Abstract
Background Coronary allograft vasculopathy is a severe complication of heart transplantation. We used virtual histology intravascular ultrasound to characterize plaque burden and tissue composition over time in heart transplant recipients.
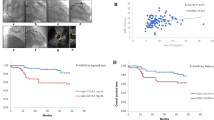
Methods We recruited patients undergoing heart transplantation in four centers in Europe and the US between 2004 and 2006. We used intravascular ultrasound to obtain morphological plaque measurements and to perform virtual histology in the left anterior descending coronary artery. Data were characterized according to the duration between transplantation and intravascular ultrasound assessment: ≤24, >24–60, >60–120 and >120–192 months.
Results We assessed vessels from 152 patients (mean age 58 ± 12 years) a mean of 70 ± 53 months (range 1 week to 16 years) after transplantation. Plaque burden of >40% was observed in 26% of vessels analyzed, with increases from baseline being seen in all time categories. If assessed >24 months after transplantation, necrotic core and dense calcified volumes were significantly greater than at baseline (P = 0.0005 and P = 0.01, respectively). Time since heart transplantation and donor age and recipient age were independent predictive factors of increased necrotic core content. Necrotic core volume >2.01 mm3, diabetes mellitus, donor age older than 40 years, follow-up from transplantation longer than 5 years and recipient age older than 58 years were associated with the need for revascularization.
Conclusions In coronary allograft vasculopathy, plaque burden and composition change over time and seem to affect clinical outcome. This relationship might facilitate identification of high-risk patients in whom the value of more aggressive medical therapy should be tested.
Key Points
-
Time-dependent increases in the necrotic core content of plaques occur in patients with coronary allograft vasculopathy
-
Necrotic core content was increased in patients whose heart came from a donor older than 58 years
-
Patients who had plaques with large necrotic cores were at risk of needing coronary revascularization
-
Identification of clinical factors that can affect plaque volume and plaque composition could help to identify patients at increased risk of rapidly developing vasculopathy; the value of aggressive therapy for these patients should be tested
-
The beneficial effects of newer immunosuppressive or anti-inflammatory therapies that might reduce development of coronary allograft vasculopathy or stabilize plaque composition could be evaluated by sequential virtual histology ultrasonography
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$209.00 per year
only $17.42 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout




Similar content being viewed by others
References
Pascoe LA et al. (1987) The prevalence of cardiac allograft arteriosclerosis. Transplantation 44: 838–839
Mullins PA et al. (1992) Coronary occlusive disease and late graft failure after cardiac transplantation. Br Heart J 68: 260–265
Johnson DE et al. (1989) The spectrum of coronary artery pathologic findings in human cardiac allografts. J Heart Lung Transplant 8: 349–359
Uretsky BF et al. (1987) Development of coronary artery disease in cardiac transplant patients receiving immunosuppressive therapy with cyclosporine and prednisone. Circulation 76: 827–834
Tuzcu EM et al. (1996) Dichotomous pattern of coronary atherosclerosis 1 to 9 years after transplantation: insights from systematic intravascular ultrasound imaging. J Am Coll Cardiol 27: 839–846
Tsutsui H et al. (2001) Lumen loss in transplant coronary artery disease is a biphasic process involving early intimal thickening and late constrictive remodeling: results from a 5-year serial intravascular ultrasound study. Circulation 104: 653–657
Escobar A et al. (1994) Cardiac allograft vasculopathy assessed by intravascular ultrasonography and nonimmunologic risk factors. Am J Cardiol 74: 1042–1046
Costanzo-Nordin MR (1992) Cardiac allograft vasculopathy: relationship with acute cellular rejection and histocompatibility. J Heart Lung Transplant 11: S90–S103
Kemna MS et al. (1994) Metabolic risk factors for atherosclerosis in heart transplant recipients. Am Heart J 128: 68–72
Esper E et al. (1997) Role of hypercholesterolemia in accelerated transplant coronary vasculopathy: results of surgical therapy with partial ileal bypass in rabbits undergoing heterotopic heart transplantation. J Heart Lung Transplant 16: 420–435
Hoang K et al. (1998) Diabetes and dyslipidemia. A new model for transplant coronary artery disease. Circulation 97: 2160–2168
Bae JH et al. (2006) Association of angiotensin-converting enzyme inhibitors and serum lipids with plaque regression in cardiac allograft vasculopathy. Transplantation 82: 1108–1111
Kapadia SR et al. (2001) Impact of lipid abnormalities in development and progression of transplant coronary disease: A serial intravascular ultrasound study. J Am Coll Cardiol 38: 206–213
Fateh-Moghadam S et al. (2003) Cytomegalovirus infection status predicts progression of heart-transplant vasculopathy. Transplantation 76: 1470–1474
Costanzo MR et al. (1998) Heart transplant coronary artery disease detected by coronary angiography: a multiinstitutional study of preoperative donor and recipient risk factors: Cardiac Transplant Research Database. J Heart Lung Transplant 17: 744–753
Rahmani M et al. (2006) Allograft vasculopathy versus atherosclerosis. Circ Res 99: 801–815
O'Neill BJ et al. (1989) Frequency of angiographic detection and quantitative assessment of coronary arterial disease one and three years after cardiac transplantation. Am J Cardiol 63: 1221–1226
Veinot JP et al. (1995) Angiographic underestimation of coronary artery disease in a cardiac transplant donor. Can J Cardiol 11: 1039–1042
Taylor DO et al. (2005) Registry of the International Society for Heart and Lung Transplantation: twenty-second official adult heart transplant report—2005. J Heart Lung Transplant 24: 945–955
Palmer ND et al. (1999) In vitro analysis of coronary atheromatous lesions by intravascular ultrasound. Reproducibility and histological correlation of lesion morphology. Eur Heart J 20: 1701–1706
Peters RJ et al. (1994) Histopathologic validation of intracoronary ultrasound imaging. J Am Soc Echocardiogr 7: 230–241
Glagov S et al. (1987) Compensatory enlargement of human atherosclerotic coronary arteries. N Engl J Med 316: 1371–1375
Rodriguez-Granillo GA et al. (2005) In vivo intravascular ultrasound-derived thin-cap fibroatheroma detection using ultrasound radiofrequency data analysis. J Am Coll Cardiol 46: 2038–2042
Nair A et al. (2002) Coronary plaque classification with intravascular ultrasound radiofrequency data analysis. Circulation 106: 2200–2206
Nair A et al. (2007) Automated coronary plaque characterization with intravascular ultrasound backscatter: ex-vivo validation. EuroIntervention 3: 113–120
Irshad K et al. (2007) Virtual histology intravascular ultrasound in carotid interventions. J Endovasc Ther 14: 198–207
Diethrich E et al. (2007) CAPITAL; First in vivo classification of high risk plaque types in carotid lesions. J Endovascular Therapy 14: 676–686
JMP[registered trademark] software version 7.0 (SAS Institute, Cary, NC, USA)
Hertz MI et al. (2002) The registry of the international society for heart and lung transplantation: nineteenth official report-2002. J Heart Lung Transplant 21: 950–970
Olivari MT et al. (1989) Arterial hypertension in heart transplant recipients treated with triple-drug immunosuppressive therapy. J Heart Transplant 8: 34–39
Pethig K et al. (2000) Systemic inflammatory response in cardiac allograft vasculopathy: highly-sensitive C-reactive protein is associated with progressive luminal obstruction. Circulation 102 (19 Suppl 3): III233–III236
Hognestad A et al. (2003) Plasma C-reactive protein as a marker of cardiac allograft vasculopathy in heart transplant recipients. J Am Coll Cardiol 42: 477–482
Eisenberg MS et al. (2000) Elevated levels of plasma C-reactive protein are associated with decreased graft survival in cardiac transplant recipients. Circulation 102: 2100–2104
Raichlin ER et al. (2007) Systemic inflammation and metabolic syndrome in cardiac allograft vasculopathy. J Heart Lung Transplant 26: 826–833
Virmani R et al. (2000) Lessons from sudden coronary death: a comprehensive morphological classification scheme for atherosclerotic lesions. Arterioscler Thromb Vasc Biol 20: 1262–1275
Virmani R et al. (2006) Pathology of the vulnerable plaque. J Am Coll Cardiol 47: C13–C18
Davies MJ et al. (1993) Risk of thrombosis in human atherosclerotic plaques: role of extracellular lipid, macrophage, and smooth muscle cell content. Br Heart J 69: 377–381
Lietz K et al. (2004) Outcomes in cardiac transplant recipients using allografts from older donors versus mortality on the transplant waiting list. Implications for donor selection criteria. J Am Coll Cardiol 43: 1553–1561
Depré C et al. (1995) Is acoustic shadowing at intracoronary ultrasound always the maker of intramural calcium accumulation. Cathet Cardiovasc Diagn 36: 179–182
Sawada T et al. (2008) Feasibility of combined use of intravascular ultrasound radiofrequency data analysis and optical coherence tomography for detecting thin-cap fibroatheroma. Eur Heart J 29: 1136–1146
Eisen HJ et al. (2003) Everolimus for the prevention of allograft rejection and vasculopathy in cardiac-transplant recipients. N Engl J Med 349: 847–858
Acknowledgements
We thank Angela Richter, Volcano Therapeutics Corporation, for her relentless collaboration with the data collection and virtual histology intravascular ultrasound analysis, as well as Armelle Guenegou, Cardio3 Biosciences, Braine-l'Alleud, Belgium, and Isabel Decramer, Cardiovascular Center, Aalst, Belgium, for their expert assistance with the statistical analysis.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing financial interests.
Rights and permissions
About this article
Cite this article
Sarno, G., Lerman, A., Bae, JH. et al. Multicenter assessment of coronary allograft vasculopathy by intravascular ultrasound-derived analysis of plaque composition. Nat Rev Cardiol 6, 61–69 (2009). https://doi.org/10.1038/ncpcardio1410
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/ncpcardio1410
This article is cited by
-
Extra cellular matrix remodelling after heterotopic rat heart transplantation: gene expression profiling and involvement of ED-A+ fibronectin, alpha-smooth muscle actin and B+ tenascin-C in chronic cardiac allograft rejection
Histochemistry and Cell Biology (2010)
-
C-reactive protein and severity of coronary allograft vasculopathy
Nature Reviews Cardiology (2009)
-
Author's response to “C-reactive protein and severity of coronary allograft vasculopathy.”
Nature Reviews Cardiology (2009)