Abstract
Posttraumatic stress disorder (PTSD) is a debilitating disorder that has been associated with brain abnormalities, including white matter alterations. However, little is known about the effect of treatment on these brain alterations. To investigate the course of white matter alterations in PTSD, we used a longitudinal design investigating treatment effects on white matter integrity using diffusion tensor imaging (DTI). Diffusion tensor and magnetization transfer images were obtained pre- and posttreatment from veterans with (n=39) and without PTSD (n=22). After treatment, 16 PTSD patients were remitted, and 23 had persistent PTSD based on PTSD diagnosis. The dorsal and hippocampal cingulum bundle, stria terminalis, and fornix were investigated as regions of interest. Exploratory whole-brain analyses were also performed. Groups were compared with repeated-measures ANOVA for fractional anisotropy (FA), and magnetization transfer ratio. Persistently symptomatic PTSD patients had increasing FA of the dorsal cingulum over time, and at reassessment these FA values were higher than both combat controls and the remitted PTSD group. Group-by-time interactions for FA were found in the hippocampal cingulum, fornix, and stria terminalis, posterior corona radiata, and superior longitudinal fasciculus. Our results indicate that higher FA of the dorsal cingulum bundle may be an acquired feature of persistent PTSD that develops over time. Furthermore, treatment might have differential effects on the hippocampal cingulum, fornix, stria terminalis, posterior corona radiata, and superior longitudinal fasciculus in remitted vs persistent PTSD patients. This study contributes to a better understanding of the neural underpinnings of PTSD treatment outcome.
Similar content being viewed by others
INTRODUCTION
Posttraumatic stress disorder (PTSD) is a trauma and stressor-related disorder that is prevalent in about 6–13% of veterans deployed to Iraq or Afghanistan (Hoge et al, 2004; Reijnen et al, 2014). Understanding PTSD pathophysiology and treatment can contribute to the improvement of interventions and perhaps the prevention of the development of PTSD (Linden, 2006). Although trauma-focused therapy is available and effective to treat PTSD, by inducing fear extinction of trauma-related memories (Foa and Kozak, 1986; Rothbaum and Davis, 2003), not all patients remit from PTSD (Bisson et al, 2007). Using a longitudinal design, we investigated neurobiological alterations in PTSD patients and combat controls before and after treatment.
PTSD has been associated with a hyperactive limbic system (eg, amygdala), and a hypoactive emotional regulation system (eg, anterior cingulate cortex (ACC), prefrontal cortex (PFC); Hayes et al, 2012; Rauch et al, 2006). Recently, research with structural and functional magnetic resonance imaging (MRI) has started to disentangle whether neurobiological alterations found in PTSD change after successful treatment. Some studies have shown that treatment potentially normalizes activity in the limbic system and regulatory brain areas (eg, amygdala, ACC; Aupperle et al, 2013; Fani et al, 2011; Roy et al, 2010). In addition, functional neuroimaging studies have reported treatment outcome to be related to pretreatment structure and activity of limbic and regulatory regions, such as the ACC (Aupperle et al, 2013; Bryant et al, 2008; Dickie et al, 2013; van Rooij et al, 2014, in preparation). These results indicate the possibility of using brain-based biological markers as pretreatment outcome predictors, and suggest the possibility that there are potential differences in the neurobiology of remitted PTSD patients compared with those that fail to respond to treatment.
In cross-sectional studies using diffusion tensor imaging (DTI), white matter microstructure alterations have been reported in PTSD (Daniels et al, 2013). From these studies, fractional anisotropy (FA) is most frequently obtained as a parameter of interest. FA is a measure sensitive to alterations in axonal directionality and white matter organization (Beaulieu, 2009). Reduced FA in the cingulum bundle has frequently been reported in PTSD patients (Fani et al, 2012; Kim et al, 2005; Sanjuan et al, 2013; Schuff et al, 2011), although heightened FA in the cingulum bundle has also been reported (Abe et al, 2006; Zhang et al, 2012). One longitudinal study has investigated white matter microstructure in a small sample of only eight PTSD patients, 10 and 24 months after experiencing a traumatic event (Zhang et al, 2011). An increase in FA in the posterior cingulum bundle over time was reported (Zhang et al, 2011). However, no control group was included in this study and the relation to symptom improvement was not directly assessed. Thus, it remains unclear as to whether or not white matter microstructure of the cingulum bundle changes in relation to PTSD treatment outcome.
In addition, we were interested in investigating other structures. The stria terminalis and fornix are important association pathways of the limbic system, which are involved in the formation of emotional memory, fear, and anxiety (Avery et al, 2014; Gray 1982). The stria terminalis comprises connections between the amygdala and the bed nucleus of the stria terminalis (BNST), whereas the fornix connects the hippocampi with the septal area and hypothalamus (Mori et al, 2008). Although literature is abundant on altered functioning of the amygdala and hippocampus in PTSD, to our knowledge the stria terminalis and the fornix, tracts that form crucial connections among these brain areas, have not been systematically investigated in PTSD patients.
In the current study, we investigate trauma-focused therapy effects on white matter microstructure of the cingulum bundle, stria terminalis, and fornix in PTSD patients vs combat controls with DTI, which provides information about axonal orientation and density (Beaulieu, 2009). In addition, magnetization transfer images are investigated, which can provide additional information on density of macromolecules, and can be sensitive to white matter degradation (Henkelman et al, 2001). Scans were acquired before treatment (baseline) and after ~6–8 months of trauma-focused therapy (posttreatment). In addition, whole-brain analyses were performed to provide a comprehensive unrestricted survey of potential treatment-related white matter differences. We included a deployed, trauma-exposed comparison group to control for the effects of time and deployment (Van Wingen et al, 2012). Using treatment outcome as an indicator, patients with remitted PTSD were compared with patients who still had a PTSD diagnosis after treatment (persistent PTSD), and with combat controls. We expected to observe: (a) an interaction effect caused by differences between PTSD patients and combat controls at baseline, with remitted PTSD patients becoming comparable with combat controls after treatment (recovery-related changes; normalization), and (b) treatment outcome-related differences (remitted and persistent PTSD differences). More specifically, based on previous research we expected lower baseline FA values in the cingulum bundle that may restore to control levels after treatment, and lower cingulum FA in persistent vs remitted PTSD patients.
MATERIALS AND METHODS
Participants and Clinical Assessment
In total, 41 male veterans with PTSD and 24 male veterans without PTSD (combat controls) were included in this study. PTSD patients were recruited from one of four outpatient clinics of the Military Mental Healthcare Organization. PTSD was diagnosed by a clinician according to the DSM-IV criteria (American Psychiatric Association, 1994), and PTSD severity was assessed with the clinician-administered PTSD scale (CAPS; Blake et al, 1995). A clinician or trained researcher administered the interviews. Control participants were recruited via advertisements. For all participants, the presence of (comorbid) disorders or lifetime disorders was assessed with the Structured Clinical Interview for DSM IV (SCID-I; First et al, 1997). At the time of inclusion, all PTSD patients had current PTSD (CAPS≥45), no current alcohol or substance dependence, and no neurological disorder. Combat controls included in the study had no clinical PTSD symptoms (CAPS ≤15), no current psychiatric disorder, no alcohol or substance dependency, and no neurological disorder. After inclusion and a baseline MRI scan (baseline), patients underwent trauma-focused therapy, which consisted of trauma-focused cognitive behavioral therapy (TFCBT) with exposure and/or eye movement desensitization and reprocessing (EMDR), in accordance with Dutch and international treatment guidelines (Balkom et al, 2013; Foa and Meadows, 1997). Treatment selection was part of ‘treatment as usual’, applied by a clinician. The clinician decided whether TFCBT or EMDR was applied as initial therapy. TFCBT and EMDR have been shown to have similar efficacy (Bisson et al, 2007). After an interval of 6–8 months, all participants were reassessed with clinical interviews (CAPS and SCID-I) and MRI protocol (posttreatment). PTSD patients were divided into a remitted group (when no PTSD diagnosis was present at the second clinical assessment according to the DSM-IV criteria; First et al, 1997) and a symptom persistent group (PTSD patients who still had a diagnosis of PTSD at the second assessment; persistent PTSD).
After written and verbal explanation of the study was given, all participants gave informed consent. This study was approved by the medical ethical committee of the University Medical Center Utrecht and was performed in accordance with the Declaration of Helsinki (World Medical Association, 2013).
Image Acquisition and Processing
Diffusion and magnetic transfer images were obtained using a 3.0 T magnetic resonance imaging scanner (Philips Medical System, Best, The Netherlands) at both time points (for scan parameters see Supplementary Information). Quality of these images was assessed and scans with bad quality were excluded from further analysis (PTSD patients n=1, control n=2). One PTSD patient was excluded from all analyses because normalization was not possible. Preprocessing steps for the diffusion images were performed with FSL, CAMINO, and DTI-TK (see Supplementary Information). Briefly, processing included distortion correction, tensor model fitting, and normalization to MNI space. Scalars of the tensor image were calculated (FA, radial diffusivity (RD), axial diffusivity (AD), and mean diffusivity (MD)), and smoothed (FWHM 8 mm) to increase the signal-to-noise ratio. FA is a fraction of diffusion in all directions, which is sensitive to axonal directionality relative to RD, and can be regarded as a summary measure for microstructural integrity (Alexander et al, 2011). FA was the initial scalar of interest. To specify which process is potentially altered, RD, AD, and MD were additionally investigated. RD represents the diffusivity in the direction perpendicular to the white matter tract and is sensitive to demyelination and axonal diameter (Alexander et al, 2011). AD represents diffusion parallel to white matter and is sensitive to general axonal damage (Alexander et al, 2011). MD is the average diffusivity in all directions and represents isotropic diffusivity, which is high in cerebrospinal fluid, and is sensitive to cellular damage (eg, edema and necrosis; Alexander et al, 2011).
The magnetization transfer images were registered to the unweighted diffusion image (b0). The magnetization transfer ratio (MTR) was calculated by subtracting the image with magnetization prepulse from the baseline image and then dividing the residual by the baseline image. The resulting MTR images were normalized to the diffusion group template using DTI-TK.
Statistical Analysis
Tract-based analyses
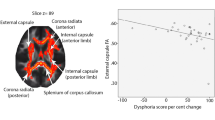
The cingulum bundle is a C-shaped bundle that runs between the ACC and the entorhinal cortex, and can be subdivided into a dorsal and hippocampal region (see Figure 1a and b). Regions of interest (ROIs) were created for the bilateral dorsal and hippocampal cingulum bundle subdivisions, derived from the JHU-ICBM-81 atlas template (Mori et al, 2005).
Regions of interest are presented that are investigated in the tract-based analysis: (a, left) Dorsal cingulum (pink), (b, left) hippocampal cingulum (light green), and (c) fornix (green) and stria terminalis (red).
To extract tracts not available in the JHU white matter atlas, we ran whole-brain deterministic tractography, using the tensor template in MNI space. The stria terminalis was iteratively traced with respect to its known anatomical boundaries by placing ROI’s in the amygdala and BNST (Avery et al, 2014; Mori et al, 2005). Tracing was verified by two researchers, MK and DPMT. The fornix was dissected following manual dissecting protocols by placing an ROI in the body of the fornix (Mori et al, 2005; see Figure 1c and d).
Mean FA and MTR values were extracted for these ROIs and exported into IBM SPSS Statistics for Windows Version 21.0 (IBM Corporation, Armonk, NY) for statistical testing. A general linear model for repeated measures was applied for all ROIs (fornix and left and right dorsal cingulum, hippocampal cingulum, stria terminalis) for FA and MTR to compare the patients with remitted PTSD, the patients with persistent PTSD, and the combat controls at both time points. Additional analyses of RD, AD, and MD were applied when an effect for FA was found, to specify which processes were altered. Post hoc tests were performed when multivariate interaction effects were found. Analyses were covaried for the whole-brain baseline mean of the eigenvalue tested, and age.
Voxel-wise analyses
From the individual pairs of FA maps (baseline and posttreatment), difference in FA maps (ΔFA maps) and mean FA maps were created to explore the interaction between time and group, and the group effect, respectively, using FSL randomize. Threshold-free cluster enhancement (TFCE-corrected p<0.05; Smith and Nichols 2009) was used to correct for multiple comparison, using a white matter mask.
RESULTS
Participants
An overview of demographical and clinical information is presented in Table 1. After treatment, 16 PTSD patients recovered from PTSD (remitted PTSD); 23 PTSD patients had not recovered and still fulfilled the DSM-IV criteria for PTSD (persistent PTSD). The combat controls, and the remitted and persistent PTSD groups did not differ in age (F(2,56)=0.520, p=0.597), educational level (F(2,.56=1.47, p=0.863), the number of times they were deployed (χ2(14)=13.343, p=0.500), time since last deployment (F(2,56)=0.291, p=0.749), and interval between scans (F(2,56)=1.112, p=0.337). The number of subjects who (self-) reported being exposed to blast during deployment was more prevalent in the persistent PTSD group (χ2(1)=6.306, p=0.043).
No difference between the remitted PTSD patients and persistent PTSD patients was found in the total number of treatment sessions between scans (t(33)=−0.008, p=0.993). More specifically, no difference was found between the remitted PTSD patients and persistent PTSD patients in the number of TFCBT sessions (t(33)=0.11, p=0.91), or the number of EMDR sessions between scans (t(33)=−0.15, p=0.88). The persistent PTSD group had a higher CAPS score at baseline (t(36)=−2.31, p=0.027), as well as after treatment (t(37)=−7.295, p=0.000). Control participants had a mean CAPS score of 4.5 (±4.3) at both time points. One control participant used psychotropic medication (Ritalin), all the others did not use psychotropic medication. Comorbidity of anxiety disorders was more prevalent in the persistent PTSD group vs the remitted PTSD group at baseline (χ2(1)=5.30, p=0.037), and a trend was observed for mood disorders (χ2(1)=3.95, p=0.059). Posttreatment comorbidity was only present in the patients with persistent PTSD. The PTSD groups did not differ on psychotropic medication use. None of the participants was physically injured during deployment.
Tract-Based Analyses
A significant multivariate group-by-time interaction effect was found for FA values (Wilks’ λ=0.589, F(14,100)=2.167, p=0.014). The interaction effect was driven by interactions in the left dorsal cingulum, left hippocampal cingulum, bilateral stria terminalis, and fornix FA, which will be described below (see Figures 2 and 3). There were no significant correlations between the differences in tract FA values over time and symptom improvement within the groups. No significant effects were observed for MTR, AD, RD, and MD.
A group-by-time interaction effect was found in the left dorsal cingulum. (a) F-values overlaid on left cingulum bundle and (b) left dorsal cingulum fractional anisotropy (FA) at baseline and posttreatment for the combat controls (green solid line), remitted (blue dashed line), and persistent posttraumatic stress disorder (PTSD) patients (red dotted line).
Group-by-time interaction effects in mean fractional anisotropy (FA) values in the left hippocampal cingulum bundle (a), fornix (b), and stria terminalis (c and d). The lines presents the mean FA values for the combat controls (green solid line), remitted (blue dashed line), and persistent posttraumatic stress disorder (PTSD) patients (red dotted line).
Dorsal cingulum
A group-by-time interaction effect was found for the left dorsal cingulum (F(2,56)=3.932, p=0.026). After treatment, persistent PTSD patients had higher FA in the left dorsal cingulum compared with combat controls (p=0.026), and remitted PTSD patients (p=0.062). The groups did not differ significantly at baseline. A significant increase in left dorsal cingulum FA over time was found in persistent PTSD patients (p=0.008). This indicates that higher FA develops over the course of treatment in persistent PTSD patients.
Of note, a univariate main effect of group (uncorrected) was observed in the right dorsal cingulum (F(2,.56)=4.614, p=0.014), where patients with persistent PTSD had higher FA in the dorsal cingulum compared with the remitted PTSD group, and combat controls across both time points.
Hippocampal cingulum
An interaction between time and group was found for left hippocampal cingulum FA (F(2,56)=4.491, p=0.016). There were no main effects for group or time. Remitted PTSD patients showed a nonsignificant reduction in FA over time towards the FA values of combat controls, the combat controls had a nonsignificant increase in FA over time, and persistent PTSD patients show stable (heightened) FA levels. This pattern suggests that changes in hippocampal cingulum FA may be recovery-related.
Stria terminalis
A significant interaction between time and group was found for bilateral stria terminalis FA (F(2,56)=3.379, p=0.041; F(2,56)=6.690, p=0.002), in the absence of main effects for group or time. Persistent PTSD patients showed a nonsignificant increase in FA over time and the remitted PTSD patients showed a nonsignificant decrease in FA over time, whereas controls showed stable lower FA values.
Fornix
A group-by-time interaction was found for fornix FA (F(2,56)=3.908, p=0.026), in the absence of main effects for group or time. Persistent PTSD patients had a nonsignificant increase in FA vs remitted PTSD and controls who displayed a nonsignificant decrease in FA.
Voxel-Wise Analyses
Exploration of whole-brain effects revealed a significant group-by-time interaction in two clusters of voxels. The largest cluster was located in the left posterior corona radiata (k=218, p=0.004, peak voxel: F=19.37, MNI coordinates x=−22, y=−40, z=35; see Figure 4). A second cluster was located in the superior longitudinal fasciculus (k=16, p=0.049, peak voxel: F=10.47, MNI coordinates x=−31, y=−43, z=26; see Figure 4). The interaction effect for both clusters was driven by a significant decrease in FA in the patients with remitted PTSD vs a significant increase in FA in combat controls, whereas the persistent PTSD group did not differ over time. The change in FA in the posterior corona radiata correlated with the percentage change in CAPS score (Pearson’s r=0.451, p=0.004).
Whole-brain time-by-group interaction effect in the left posterior corona radiata and superior longitudinal fasciculus (a: TFCE-corrected p<0.05). The tracts that run through this cluster are visualized in (b).
DISCUSSION
This is the first longitudinal study to report treatment-related differences in white matter microstructure between remitted and persistent PTSD patients, and combat controls. After treatment, higher FA values in the dorsal cingulum were found in patients with persistent PTSD vs patients with remitted PTSD and combat controls, indicating that white matter microstructure in the dorsal cingulum may be an acquired feature of persistent PTSD that develops over time. In addition, group-by-time interaction effects were found for the left hippocampal cingulum, fornix, stria terminalis, posterior corona radiata, and superior longitudinal fasciculus.
Cross-sectional studies have previously found higher dorsal cingulum FA in PTSD patients compared with controls (Abe et al, 2006; Zhang et al, 2012). We showed that this heightened FA was specific to patients with persistent PTSD, who differed from both combat controls and remitted PTSD patients after treatment. The dorsal cingulum runs from subcallosal frontal cortex to the posterior cingulate cortex (PCC), forming connections between the cingulate cortex and frontal and parietal brain areas (Mori et al, 2005). Heightened functional activation of the dorsal ACC and PCC has been reported in a meta-analysis of PTSD studies (Hayes et al, 2012). Moreover, altered PCC–medial PFC connectivity has been shown in PTSD patients both during a working memory task (increased) (Daniels et al, 2010) and at rest (decreased) (Bluhm et al, 2009). Interestingly, in a recent study by our group, persistent PTSD patients showed increased dorsal ACC activity towards negative images, whereas remitted PTSD patients did not (van Rooij et al, in preparation). In line with these studies, our results show increased white matter microstructural integrity in the cingulum bundle near the PCC and dorsal ACC (see Figure 2). Taken together with previous findings, our results suggest that altered dorsal cingulum structure may complement altered cingulate function and be specific for treatment-resistant PTSD that develops or progresses over time.
The only previous longitudinal DTI study that was performed in a small sample of PTSD subjects found an increase in (posterior) cingulum FA values over time in PTSD patients with persistent symptoms, although no control group was included (Zhang et al, 2011). We complement these findings by showing that persistent PTSD patients had increasing FA in the dorsal cingulum over time, and higher FA values after treatment compared with remitted PTSD patients and controls. Interestingly, a correlation between state anxiety and an increase in left cingulum FA over time has been reported in recently traumatized subjects (Sekiguchi et al, 2014), suggesting that some individuals develop heightened FA early after trauma. In the current study, there were indications (that is an uncorrected group difference in right cingulum) that FA was already heightened at baseline. Therefore, future studies should follow-up recently traumatized subjects during the development of PTSD (and compare these with controls over time) to investigate if FA increases before or after the onset of PTSD. These studies will help determine if altered cingulum FA is a biomarker or, perhaps more interestingly, a mechanism that underlies persistent PTSD, and can be the target of early interventions to prevent persistent PTSD.
The interaction effect in the dorsal cingulum may be related to neural plasticity. As noted, previous studies reported increased cingulum cortex activity (Hayes et al, 2012), in particular in persistent PTSD patients (van Rooij et al, in preparation). Cortical activity has been reported to modulate myelination (Wang and Young, 2014), and increased FA values have been reported after learning (Concha, 2014). Therefore, we can speculate that hyperactivity of the cingulate cortex (eg, during intrusions) may augment a kind of ‘fear learning’ by initiating dorsal cingulum bundle myelination, resulting in higher FA. Some studies support this suggestion; higher cingulum bundle FA in particular has been reported after fear conditioning in rats (Ding et al, 2013), and higher cingulum bundle FA has been related to state anxiety after an earthquake (Sekiguchi et al, 2014). Further studies could confirm this suggestion by investigating the relation between heightened FA and heightened activity in PTSD.
In this study using a longitudinal design and a non-PTSD combat control group to account for trauma exposure and deployment effects, we found increased dorsal cingulum FA in PTSD patients. In contrast, previous studies have reported decreased cingulum FA of PTSD patients (Fani et al, 2012; Kim et al, 2005; Sanjuan et al, 2013; Schuff et al, 2011). These inconsistencies in cingulum FA are likely due to differences in study design (eg, cross-sectional, no control group), or inclusion of non-deployed controls. These differences, along with the observation that deployment has been shown to reduce white matter microstructure integrity in the brainstem (Van Wingen et al, 2012), suggest that future studies aimed at understanding the neurobiology of PTSD in combat-deployed PTSD patients must include a combat-exposed control group.
The hippocampal cingulum FA values of remitted PTSD patients showed a pattern for recovery, as remitted PTSD patients show nonsignificant heightened baseline FA values that are more comparable to controls after treatment. This could reflect normalization of hippocampal cingulum FA values in remitted PTSD patients, although no group effects were observed at either time point and none of the groups showed a significant change over time. The hippocampal cingulum comprises connections between the cingulate cortex and the temporal lobe, including the hippocampus and amygdala (Mori et al, 2005). Restoration of hippocampal and ACC structure and function has previously been reported in PTSD after treatment (Lindauer et al, 2005; Roy et al, 2010). Furthermore, altered connectivity between temporal regions and the PCC and ACC has been reported in PTSD during a working memory task (Daniels et al, 2010), and a resting state (Kennis et al, 2014). Potentially, our results, suggesting normalization of increased hippocampal cingulum FA, may be related to restoration of hippocampal and ACC structure and function, and connectivity from medial temporal brain areas to the cingulate cortex.
The interaction effects in stria terminalis and fornix were characterized by differential FA time-related patterns between remitted (nonsignificant decrease) and persistent (nonsignificant increase) PTSD patients. This might indicate that different processes take place during a period of treatment that differentially alter these limbic tracts. For example, we could speculate that processes of fear extinction take place in remitted PTSD during exposure therapy, whereas fear reinstatement processes take place in persistent PTSD patients, which are processes that involve the fornix and stria terminalis (Philip et al, 2013). However, there were no significant changes in any group over time, and no group differences at any time point. Therefore, caution should be taken with interpreting these effects, as partial voluming effects and delineation of the stria terminalis could confound our results. Further studies should investigate the time course of the hippocampal cingulum, stria terminalis, and fornix to confirm the observed patterns.
Whole-brain voxel-wise correlation analyses revealed a significant decrease over time in the posterior corona radiata and superior longitudinal fasciculus FA of remitted PTSD patients. The posterior corona radiata comprises thalamocortical and corticospinal projections, which are postulated to be important in the psychopathology of PTSD (Lanius et al, 2003). Alterations in superior longitudinal fasciculus FA values have previously been reported in PTSD patients compared with trauma-exposed controls (Daniels et al, 2013). However, the pattern of the interactions found in the current study was not consistent with a normalization of function as was expected, but rather showed more deviation of the remitted PTSD patients from combat controls at reassessment. In addition, it was not expected that the combat controls would demonstrate time-related increases in FA, as was found for the posterior corona radiata. Therefore, it is unclear how to interpret these results and replication of this finding is necessary.
Blast exposure during deployment was more prevalent in persistent PTSD patients in our study. Blast exposure may induce mild traumatic brain injury, which has been suggested to increase vulnerability to develop PTSD and potentially reinforces PTSD symptoms (Bazarian et al, 2013; Costanzo et al, 2014). However, mild traumatic brain injury has been related to white matter lesions and reductions in white matter microstructure integrity (Bazarian et al, 2013). As we found higher FA values in our persistent PTSD patients after treatment, it is unlikely that blast exposure affects our results. Post hoc analyses excluding participants with blast exposure yielded similar results (see Supplementary Material). Future studies should further investigate the contributing effects of blast exposure to PTSD symptoms.
This study has some limitations. First, we included a small number of PTSD patients currently taking medication, and a number of patients (in particular persistent PTSD patients) had comorbid disorders. However, this is representative for PTSD (Brady et al, 2000), and makes our results more generalizable. Post hoc correlations between change in FA values and comorbidity only revealed a correlation between change in fornix FA and baseline comorbidity within the persistent PTSD group, indicating that (only) this tract may be influenced by comorbidity. Treatment type was not randomised, but represented treatment as usual. No differences in the number of EMDR vs TFCBT sessions were present between groups. In addition, there were no correlations within the groups between number of EMDR or TFCBT sessions with CAPS improvement, or with differences in tract FA values. Therefore, it is not expected that the type of treatment influenced our results. Furthermore, our remitted and persistent PTSD group differed in initial symptom severity, which may confound our results. However, there were no correlations between baseline CAPS scores and tract FA values within the PTSD group, and it is therefore not expected that the difference in baseline CAPS scores directly influenced the results. Although it could be argued that the persistent PTSD group represents a more ‘complex’ PTSD group (more comorbidity and severity), and is therefore more treatment resistant (Morina et al, 2013). Hence, when studying PTSD treatment, comorbidity, medication, and higher symptom severity will generally be confounding factors in these studies, when not used as exclusion criteria. To address the effects of these factors in treatment response, large-scale studies need to be performed to understand the heterogeneity within PTSD and in treatment response.
In summary, we observed differences in white matter microstructure of the dorsal cingulum between patients with persistent PTSD and patients with remitted PTSD and combat controls at reassessment. In the persistent PTSD patients, dorsal cingulum FA increased over time. Treatment may be accompanied with white matter microstructure changes of the left hippocampal cingulum bundle, stria terminalis, fornix, posterior corona radiata, and superior longitudinal fasciculus, but the interaction patterns observed need to be replicated. In addition, future studies should investigate recently traumatized subjects longitudinally to determine whether dorsal cingulum differences develop before the onset of PTSD (vulnerability factor) or are acquired after onset. This study provides first steps to help in a better understanding of the neural underpinnings of PTSD and identifying potential markers of treatment resistance can help to develop targeted treatments for these persistent PTSD patients.
Funding and Disclosure
This research was funded by the Dutch Ministry of Defence. Dr Kalin has served on scientific advisory boards for Corcept Therapeutics, Neuronetics, CeNeRx BioPharma, and Skyland Trail; is a stockholder with equity options in Corcept Therapeutics and CeNeRx BioPharma; owned Promoter Neurosciences; and holds patents for promoter sequences for corticotropin-releasing factor CRF2α and a method of identifying agents that alter the activity of the promoter sequences, promoter sequences for urocortin II and the use thereof, and promoter sequences for corticotropin-releasing factor binding protein and the use thereof. The authors declare no conflict of interest.
References
Abe O, Yamasue H, Kasai K, Yamada H, Aoki S, Iwanami et al (2006). Voxel-based diffusion tensor analysis reveals aberrant anterior cingulum integrity in posttraumatic stress disorder due to terrorism. Psychiatry Res Neuroimag 146: 231–242.
Alexander AL, Hurley SA, Samsonov AA, Adluru N, Hosseinbor AP, Mossahebi P et al (2011). Characterization of cerebral white matter properties using quantitative magnetic resonance imaging stains. Brain Connect 1: 423–446.
American Psychiatric Association (1994). Diagnostic and Statistical Manual of Mental Disorders. 4th edn. American Psychiatric Association: Washington, DC.
Aupperle RL, Allard CB, Simmons AN, Flagan T, Thorp SR, Norman SB et al (2013). Neural responses during emotional processing before and after cognitive trauma therapy for battered women. Psychiatry Res Neuroimag 214: 48–55.
Avery SN, Clauss JA, Winder DG, Woodward N, Heckers S, Blackford JU (2014). BNST neurocircuitry in humans. NeuroImage 91: 311–323.
Balkom AV, Vliet IV, Emmelkamp P, Bockting C, Spijker J, Hermens M, Meeuwissen J, namens de Werkgroep Multidisciplinaire richtlijnontwikkelingAngststoornissen/Depressie (2013). Multidisciplinaire richtlijn Angststoornissen (Derde revisie). Richtlijn voor de diagnostiek, behandeling en begeleiding van volwassen patiënten met een angststoornis. Trimbos-instituut: Utrecht, The Netherlands.
Bazarian JJ, Donnelly K, Peterson DR, Warner GC, Zhu T, Zhong J (2013). The relation between posttraumatic stress disorder and mild traumatic brain injury acquired during operations enduring freedom and iraqi freedom. J Head Trauma Rehab 28: 1–12.
Beaulieu C (2009). The biological basis of diffusion anisotropy. Diffus MRI 15: 105–126.
Bisson JI, Ehlers A, Matthews R, Pilling S, Richards D, Turner S (2007). Psychological treatments for chronic post-traumatic stress disorder: systematic review and meta-analysis. Br J Psychiatry 190: 97–104.
Blake DD, Weathers FW, Nagy LM, Kaloupek DG, Gusman FD, Charney DS et al (1995). The development of a clinician-administered PTSD scale. J Traum Stress 8: 75–90.
Bluhm RL, Williamson PC, Osuch EA, Frewen PA, Stevens TK, Boksman K et al (2009). Alterations in default network connectivity in posttraumatic stress disorder related to early-life trauma. J Psychiatry Neurosci 34: 187–194.
Brady K, Pearlstein T, Asnis GM, Baker D, Rothbaum B, Sikes CR et al (2000). Efficacy and safety of sertraline treatment of posttraumatic stress disorder: a randomized controlled trial. J Am Med Assoc 283: 1837–1844.
Bryant RA, Felmingham K, Kemp A, Das P, Hughes G, Peduto A et al (2008). Amygdala and ventral anterior cingulate activation predicts treatment response to cognitive behaviour therapy for post-traumatic stress disorder. Psychol Med 38: 555–561.
Bryant RA, Felmingham K, Whitford TJ, Kemp A, Hughes G, Peduto A et al (2008). Rostral anterior cingulate volume predicts treatment response to cognitive-behavioural therapy for posttraumatic stress disorder. J Psychiatry Neurosci 33: 142–146.
Concha L (2014). A macroscopic view of microstructure: using diffusion-weighted images to infer damage, repair, and plasticity of white matter. Neuroscience 276: 14–28.
Costanzo ME, Chou Y-, Leaman S, Pham DL, Keyser D, Nathan DE et al (2014). Connecting combat-related mild traumatic brain injury with posttraumatic stress disorder symptoms through brain imaging. Neurosci Lett 577: 11–15.
Daniels JK, Lamke J-, Gaebler M, Walter H, Scheel M (2013). White matter integrity and its relationship to PTSD and childhood trauma—a systematic review and meta-analysis. Depress Anxiety 30: 207–216.
Daniels JK, Mcfarlane AC, Bluhm RL, Moores KA, Richard Clark C, Shaw ME et al (2010). Switching between executive and default mode networks in posttraumatic stress disorder: alterations in functional connectivity. J Psychiatry Neurosci 35: 258–266.
Dickie EW, Brunet A, Akerib V, Armony JL (2013). Anterior cingulate cortical thickness is a stable predictor of recovery from post-traumatic stress disorder. Psychol Med 43: 645–653.
Ding AY, Li Q, Zhou IY, Ma SJ, Tong G, McAlonan GM et al (2013). MR diffusion tensor imaging detects rapid microstructural changes in amygdala and hippocampus following fear conditioning in mice. PLoS One 8: e51704.
Fani N, Ashraf A, Afzal N, Jawed F, Kitayama N, Reed L et al (2011). Increased neural response to trauma scripts in posttraumatic stress disorder following paroxetine treatment: a pilot study. Neurosci Lett 491: 196–201.
Fani N, King TZ, Jovanovic T, Glover EM, Bradley B, Choi K et al (2012). White matter integrity in highly traumatized adults with and without post-traumatic stress disorder. Neuropsychopharmacology 37: 2740–2746.
First MB, Spitzer RL, Gibbon M, Williams JBW (1997) Structured Clinical Interview for DSM-IV Axis I Disorders SCID-I. Clinician Version (Administration Booklet).
Foa EB, Kozak MJ (1986). Emotional processing of fear. Exposure to corrective information. Psychol Bull 99: 20–35.
Foa EB, Meadows EA (1997). Psychosocial treatments for posttraumatic stress disorder: a critical review. Annu Rev Psychol 48: 449–480.
Gray JA (1982). The neuropsychology of anxiety: an enquiry into the functions of the septo-hippocampal system. Neuropsychol Anxiety.
Hayes JP, Hayes SM, Mikedis AM (2012). Quantitative meta-analysis of neural activity in posttraumatic stress disorder. Biol Mood Anxiety Disord 2: 9–5380-2-9.
Henkelman RM, Stanisz GJ, Graham SJ (2001). Magnetization transfer in MRI: a review. NMR Biomed 14: 57–64.
Hoge CW, Castro CA, Messer SC, McGurk D, Cotting DI, Koffman RL (2004). Combat duty in Iraq and Afghanistan, mental health problems, and barriers to care. N Engl J Med 351: 13–22.
Kennis M, Rademaker AR, van Rooij SJ, Kahn RS, Geuze E (2014). Resting state functional connectivity of the anterior cingulate cortex in veterans with and without post-traumatic stress disorder. Hum Brain Mapp 36: 99–109.
Kim MJ, Lyoo IK, Kim SJ, Sim M, Kim N, Choi N et al (2005). Disrupted white matter tract integrity of anterior cingulate in trauma survivors. NeuroReport 16: 1049–1053.
Lanius RA, Williamson PC, Hopper J, Densmore M, Boksman K, Gupta MA et al (2003). Recall of emotional states in posttraumatic stress disorder: an fMRI investigation. Biol Psychiatry 53: 204–210.
Lindauer RJJ, Vlieger E, Jalink M, Olff M, Carlier IV, Majoie CB et al (2005). Effects of psychotherapy on hippocampal volume in out-patients with post-traumatic stress disorder: a MRI investigation. Psychol Med 35: 1421–1431.
Linden DEJ (2006). How psychotherapy changes the brain—the contribution of functional neuroimaging. Mol Psychiatry 11: 528–538.
Mori S, Oishi K, Jiang H, Jiang L, Li X, Akhter K et al (2008). Stereotaxic white matter atlas based on diffusion tensor imaging in an ICBM template. NeuroImage 40: 570–582.
Mori S, Wakana S, Nagae-Poetscher LM, van Zijl PC (2005) MRI Atlas of Human White Matter. Elsevier: Amsterdam, The Netherlands.
Morina N, Ajdukovic D, Bogic M, Franciskovic T, Kucukalic A, Lecic-Tosevski D et al (2013). Co-occurrence of major depressive episode and posttraumatic stress disorder among survivors of war: How is it different from either condition alone? J Clin Psychiatry 74: e212–e218.
Philip NS, Sweet LH, Tyrka AR, Price LH, Bloom RF, Carpenter LL (2013). Decreased default network connectivity is associated with early life stress in medication-free healthy adults. Eur Neuropsychopharmacol 23: 24–32.
Rauch SL, Shin LM, Phelps EA (2006). Neurocircuitry models of posttraumatic stress disorder and extinction: human neuroimaging research—past, present, and future. Biol Psychiatry 60: 376–382.
Reijnen A, Rademaker AR, Vermetten E, Geuze E (2014). Prevalence of mental health symptoms in Dutch military personnel returning from deployment to Afghanistan: a 2-year longitudinal analysis. Eur Psychiatry 30: 341–346.
Rothbaum BO, Davis M (2003). Applying learning principles to the treatment of post-trauma reactions. Ann NY Acad Sci 1008: 112–121.
Roy MJ, Francis J, Friedlander J, Banks-Williams L, Lande RG, Taylor P et al (2010). Improvement in cerebral function with treatment of posttraumatic stress disorder. Ann NY Acad Sci 1208: 142–149.
Sanjuan PM, Thoma R, Claus ED, Mays N, Caprihan A (2013). Reduced white matter integrity in the cingulum and anterior corona radiata in posttraumatic stress disorder in male combat veterans: a diffusion tensor imaging study. Psychiatry Res Neuroimag 214: 260–268.
Schuff N, Zhang Y, Zhan W, Lenoci M, Ching C, Boreta L et al (2011). Patterns of altered cortical perfusion and diminished subcortical integrity in posttraumatic stress disorder: an MRI study. NeuroImage 54: S62–S68.
Sekiguchi A, Sugiura M, Taki Y, Kotozaki Y, Nouchi R, Takeuchi H et al (2014). White matter microstructural changes as vulnerability factors and acquired signs of post-earthquake distress. PLoS One 9: e83967.
Smith SM, Nichols TE (2009). Threshold-free cluster enhancement: addressing problems of smoothing, threshold dependence and localisation in cluster inference. NeuroImage 44: 83–98.
van Rooij S, Geuze E, Kennis M, Rademaker A, Vink M (2014). Neural correlates of inhibition and contextual cue processing related to treatment response in PTSD. Neuropsychopharmacology 40: 667–675.
van Rooij SJH, Kennis M, Vink M, Kahn RS, Geuze E (2015). Predicting persistence of PTSD: A longitudinal functional MRI study on trauma-unrelated emotional processing (in preparation).
Van Wingen GA, Geuze E, Caan MWA, Kozicz T, Olabarriaga SD, Denys D et al (2012). Persistent and reversible consequences of combat stress on the mesofrontal circuit and cognition. Proc Natl Acad Sci USA 109: 15508–15513.
Wang S, Young KM (2014). White matter plasticity in adulthood. Neuroscience 276: 148–160.
World Medical Association (2013). Declaration of Helsinki: ethical principles for medical research involving human subjects. JAMA 310: 2191–2194.
Zhang L, Li W, Shu N, Zheng H, Zhang Z, Zhang Y et al (2012). Increased white matter integrity of posterior cingulate gyrus in the evolution of post-traumatic stress disorder. Acta Neuropsychiatr 24: 34–42.
Zhang L, Zhang Y, Li L, Li Z, Li W, Ma N et al (2011). Different white matter abnormalities between the first-episode, treatment-naive patients with posttraumatic stress disorder and generalized anxiety disorder without comorbid conditions. J Affect Disord 133: 294–299.
Acknowledgements
We thank Alieke Reijnen for her valuable suggestions.
Author information
Authors and Affiliations
Corresponding author
Additional information
Supplementary Information accompanies the paper on the Neuropsychopharmacology website
Supplementary information
Rights and permissions
About this article
Cite this article
Kennis, M., van Rooij, S., Tromp, D. et al. Treatment Outcome-Related White Matter Differences in Veterans with Posttraumatic Stress Disorder. Neuropsychopharmacol 40, 2434–2442 (2015). https://doi.org/10.1038/npp.2015.94
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/npp.2015.94
This article is cited by
-
Internal capsule microstructure mediates the relationship between childhood maltreatment and PTSD following adulthood trauma exposure
Molecular Psychiatry (2023)
-
Microstructural Differences of the Cerebellum-Thalamus-Basal Ganglia-Limbic Cortex in Patients with Somatic Symptom Disorders: a Diffusion Kurtosis Imaging Study
The Cerebellum (2022)
-
White matter anisotropy and response to cognitive behavior therapy for posttraumatic stress disorder
Translational Psychiatry (2021)
-
Sex-specific and shared expression profiles of vulnerability and resilience to trauma in brain and blood
Biology of Sex Differences (2020)
-
White matter microstructure varies with post-traumatic stress severity following medical trauma
Brain Imaging and Behavior (2020)