fluid of patients with diabetic retinopathy and other retina disorders. N. Engl. J. Med. 331, 1480–1487 (1994).
Zweers, M. M., Struijk, D. G. & Krediet, R. T. Vascular endothelial growth factor in peritoneal dialysis, a longitudinal follow-up. J. Lab. Clin. Med. 137, 125–132 (2001).
Shimo, T. et al. Connective tissue growth factor induces proliferation, migration, and tube formation of endothelial cells in vitro, and angiogenesis in vivo. J. Biochem. 126, 137–145 (1999).
Mizutani, M. et al. Connective tissue growth factor (CTGF/CCN2) is increased in peritoneal dialysis patients with high peritoneal solute transport rate. Am. J. Physiol. Renal Physiol. 298, F721–F733 (2010).
Krediet, R. T. et al. Connective tissue growth factor (CTGF) is associated with peritoneal transport parameters. Perit. Dial. Int. 26 (Suppl. 2), S8 (2006).
Ho-dac-Pannekeet, M. M., Hiralall, J. K., Struijk, D. G. & Krediet, R. T. Markers of peritoneal mesothelial cells during treatment with peritoneal dialysis. Adv. Perit. Dial. 13, 72–76 (1997).
Lai, K. N. et al. Increased production of hyaluronan by peritoneal cells and its significance in patients on CAPD. Am. J. Kidney Dis. 32, 318–324 (1999).
Wong, T. Y. et al. Longitudinal study of peritoneal membrane function in continuous ambulatory peritoneal dialysis: relationship with peritonitis and fibrosing factors. Perit. Dial. Int. 20, 679–685 (2000).
Martikainen, T., Ekstrand, A., Honkanen, E., Teppo, A.-M. & Gronhagen-Riska, C. Do interleukin-6, hyaluronan, soluble adhesion molecule-1 and cancer antigen 125 in dialysate predict changes in peritoneal function? Scand. J. Urol. Nephrol. 39, 410–416 (2005).
Yamagata, K., Tomida, C. & Koyama, A. Intraperitoneal hyaluronan production in stable continuous ambulatory peritoneal dialysis patients. Perit. Dial. Int. 19, 131–137 (1999).
Szeto, C. C. et al. Dialysate hyaluronan concentration predicts survival but not peritoneal sclerosis in continuous ambulatory peritoneal dialysis. Am. J. Kidney Dis. 36, 609–614 (2000).
Ho-dac-Pannekeet, M. M. et al. Analysis of non enzymatic glycosylation in vivo: impact of different dialysis solutions. Perit. Dial. Int. 19 (Suppl. 2), S68–S74 (1999).
Ahmad, S. et al. CCL18 in peritoneal dialysis patients and encapsulating peritoneal sclerosis. Eur. J. Clin. Invest. 40, 1067–1073 (2010).
Eddy, A. A. Plasminogen activator inhibitor-1 and the kidney. Am. J. Physiol. Renal Physiol. 283, F209–F220 (2002).
Goedde, M. et al. Coagulation and fibrinolysis-related antigens in plasma and dialysate of CAPD patients. Perit. Dial. Int. 17, 162–166 (1997).
De Boer, A. W. et al. Intraperitoneal hypercoagulation ans hypofibrinolysis is present in childhood peritonitis. Pediatr. Nephrol. 13, 284–287 (1999).
Lopes-Barreto, D., Coester, A. M., Struijk, D. G. & Krediet, R. T. Can effluent matrix metalloproteinase-2 and plasminogen activator-1 be used as biomarkers of peritoneal membrane alterations in peritoneal dialysis patients? Perit. Dial. Int. (in press).
Masunaga, Y. et al. A case of encapsulating peritoneal sclerosis at the clinical early stage with high concentration of matrix metalloproteinase-2 in peritoneal effluent. Clin. Exp. Nephrol. 9, 85–89 (2005).
Hirahara, I. et al. The potential of matrix metalloproteinase-2 as a marker of peritoneal injury, increased solute transport, or progression to encapsulating peritoneal sclerosis during peritoneal dialysis—a multi centre study in Japan. Nephrol. Dial. Transplant. 22, 560–567 (2007).
Hommes, N. H. et al. Matrix metalloproteinase-2 and procollagen lll peptide in peritoneal effluent: relationship with markers of mesothelial cell mass and angiogenesis. Perit. Dial. Int. 23 (Suppl. 1), S8 (2003).
Flessner, M. Osmotic barrier of the parietal peritoneum. Am. J. Physiol. 267, F861–F870 (1994).
Lindholm, B., Heimburger, O., Waniewski, J., Werynski, A. & Bergstrom, J. Peritoneal ultrafiltration and fluid reabsorption during peritoneal dialysis. Nephrol. Dial. Transplant. 4, 805–813 (1989).
Krediet, R. T., Struijk, D. G., Koomen, G. C. & Arisz, L. Peritoneal fluid kinetics during CAPD measured with intraperitoneal dextran 70. ASAIO Trans. 37, 662–667 (1991).
Tran, L. et al. Lymphatic drainage of hypertonic solution from peritoneal cavity of anasthetized and conscious sheep. J. Appl. Physiol. 74, 859–867 (1993).
Zakaria, E. R., Mays, C. J., Matheson, P. J., Hurt, R. T. & Garrison, R. N. Plasma appearance rate of intraperitoneal macromolecular tracer underestimates peritoneal lymph flow. Adv. Perit. Dial. 24, 16–21 (2008).
Zakaria, E. R. & Rippe, B. Peritoneal fluid and tracer albumin kinetics in the rat. Effects of increases in intraperitoneal hydrostatic pressure. Perit. Dial. Int. 15, 118–128 (1995).
Galach, M., Werynski, A., Lindholm, B. & Waniewski, J. in Progress in Peritoneal Dialysis (ed. Krediet, R. T.) 1–22 (InTech, Rijeka, 2011).
Blake, P. G. Controversies in peritoneal dialysis. Perit. Dial. Int. 24, 309–317 (2004).
Pannekeet, M. M. et al. The standard peritoneal permeability analysis: a tool for the assessment of peritoneal permeability characteristics in CAPD patients. Kidney Int. 48, 866–875 (1995).
Smit, W. et al. Peritoneal function and assessment of reference values using a 3.86% glucose solution. Perit. Dial. Int. 23, 440–449 (2003).
Fuszholler, A., Zur Nieden, S., Grabensee, B. & Plum, J. Peritoneal fluid and solute transport: influence of treatment time, peritoneal dialysis modality, and peritonitis incidence. J. Am. Soc. Nephrol. 13, 1055–1060 (2002).
Michels, W. M. et al. Does lymphatic absorption change with the duration of peritoneal dialysis? Perit. Dial. Int. 24, 347–352 (2004).
Coester, A. M., Smit, W., Struijk, D. G., Parikova, A. & Krediet, R. T. Longitudinal analysis of peritoneal fluid transport and its determinants in a cohort of incident PD patients. Perit. Dial. Int. (in press).
Smit, W., Parikova, A., Struijk, D. G. & Krediet, R. T. The difference in causes of early and late ultrafiltration failure in peritoneal dialysis. Perit. Dial. Int. 25 (Suppl. 1), S41–S45 (2005).
Rippe, B. & Haraldsson, B. Transport of macromolecules across microvascular walls. Physiol. Rev. 74, 163–219 (1994).
Nolph, K. D., Hano, J. E. & Teschan, P. E. Peritoneal sodium transport during hypertonic peritoneal dialysis: physiologic mechanisms and clinical implications. Ann. Intern. Med. 70, 931–941 (1969).
Rippe, B. & Stelin, G. Simulations of peritoneal solute transport during CAPD. Application of two-pore formalism. Kidney Int. 35, 1234–1244 (1989).
Rippe, B., Stelin, G. & Haraldsson, B. Computer simulations of peritoneal fluid transport in CAPD. Kidney Int. 40, 315–325 (1991).
Pannekeet, M. M. et al. Demonstration of aquaporin-CHIP in peritoneal tissue of uremic and CAPD patients. Perit. Dial. Int. 19 (Suppl. 1), S54–S57 (1996).
Ni, J. et al. Aquaporin-1 plays an essential role in water permeability and ultrafiltration during peritoneal dialysis. Kidney Int. 69, 1518–1525 (2006).
Smit, W., Struijk, D. G., Ho-dac-Pannekeet, M. M. & Krediet, R. T. Quantification of free water transport in peritoneal dialysis. Kidney Int. 66, 849–854 (2004).
La Milia, V. et al. Mini-peritoneal equilibration test: a simple and fast method to assess free water and small solute transport across the peritoneal membrane. Kidney Int. 68, 840–846 (2005).
Parikova, A., Smit, W., Struijk, D. G., Zweers, M. M. & Krediet, R. T. The contribution of free water transport and small pore transport to the total fluid removal in peritoneal dialysis. Kidney Int. 68, 1849–1856 (2005).
Parikova, A., Smit, W., Zweers, M. M., Struijk, D. G. & Krediet, R. T. Free water transport, small pore transport and the osmotic gradient. Nephrol. Dial. Transplant. 23, 2350–2355 (2008).
Numata, M. et al. Association between an increased surface area of peritoneal microvessels and a high peritoneal solute transport rate. Perit. Dial. Int. 23, 116–122 (2003).
Davies, S. J., Brown, B., Bryan, J. & Russel, G. I. Clinical evaluation of the peritoneal equilibration test: a population-based study. Nephrol. Dial. Transplant. 8, 64–70 (1993).
Smit, W. et al. Free water transport in fast transport status: a comparison between CAPD peritonitis and long-term PD. Kidney Int. 65, 298–303 (2004).
Parikova, A., Smit, W., Struijk, D. G. & Krediet, R. T. Analysis of fluid transport pathways and their determinants in peritoneal dialysis patients with ultrafiltration failure. Kidney Int. 70, 1988–1994 (2006).
Michels, W. M. et al. Time course of peritoneal function in automated and continuous peritoneal dialysis. Perit. Dial. Int. 32, 605–611 (2012).
Lo, W. K. et al. Changes in the peritoneal equilibration test in selected chronic peritoneal dialysis patients. J. Am. Soc. Nephrol. 4, 1466–1474 (1994).
Struijk, D. G. et al. A prospective study of peritoneal transport in CAPD patients. Kidney Int. 45, 1739–1744 (1994).
Heimburger, O., Wang, T. & Lindholm, B. Alterations in water and solute transport with time on peritoneal dialysis. Perit. Dial. Int. 19 (Suppl. 2), S83–S90 (1999).
Del Peso, G. et al. Factors influencing peritoneal transport parameters during the first year on peritoneal dialysis: peritonitis is the main factor. Nephrol. Dial. Transplant. 20, 1201–1206 (2005).
Clerbaux, G., Francart, J., Wallemacq, P., Robert, A. & Goffin, E. Evaluation of peritoneal transport properties at onset of peritoneal dialysis and longitudinal follow-up. Nephrol. Dial. Transplant. 21, 1032–1039 (2006).
Fernandez-Reyes, M. J. et al. The influence of initial peritoneal transport characteristics, inflammation, and high glucose exposure on prognosis of peritoneal membrane function. Perit. Dial. Int. 32, 636–644 (2012).
Davies, S. J., Bryan, J., Phillips, L. & Russel, G. I. Longitudinal changes in peritoneal kinetics: the effects of peritoneal dialysis and peritonitis. Nephrol. Dial. Transplant. 11, 498–506 (1996).
Fernandez-Reyes, M. J. et al. Inherent high peritoneal transport and ultrafiltration deficiency: their mid-term clinical relevance. Nephrol. Dial. Transplant. 22, 218–223 (2007).
Oliveira, L. & Rodrigues, A. Previous renal replacement therapy time at start of peritoneal dialysis independently impact on peritoneal membrane ultrafiltration failure. Int. J. Nephrol. http://dx.doi.org/10.4061/2011/685457.
Chung, S. H. et al. Peritoneal transport characteristics, comorbid diseases and survival in CAPD patients. Perit. Dial. Int. 20, 541–547 (2000).
Szeto, C. C., Law, M. C., Wong, T. Y., Leung, C. B. & Li, P. K. Peritoneal transport status correlates with morbidity but not longitudinal change of nutritioinal status of continuous ambulatory peritoneal dialysis patients: a 2-year prospective study. Am. J. Kidney Dis. 37, 329–336 (2001).
Selgas, R. et al. Ultrafiltration and small solute transport at initiation of PD: Questioning the paradigm of peritoneal function. Perit. Dial. Int. 25, 68–70 (2005).
Smit, W. et al. Analysis of the prevalence and causes of ultrafiltration failure during long-term peritoneal dialysis: a cross-sectional study. Perit. Dial. Int. 24, 562–570 (2004).
Davies, S. J. Longitudinal relationship between solute transport and ultrafiltration capacity in peritoneal dialysis patients. Kidney Int. 66, 2437–2445 (2004).
Lambie, M. L., John, B., Mushahar, L., Huckvale, C. & Davies, S. J. The peritoneal osmotic conductance is low well before the diagnosis of encapsulating peritoneal sclerosis is made. Kidney Int. 78, 611–618 (2010).
Feit, J., Richard, C., McCaffrey, C. & Levy, M. Peritoneal clearance of creatinine and inulin in dogs: effect of splanchnic vasodilators. Kidney Int. 16, 459–469 (1979).
Pietrzak, I. et al. Splanchnic volume, not flow rate, determines peritoneal permeability. ASAIO Trans. 35, 583–587 (1989).
Kim, M., Lofthouse, J. & Flessner, M. F. A method to test blood flow limitation of peritoneal-blood solute transport. J. Am. Soc. Nephrol. 8, 471–474 (1997).
Flessner, M. F., Henegar, J., Bigler, S. & Genous, L. Is the peritoneum a significant transport barrier in peritoneal dialysis? Perit. Dial. Int. 23, 542–549 (2003).
Levick, J. R. Flow through interstitium and other fibrous matrices. Q. J. Exp. Physiol. 72, 409–438 (1987).
Fox, J. R. & Wayland, H. Interstitial diffusion of macromolecules in the rat mesentery. Microvasc. Res. 18, 255–276 (1979).
Flessner, M. F., Fenstermacher, J. D., Dedrick, R. L. & Blasberg, R. G. A distributed model of peritoneal-plasma transport: tissue concentration gradients. Am. J. Physiol. 248, F425–F435 (1985).
Wiig, H., DeCarlo, M., Sibley, L., Renkin, E. M. Interstitial exclusion of albumin in rat tissues measured by a continuous infusion method. Am. J. Physiol. 263, H1222–H1233 (1992).
Hirszel, P., Shea-Donohue, T., Chakrabarti, E., Montcalm, E. & Maher, J. F. The role of the capillary wall in restricting diffusion of macromolecules. Nephron 49, 58–61 (1988).
Lasrich, M., Maher, J. M, Hirszel, P. & Maher, J. F. Correlation of peritoneal transport rates with molecular weight: a method for predicting clearances. ASAIO J. 2, 107–113 (1979).
Leypoldt, J. K., Parker, H. R., Frigon, R. P. & Henderson, L. W. Molecular size dependence of peritoneal transport. J. Lab. Clin. Med. 110, 207–216 (1987).
Krediet, R. T., Zuyderhoudt, F. M., Boeschoten, E. W. & Arisz, L. Alterations in the peritoneal transport of water and solutes during peritonitis in continuous ambulatory peritoneal dialysis patients. Eur. J. Clin. Invest. 17, 43–52 (1987).
Krediet, R. T. et al. The peritoneal transport of serum proteins and neutral dextran in CAPD patients. Kidney Int. 35, 1064–1072 (1989).
Gotloib, L., Bar Sella, P. & Shustack, A. Ruthenium-red-stained polyanionic fixed charges in peritoneal microvessels. Nephron 47, 22–28 (1998).
Buis, B. et al. Effect of electric charge on the transperitoneal transport of plasma proteins during CAPD. Nephrol. Dial. Transplant. 11, 1113–1120 (1996).
Zemel, D., Krediet, R. T., Koomen, G. C., Struijk, D. G. & Arisz, L. Day to day variability of protein transport used as a method for the analysis of peritoneal permeability in continuous ambulatory peritoneal dialysis patients. Perit. Dial. Int. 11, 217–223 (1991).
Rumpsfeld, M., McDonald, S. P., Purdie, D. M., Collins, J. & Johnson, D. W. Predictors of baseline peritoneal transport status in Australian and New Zealand peritoneal dialysis patients. Am. J. Kidney Dis. 43, 492–501 (2004).
Serlie, M. J., Struijk, D. G., de Blok, K. & Krediet, R. T. Differences in fluid and solute transport between diabetic and nondiabetic patients at the onset of CAPD. Adv. Perit. Dial. 13, 29–32 (1997).
Hendriks, P. M. et al. Peritoneal sclerosis in chronic peritoneal dialysis patients: analysis of clinical presentation, risk factors, and peritoneal transport kinetics. Perit. Dial. Int. 17, 136–143 (1997).
Davies, S. J., Phillips, L., Naish, P. F. & Russell, G. I. Peritoneal glucose exposure and changes in membrane solute transport with time on peritoneal dialysis. J. Am. Soc. Nephrol. 12, 1046–1051 (2001).
Goel, S., Kathuria, P., Moore, H. L., Prowant, B. F. & Nolph, K. D. The effect of peritonitis on the peritoneal membrane transport properties in patients on CAPD. Adv. Perit. Dial. 12, 181–184 (1996).
Kolesnyk, I. et al. The impact of ACE inhibitors and AII receptor blockers on the peritoneal membrane transport characteristics in long-term PD patients. Perit. Dial. Int. 27, 446–453 (2007).
Kolesnyk, I. et al. A positive effect of AII inhibitors on peritoneal membrane function in long-term PD patients. Nephrol. Dial. Transplant. 24, 272–277 (2009).
Selgas, R. et al. Stability of the peritoneal membrane in long-term peritoneal dialysis patients. Adv. Ren. Replace. Ther. 5, 168–178 (1998).
Rodrigues, A., Cabrita, A., Maia, P. & Guimares, S. Peritoneal rest may successfully recover ultrafiltration in patients who develop hyperpermeability with time on continuous ambulatory peritoneal dialysis. Adv. Perit. Dial. 18, 78–80 (2002).
Struijk, D. G. et al. Functional characteristics of the peritoneal membrane in long-term continuous ambulatory peritoneal dialysis. Nephron 59, 213–220 (1991).
Ho-dac-Pannekeet, M. M., Koopmans, J. G., Struijk, D. G. & Krediet, R. T. Restriction coefficients of low molecular weight solutes and macromolecules during peritoneal dialysis. Adv. Perit. Dial. 13, 17–22 (1997).
Author information
Authors and Affiliations
Contributions
The authors contributed equally to all aspects of this manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing financial interests.
Rights and permissions
About this article
Cite this article
Krediet, R., Struijk, D. Peritoneal changes in patients on long-term peritoneal dialysis. Nat Rev Nephrol 9, 419–429 (2013). https://doi.org/10.1038/nrneph.2013.99
Published:
Issue Date:
DOI: https://doi.org/10.1038/nrneph.2013.99
This article is cited by
-
Melatonin decreases GSDME mediated mesothelial cell pyroptosis and prevents peritoneal fibrosis and ultrafiltration failure
Science China Life Sciences (2024)
-
Tamoxifen exerts anti-peritoneal fibrosis effects by inhibiting H19-activated VEGFA transcription
Journal of Translational Medicine (2023)
-
STAT3/HIF-1α signaling activation mediates peritoneal fibrosis induced by high glucose
Journal of Translational Medicine (2021)
-
The osmo-metabolic approach: a novel and tantalizing glucose-sparing strategy in peritoneal dialysis
Journal of Nephrology (2021)
-
Peritoneal Dialysis Guidelines 2019 Part 1 (Position paper of the Japanese Society for Dialysis Therapy)
Renal Replacement Therapy (2021)