Abstract
Celiac disease is common and can present with nonspecific upper gastrointestinal symptoms. Patients may therefore undergo esophagogastroduodenoscopy as their initial investigation. Markers of villous atrophy, which can be seen in the duodenum during endoscopy, are well described. They have limited sensitivity for patients with mild enteropathy and duodenal biopsies should be performed if there is strong suspicion of celiac disease irrespective of endoscopic appearance. Endoscopic markers do, however, allow the selection of patients with nonspecific symptoms for duodenal biopsy, and these markers should, therefore, be looked for routinely during esophagogastroduodenoscopy.
Key Points
-
Celiac disease is common and can present with upper gastrointestinal symptoms rather than malabsorption
-
Esophagogastroduodenoscopy might be the first investigation ordered in patients with celiac disease
-
There are well-defined markers of villous atrophy in the duodenum that should be routinely looked for during endoscopy
-
The absence of endoscopic markers should not preclude biopsy if celiac disease is strongly suspected, because the markers lack sensitivity, particularly for mild enteropathy
-
Endoscopic markers are useful in the selection of patients who have nonspecific upper gastrointestinal symptoms for biopsy
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$209.00 per year
only $17.42 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout


Similar content being viewed by others
References
Fasano A et al. (2003) Prevalence of celiac disease in at-risk and not-at-risk groups in the United States: a large multicenter study. Arch Intern Med 163: 286–292
United European Gastroenterology (2001) When is a coeliac a coeliac? Report of a working group of the United European Gastroenterology Week in Amsterdam, 2001. Eur J Gastroenterol Hepatol 13: 1123–1128
Saverymuttu SH et al. (1991) Impact of endoscopic duodenal biopsy on the detection of small intestinal villous atrophy. Postgrad Med J 67: 47–49
Marsh MN (1992) Gluten, major histocompatibility complex, and the small intestine. A molecular and immunobiologic approach to the spectrum of gluten sensitivity ('celiac sprue'). Gastroenterology 102: 330–354
Oberhuber G et al. (1999) The histopathology of coeliac disease: time for a standardized report scheme for pathologists. Eur J Gastroenterol Hepatol 11: 1185–1194
Dickey W and McMillan SA (2005) Increasing numbers at a specialist coeliac clinic: contribution of serological testing in primary care. Dig Liver Dis 37: 928–933
Dickey W and Bodkin S (1998) Prospective study of body mass index in coeliac disease. Br Med J 317: 1290
Fasano A and Catassi C (2001) Current approaches to diagnosis and treatment of celiac disease: an evolving spectrum. Gastroenterology 120: 636–651
Ciacci C et al. (1995) Gender and clinical presentation in adult celiac disease. Scand J Gastroenterol 30: 1077–1081
Usai P et al. (1995) Oesophageal motility in adult coeliac disease. Neurogastroenterol Motil 7: 239–244
Cuomo A et al. (2003) Reflux oesophagitis in adult coeliac disease: beneficial effect of a gluten free diet. Gut 52: 514–517
Maieron R et al. (2005) Celiac disease and intestinal metaplasia of the esophagus (Barrett's esophagus). Dig Dis Sci 50: 126–129
Bassotti G et al. (1994) Abnormal gastrointestinal motility in patients with celiac sprue. Dig Dis Sci 39: 1947–1954
Iovino P et al. (1998) Esophageal impairment in adult celiac disease with steatorrhea. Am J Gastroenterol 93: 1243–1249
Usai P et al. (1997) Autonomic dysfunction and upper digestive functional disorders in untreated adult coeliac disease. Eur J Clin Invest 27: 1009–1015
Bardella et al. (2000) Gastric emptying and plama neurotensin levels in untreated celiac patients. Scan J Gastroenterol 35: 269–273
Kilander AF et al. (1984) Plasma enteroglucagon related to malabsorption in coeliac disease. Gut 25: 629–635
Wahab PJ et al. (2001) Basal and fat-stimulated plasma peptide YY levels in celiac disease. Dig Dis Sci 46: 2504–2509
Giorgetti GM et al. (2004) Assessment of autonomic function in untreated adult coeliac disease. World J Gastroenterol 10: 2715–2718
Dickey W and Hughes DF (2004) Erosions of the second part of duodenum in patients with villous atrophy. Gastrointest Endosc 59: 116–118
Brocchi E et al. (2002) Endoscopic markers in adult coeliac disease. Dig Liver Dis 34: 177–182
Brocchi E et al. (1998) Endoscopic demonstration of loss of duodenal folds in the diagnosis of celiac disease. N Engl J Med 319: 741–744
McIntyre AS et al. (1992) The endoscopic appearance of duodenal folds is predictive of untreated adult celiac disease. Gastrointest Endosc 38: 148–151
Maurino E et al. (1993) Value of endoscopic markers in celiac disease. Dig Dis Sci 38: 2028–2033
Dickey W and Hughes DF (2001) Disappointing sensitivity of endoscopic markers for villous atrophy in a high-risk population: implications for celiac disease diagnosis during routine endoscopy. Am J Gastroenterol 96: 2126–2128
Oxentenko AS et al. (2002) The insensitivity of endoscopic markers in celiac disease. Gastrointest Endosc 97: 933–938
Lecleire S et al. (2006) Endoscopic markers of villous atrophy are not useful for the detection of celiac disease in patients with dyspeptic symptoms. Endoscopy 38: 696–701
Culliford A et al. (2004) Scalloping of duodenal mucosa in Crohn's disease. Inflamm Bowel Dis 10: 270–273
Shah VH et al. (2000) All that scallops is not celiac disease. Gastrointest Endosc 51: 717–720
Luzi G et al. (2003) Duodenal pathology and clinical–immunological implications in common variable immunodeficiency patients Am J Gastroenterol 98: 118–121
Dickey W (2002) Low serum B12 is common in coeliac disease and is not due to autoimmune gastritis. Eur J Gastroenterol Hepatol 14: 425–427
Mahmud FH et al. (2005) Celiac disease in type 1 diabetes mellitus in a North American community: prevalence, serologic screening, and clinical features. Mayo Clin Proc 80: 1429–1434
Ch'ng CL et al. (2005) Prospective screening for coeliac disease in patients with Graves' hyperthyroidism using anti-gliadin and tissue transglutaminase antibodies. Clin Endocrinol 62: 303–306
Green PHR and Murray J (2003) Routine duodenal biopsies to exclude celiac disease? Gastrointest Endosc 58: 92–95
Dickey W and Hughes D (1999) Prevalence of celiac disease and its endoscopic markers among patients having routine upper gastrointestinal endoscopy. Am J Gastroenterol 94: 2182–2186
Bardella MT et al. (2000) Reevaluation of duodenal endoscopic markers in the diagnosis of celiac disease. Gastrointest Endosc 51: 714–716
Collin P et al. (2002) The hunt for coeliac disease in primary care. Q J Med 95: 75–77
Dickey W (1998) Diagnosis of coeliac disease at open-access endoscopy. Scand J Gastroenterol 33: 612–615
Vjero K et al. (2003) Defining a proper setting for endoscopy in coeliac disease. Eur J Gastroentero Hepatol 15: 675–678
Stevens FM and McCarthy CF (1976) The endoscopic demonstration of coeliac disease. Endoscopy 8: 177–180
Niveloni S et al. (1998) Usefulness of videoduodenoscopy and vital dye staining as indicators of mucosal atrophy of celiac disease: assessment of interobserver agreement. Gastrointest Endosc 47: 223–229
Siegel LM et al. (1997) Combined magnification endoscopy with chromoendoscopy in the evaluation of patients with suspected malabsorption. Gastrointest Endosc 46: 226–230
Cammarota G et al. (2004) Reliability of the “immersion technique” during routine upper endoscopy for detection of abnormalities of duodenal villi in patients with dyspepsia. Gastrointest Endosc 60: 223–228
Cammarota G et al. (2004) Direct visualization of intestinal villi by high-resolution magnifying upper endoscopy: a validation study. Gastrointest Endosc 60: 732–738
Badreldin R et al. (2005) How good is zoom endoscopy for assessment of villous atrophy in coeliac disease? Endoscopy 37: 994–998
Cammarota G et al. (2006) High accuracy and cost-effectiveness of a biopsy-avoiding endoscopic approach in diagnosing coeliac disease. Aliment Pharm Ther 23: 61–69
Cellier C et al. (2005) ICCE consensus for celiac disease. Endoscopy 37: 1055–1059
Culliford A et al. (2005) The value of wireless capsule endoscopy in patients with complicated celiac disease. Gastrointest Endosc 62: 55–61
Pertroniene E et al. (2005) Given capsule endoscopy in celiac disease: evaluation of diagnostic atrophy and interobserver agreement. Am J Gastroenterol 100: 685–694
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The author declares no competing financial interests.
Rights and permissions
About this article
Cite this article
Dickey, W. Endoscopic markers for celiac disease. Nat Rev Gastroenterol Hepatol 3, 546–551 (2006). https://doi.org/10.1038/ncpgasthep0601
Received:
Accepted:
Issue Date:
DOI: https://doi.org/10.1038/ncpgasthep0601
This article is cited by
-
Anti-tissue transglutaminase titers are associated with endoscopic findings and severity of mucosal damage in children with celiac disease
European Journal of Pediatrics (2021)
-
A Caucasian American patient with celiac disease diagnosed in Japan and successfully treated with a gluten-free diet
Clinical Journal of Gastroenterology (2018)
-
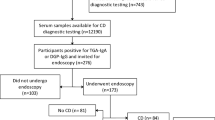
‘Pre-endoscopy point of care test (Simtomax- IgA/IgG-Deamidated Gliadin Peptide) for coeliac disease in iron deficiency anaemia: diagnostic accuracy and a cost saving economic model’
BMC Gastroenterology (2016)
-
Celiac disease in the elderly
Nature Clinical Practice Gastroenterology & Hepatology (2008)