Abstract
Langerhans cell histiocytosis is characterized by a localized or systemic proliferation of Langerhans cells. BRAF mutations have been reported in 40–70% of cases and MAP2K1 mutations have been found in BRAF-negative cases, supporting that Langerhans cell histiocytosis is a true neoplasm, at least in mutated cases. In a small subset of patients, Langerhans cell histiocytosis is detected incidentally in a biopsy involved by lymphoma. These lesions are usually minute and rarely have been assessed for mutations. We assessed for BRAF and MAP2K1 mutations in seven cases of Langerhans cell histiocytosis detected incidentally in biopsies involved by lymphoma. We performed immunohistochemical analysis for phosphorylated (p)-ERK. There were four men and three women (median age, 54 years; range, 28–84). The biopsies included lymph nodes (n=6) and chest wall (n=1). The lymphomas included five classical Hodgkin lymphoma, one mantle cell lymphoma, and one angioimmunoblastic T-cell lymphoma. All cases were negative for BRAF V600E and MAP2K1 mutations. Nevertheless, three of seven cases showed ERK activation as shown by expression of p-ERK. We performed mutation analysis using a panel of 134 commonly mutated genes (including BRAF and MAP2K1) by next-generation sequencing on three cases, including two cases positive for p-ERK by immunohistochemistry. No mutations were detected in any of the three cases assessed. Six patients received therapy appropriate for their lymphoma. With a median follow-up of 21 months (range, 6–89), no patients developed disseminated or recurrent Langerhans cell histiocytosis. We conclude that lymphoma-associated Langerhans cell histiocytosis is a clinically benign process that is not associated with BRAF V600E or MAP2K1 mutations and, as suggested by others, the designation Langerhans cell hyperplasia may be more appropriate. Nevertheless, the expression of p-ERK in three cases suggests that the RAS–RAF–MAP2K–ERK pathway is activated, perhaps by non-mutational mechanisms induced by the presence of lymphoma or lymphoma–microenvironment interactions.
Similar content being viewed by others
Main
Langerhans cell histiocytosis is a rare disease characterized histologically by a proliferation of Langerhans cells admixed with eosinophils, lymphocytes, macrophages, and multinucleated giant cells, with or without eosinophilic abscesses or necrosis.1 Virtually any anatomic site can be involved by Langerhans cell histiocytosis, and the disease may present as a localized lesion or multiorgan disease. Prognosis is variable, correlating in part with extent of disease, but morphologic findings of Langerhans cell histiocytosis are identical in localized or multifocal disease and are not an indicator of prognosis. Because of its heterogeneous clinical manifestations and benign morphology, the reactive or neoplastic nature of Langerhans cell histiocytosis was controversial for over 50 years.2 However, in 1994 two independent groups showed that a subset of cases of Langerhans cell histiocytosis is monoclonal by using a human androgen receptor X-chromosome-inactivation assay.3, 4
In 2010, Badalian-Very et al described BRAF V600E mutation in 40–70% of cases of Langerhans cell histiocytosis5 supporting the interpretation that Langerhans cell histiocytosis is a neoplasm, at least in mutated cases. Similar findings also were reported by others.6, 7, 8, 9 BRAF is a member of the rapid accelerating fibrosarcoma (RAF) kinase family that is activated by RAS and RAS-coupled receptor tyrosine kinases. RAS–RAF-activated complexes transmit downstream signals to the mitogen-activated protein kinase (MAPK) cascade including MEK/ERK kinases via protein phosphorylation.10, 11, 12 The RAS–RAF–MAPK–ERK pathway is a key regulator involved in cell proliferation, growth, differentiation, and apoptosis by transmitting activating signals to several nuclear, cytoplasmic and cell membrane targets.10, 11 Subsequently, a subset of BRAF wild-type Langerhans cell histiocytosis cases (30–50%) were shown to carry mutations in the MAPK-kinase 1 (MAP2K1 or MEK1) gene, further implicating the oncogenic MAPK pathway signaling in Langerhans cell histiocytosis pathogenesis.13, 14 Most of these mutations cause constitutive activation of MAP2K1 and activation of the RAS–RAF–MAPK signaling cascade via ERK phosphorylation.13, 14 BRAF V600E and MAP2K1 mutations are not exclusively seen in Langerhans cell histiocytosis and also have been reported with variable frequency in other hematopoietic neoplasms, for example, hairy cell leukemia as well as non-hematopoietic malignancies including melanoma, papillary thyroid carcinoma, colorectal carcinoma, and glioneuronal tumors.10, 11, 12, 15, 16, 17, 18, 19, 20, 21, 22
In a small subset of patients, Langerhans cell histiocytosis has been identified as an incidental finding in biopsy specimens involved by lymphoma. Classical Hodgkin lymphoma is the most common associated lymphoma,23, 24, 25, 26 whereas only sporadic cases of other types of non-Hodgkin lymphoma associated with Langerhans cell histiocytosis are reported in the literature.23, 25, 27, 28, 29, 30 The relationship between Langerhans cell histiocytosis and concurrent lymphoma remains unknown. To our knowledge, there are no previous studies that have assessed the status of BRAF or MAP2K1 in cases of Langerhans cell histiocytosis associated with concurrent lymphomas.
In this study, we identified seven patients with concurrent Langerhans cell histiocytosis and lymphoma and assessed the Langerhans cell component for BRAF and MAP2K1 mutations.
Materials and methods
Study Group and Immunohistochemistry
The archives of the Department of Hematopathology at The University of Texas MD Anderson Cancer Center from January 2000 to December 2015 were searched for cases diagnosed as Langerhans cell histiocytosis associated with lymphoma involving the same biopsy specimen. Cases with available paraffin-embedded tissue blocks or unstained slides were selected. Clinical and laboratory data were retrieved from the electronic medical record. This study was conducted under an Institutional Review Board-approved protocol.
Routinely prepared hematoxylin–eosin stained slides for all cases were reviewed. Immunohistochemical studies were performed to confirm the diagnosis of lymphoma and Langerhans cell histiocytosis using antibodies specific for CD1a and CD21 (Leica Biosystem, Newcastle, UK); CD2, CD3, CD4, CD7, CD8, CD20, CD30, CD45/LCA, BCL-6, MUM1, and TIA-1 (DAKO, Carpinteria, CA, USA); CD5 and cyclin D1 (Labvision/Neomarkers, Fremont, CA, USA); CD10, CD23, and BCL-2 (Novocastra/Vision Biosystem, Benton Lane, Newcastle-upon-Tyne, UK); CD15 (Becton-Dickinson Biosciences, San Jose, CA, USA); PAX-5 (Transduction Labs, San Diego, CA, USA); CXCL-13 (R&D Systems, Minneapolis, MN, USA); S-100 protein (BioGenex, Fremont, CA, USA) and Langerin/CD207 (Novocastra Biosystem, Newcastle, UK). In situ hybridization for Epstein–Barr virus-encoded RNA (EBER) was also performed.
ERK Phosphorylation Analysis by Immunohistochemistry
The highly specific antibody phospho-p44/42 MAPK (Thr202/Tyr204) (D13.14.4E) p-ERK (dilution 1:300, Cell Signaling, Danvers, MA, USA) was used to assess for the presence of nuclear and cytoplasmic phosphorylated p44 and p42 MAPK (Erk1 and Erk2).
BRAF Mutation Analysis by Immunohistochemistry
The VE-1 antibody (dilution 1:50, Spring Bioscience, Pleasanton, CA, USA) was used to assess for cytoplasmic staining supportive of the presence of BRAF V600E mutation. The antibody is highly specific for this mutation as shown previously by Capper et al.31
BRAF Mutation Analysis by Pyrosequencing
A polymerase chain reaction (PCR)-based pyrosequencing assay for BRAF mutation analysis was employed. This assay was developed at our institution and covers mutation hotspots in exons 11 (codon 468) and 15 (codons 595–600).32 This assay was chosen because all BRAF mutations in Langerhans cell histiocytosis identified previously have been clustered in exons 11 or 15 of the gene and alter the kinase domain of the protein.33 The Langerhans cell histiocytosis lesion was microdissected from fixed, paraffin-embedded tissue sections (10 μm thick) and DNA was extracted and PCR amplified using either a forward primer, 5′-TCCTGTATCCCTCTCAGGCATAAGGTAA-3′, and a reverse biotinylated primer, 5′-biotin-CGAACAGTGAATATTCCTTTGAT-3′ (for codon 468 of exon 11), or a forward primer, 5′-CATAATGCTTGCTCTGATAGGA-3′, and a reverse biotinylated primer, 5′-biotin-GGCCAAAAATTTAATCAGTGGA-3′ (for codons 595–600 of exon 15). PCR amplification was performed in duplicate on an ABI 2720 Thermocycler (Applied Biosystems, Grand Island, NY, USA). The PCR products underwent electrophoresis on agarose gels to confirm successful amplification. Fifteen microliter of the PCR products were then sequenced in duplicate using primers 5′-TTGGATCTGGATCATTT-3′ (for exon 11) or 5′-GAAGACCTCACAGTAAAAATA-3′ (for exon 15) and the pyrosequencing PSQ96 HS System (Biotage AB, Uppsala, Sweden) according to the manufacturer’s instructions. The HL-60 cell line, negative for BRAF mutation, and A375, a melanoma cell line positive for BRAF mutation (exon 15 V600E), were used as negative and positive controls, respectively.
MAP2K1 Mutation Analysis
We performed Sanger sequencing to assess for mutations in exons 2 and 3 of MAP2K1. DNA was subjected to PCR using a pair of M13-tagged forward primer, 5′-TGTAAAACGACGGCCAGTAGTATGACTTGTGCTCCCCA-3′, and reverse primer, 5′-CAGGAAACAGCTATGACCTGGTCCCCAGGCTTCTAAGT-3′, for exon 2, and a pair of M13-tagged forward primer, 5′-TGTAAAACGACGGCCAGTCATAAAACCTCTCTTTCTTCCACC-3′, and reverse primer, 5′-CAGGAAACAGCTATGACCCCAGAGCCACCCAACTCTTA-3′, for exon 3, in a 50 μl reaction containing 10 ng DNA, 0.03 U/μl Go Taq polymerase (Promega, Madison, WI, USA), 0.2 μM each of forward and reverse primers, 2 mM MgCl2, 1 mM dNTP mix and 1x Go Taq buffer. The reaction mix was first heated to 95 °C for 10 min, then subjected to 40 cycles of 95 °C for 30 s, 60 °C for 30 s, and 72 °C for 30 s, followed by 72 °C for 7 min. The PCR products underwent electrophoresis to confirm successful amplification, were purified using Agencourt AMPure Kit (Beckman Coulter, Indianapolis, IN, USA), and sequenced using the same primer sets as shown above.
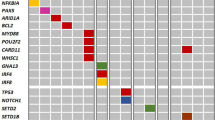
Next-Generation Sequencing
We performed amplicon-based next-generation sequencing targeting the coding regions of a panel of 134 genes that are commonly mutated in hematopoietic neoplasms using Torrent Suite platform (Thermo Fisher Scientific, Waltham, MA, USA) on DNA extracted from paraffin-embedded tissues. For two cases, we were able to retrieve tissues that were not involved by Langerhans cell histiocytosis to be used as a control. We used 20 ng of DNA to prepare the genomic library. The genes included in the panel are as follows: ABL1, ACVRL1, AKT1, ALK, APC, APEX1, AR, ARAF, ATM, ATP11B, BAP1, BCL2L1, BCL9, BIRC2, BIRC3, BRAF, BRCA1, BRCA2, BTK, CBL, CCND1, CCNE1, CD274, CD44, CDH1, CDK4, CDK6, CDKN2A, CHEK2, CSF1R, CSNK2A1, CTNNB1, DCUN1D1, DDR2, DNMT3A, EGFR, ERBB2, ERBB3, ERBB4, ESR1, EZH2, FBXW7, FGFR1, FGFR2, FGFR3, FGFR4, FLT3, FOXL2, GAS6, GATA2, GATA3, GNA11, GNAQ, GNAS, HNF1A, HRAS, IDH1, IDH2, IFITM1, IFITM3, IGF1R, IL6, JAK1, JAK2, JAK3, KDR, KIT, KNSTRN, KRAS, MAGOH, MAP2K1, MAP2K2, MAPK1, MAX, MCL1, MDM2, MDM4, MED12, MET, MLH1, MPL, MSH2, MTOR, MYC, MYCL, MYCN, MYD88, MYO18A, NF1, NF2, NFE2L2, NKX2-1, NKX2-8, NOTCH1, NPM1, NRAS, PAX5, PDCDILG2, PDGFRA, PIK3CA, PIK3R1, PNP, PPARG, PPP2R1A, PTCH1, PTEN, PTPN11, RAC1, RAF1, RB1, RET, RHEB, RHOA, RPS6KB1, SF3B1, SMAD4, SMARCB1, SMO, SOX2, SPOP, SRC, STAT3, STK11, TERT, TET2, TIAF1, TP53, TSC1, TSC2, U2AF1, VHL, WT1, XOP1, and ZNF217. Following successful library generation and purification, DNA was used for multiplex sequencing on the Ion Proton platform, and analyzed using the Torrent Suite and OncoSeek data pipeline.
Results
Clinical Features
The study group included seven patients, four men and three women, with a median age of 54 years (range, 28–84 years). The demographic, clinical, laboratory features at diagnosis, and pathology and molecular results are summarized in Table 1. One patient presented with mild leukocytosis (median white blood cell count, 5.6 × 103/μl; range, 4–13.2 × 103/μl; reference range, 4–11 × 103/μl); three patients had normocytic anemia (median hemoglobin, 13.3 g/dl; range, 9.8–16.2 g/dl; reference range, 14–18 g/dl for men and 12–16 g/dl for women), and one patient had thrombocytopenia (median platelet count, 158 × 103/μl; range, 41–368 × 103/μl; reference range, 140–440 × 103/μl). Serum lactate dehydrogenase was slightly elevated in one patient (median, 434 IU/l; range, 390–668 IU/l; reference range, 313–618 IU/l) and β2-microglobulin levels were elevated in five patients (median, 2.3 mg/l; range, 1.8–4.3 mg/l; reference range, 0.7–1.8 mg/l). Laboratory data were not available for one patient. The lymphomas include five cases of classical Hodgkin lymphoma and one case each of mantle cell lymphoma and angioimmunoblastic T-cell lymphoma. The cases of Hodgkin lymphoma were further classified as three nodular sclerosis, one mixed cellularity, and one recurrent disease. Concomitant Langerhans cell histiocytosis and lymphoma occurred in lymph nodes in six patients: three cervical, one axillary, one retroperitoneal, and one inguinal. In one patient a biopsy was obtained from the chest wall.
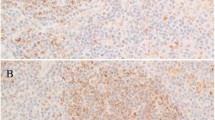
Morphologically, the lymphomas had pathologic and immunophenotypic findings that are typical of classical Hodgkin lymphoma (Figures 1 and 2), mantle cell lymphoma (Figure 3) and angioimmunoblastic T-cell lymphoma (Figure 4), and are not further discussed. In addition to the lymphomas, all biopsy specimens contained foci of Langerhans cell histiocytosis characterized by variable amounts of Langerhans cells with oval to folded nuclei with nuclear grooves, thin nuclear membranes, vesicular chromatin, inconspicuous nucleoli, and abundant pale to eosinophilic cytoplasm with ill-defined cell borders. The distribution of Langerhans cells was variable and ranged from a focal cluster of Langerhans cells to multiple foci of Langerhans cells intermingled intimately with lymphoma. Interspersed eosinophils, eosinophilic abscesses and areas of necrosis were observed variably (Figures 1–4). No cytologic atypia or increased mitotic activity was found in the Langerhans cell component in any case. Immunohistochemical stains for CD1a, langerin and S-100 were positive in the Langerhans cell component in all cases (Figures 1–4).
Langerhans cell histiocytosis and classical Hodgkin lymphoma, mixed cellularity (case 2). (a) Low power image of a lymph node involved by classical Hodgkin lymphoma, mixed cellularity type, and multiple clusters of Langerhans cell histiocytosis of variable sizes (arrows) (× 40). (b) Largest ill-defined nodule of Langerhans cell histiocytosis (× 200). (c) Area of transition of classical Hodgkin lymphoma with a Reed–Sternberg cell (left) and Langerhans cells (right) (× 400). (d) Immunostain for CD30 highlights the Reed–Sternberg cells and is negative in the Langerhans cells (× 400). (e). Immunostain for CD1a is positive in the Langerhans cells and is negative in the Reed–Sternberg cells (× 400). (f) BRAF is negative in both components (× 400).
Langerhans cell histiocytosis and classical Hodgkin lymphoma, nodular sclerosis (case 5). (a) The lymph node capsule is thickened and contains multiple fibrous bands extending into the parenchyma that incompletely surround cellular areas. In addition, the subcapsular region contains large clusters of Langerhans cells (arrows) (× 40). (b) Area of transition between classical Hodgkin lymphoma (top) and a nodule of Langerhans cells (bottom) (× 200). Immunostain for CD15 highlights the Reed–Sternberg cells (top) and is negative in the Langerhans cells (bottom) (× 200). (c) The widespread involvement of the lymph node by Langerhans cell histiocytosis is more evident with immunostain for CD1a (× 100). (d) Immunostain for BRAF is positive only in the Langerhans cell component with a weak cytoplasmic pattern of staining (× 100). Despite a positive BRAF V600E immunohistochemical result, BRAF pyrosequencing demonstrated a wild type sequence in codons 596 (GGT) and 600 (GTG). This case is negative for pERK by immunohistochemistry (inset, × 100).
Langerhans cell histiocytosis and mantle cell lymphoma (case 7). (a) The lymph node is replaced by a monotonous proliferation of small lymphocytes with focal sclerosis. A single nodule of Langerhans cells with central necrosis is identified at the center of the lymph node (× 100). (b) Left, mantle cell lymphoma composed of small lymphocytes with cleaved nuclei and perivascular fibrosis. Right, Langerhans cell module with scattered apoptotic cells (× 400). (c) Immunostain for CD1a is positive in the Langerhans cells and is negative in mantle cell lymphoma cells (× 400). (d) BRAF is negative in both components (× 400).
Langerhans cell histiocytosis and angioimmunoblastic T-cell lymphoma (case 1). (a) At low power, the lymph node is replaced by a diffuse lymphoproliferative process composed of small lymphocytes, clear cells and increased vascularity, characteristic of angioimmunoblastic T-cell lymphoma. A well circumscribed pale nodule of Langerhans cell histiocytosis (arrow) is present within the lymphomatous process (× 100). (b) At higher magnification, the paler nodule (left) is composed of Langerhans cells and scattered eosinophils (× 400). (c) By immunohistochemistry, the lymphoma cells are positive for CD3 and CD10 (× 200). (d) The Langerhans cell nodule is positive for CD1a (× 200). (e) BRAF is negative in both angioimmunoblastic T-cell lymphoma and Langerhans cell histiocytosis (× 200). (f) Immunostain with the anti-pERK antibody is positive in both the nucleus and cytoplasm of Langerhans cells (× 400).
Clinical follow-up data were available for six patients. Six patients received chemotherapy for the specific lymphoma (detailed chemotherapy regimens are listed in Table 1); two received additional radiation therapy, two underwent stem cell transplantation, and one patient is on the list in anticipation of a stem cell transplant. No patient received treatment specific for Langerhans cell histiocytosis. Treatment and outcome information were not available for one patient who was lost to follow-up. With a median follow-up of 21 months (range, 6–89 months), three patients remained in clinical remission for both Langerhans cell histiocytosis and lymphoma, one patient developed recurrent mediastinal lymphoma detected by imaging (biopsy not performed at the time of this study), one patient developed therapy-related myelodysplastic syndrome, and one patient died of Hodgkin lymphoma. No patient developed recurrent Langerhans cell histiocytosis.
BRAF and Phosphorylated ERK Immunohistochemical Assessment
The Langerhans cell component was negative for BRAF V600E mutant protein by immunohistochemistry in six of seven cases. The case of Langerhans cell histiocytosis positive for BRAF (case 5) is shown in Figure 2d. This result was performed twice with identical results.
The Langerhans cell component was positive for p-ERK by immunohistochemistry in three of seven cases (cases 1, 4, and 6). p-ERK expression was observed in the nucleus and cytoplasm of Langerhans cells (Figure 4f). In case 4, two small subcapsular Langerhans cell nodules were positive for p-ERK whereas the largest focus found in the mid portion of the lymph node was negative (not shown). In all cases, stromal cells, fibroblasts, and endothelial cells were positive for p-ERK (internal controls).
BRAF and MAP2K1 Mutation Analysis
None of the seven cases harbored a BRAF V600E or MAP2K1 mutation by PCR/pyrosequencing and PCR/Sanger sequencing, respectively.
Next-Generation Sequencing Results
To evaluate the discrepancy between immunohistochemistry and pyrosequencing for BRAF mutation on one case, and to explore the mutational status of the three cases positive for p-ERK, we performed next-generation sequencing analysis to assess mutation status of a panel of 134 genes that are commonly mutated in hematopoietic neoplasms, including ARAF, BRAF, ERBB1, ERBB2, ERBB3, KRAS, MAP2K1, NRAS, and PIK3CA, on three cases with DNA available. No mutations in any genes were detected in all three cases.
Discussion
We assessed the frequency of Langerhans cell histiocytosis-related mutations in biopsy specimens involved by Langerhans cell histiocytosis and lymphoma in seven patients. This form of Langerhans cell histiocytosis, usually microscopic and virtually always detected incidentally, is rare with most cases reported in the literature as case reports or small case series.23, 24, 25, 26, 27, 28, 29, 30 Most of these studies were published before the discovery of BRAF and MAP2K1 mutations in Langerhans cell histiocytosis, and therefore, as far as we are aware, this is the first study to assess BRAF V600E and MAP2K1 mutation status in the Langerhans cell component in cases with concomitant Langerhans cell histiocytosis and lymphoma.
Using molecular methods, we did not identify BRAF V600E or MAP2K1 mutations in the Langerhans cell lesions in this cohort. Nevertheless, we detected p-ERK by immunohistochemistry in three of seven cases consistent with activation of this pathway. Next-generation sequencing analysis for a panel of 134 genes (including ARAF, BRAF, ERBB1, ERBB2, ERBB3, KRAS, MAP2K1, NRAS, and PIK3CA) on two of these three cases failed to detect any mutation. These data, therefore, do not provide an explanation for the positive p-ERK results in these three cases. One possibility is that the sensitivity of the methods we employed is insufficient to detect mutations. In our opinion, this seems unlikely as the Langerhans cell histiocytosis lesions were microdissected and had well above 10% Langerhans cells in the specimen analyzed, the lower limit of sensitivity for the methods employed. We considered the possibility of non-V600E BRAF mutations, but the next-generation sequencing results in two cases did not support this idea. Nevertheless, in a recent study Chakraborty and colleagues performed whole-exome sequencing, targeted BRAF sequencing and/or whole-transcriptome sequencing (RNA-seq) on 24 patients with Langerhans cell histiocytosis lacking BRAF-V600E or MAP2K1 mutations, and identified in-frame BRAF deletions in the β3-αC loop in six cases and an in-frame FAM73A-BRAF fusion in one case.34 Whereas our methods can detect the in-frame deletions reported by Charkraborty et al, the methods used in our study cannot detect any gene fusion. Therefore, we cannot completely exclude the possibility of gene fusions involving BRAF, although the rarity of these fusions makes this possibility unlikely. It seems reasonable to suggest that the RAS/RAF/MAPK signaling pathway in some cases of incidental Langerhans cell histiocytosis may be activated by non-mutational mechanisms. Possibly, a local cytokine-mediated process imparting a growth advantage to Langerhans cells through activation of p-ERK might be involved, perhaps induced by the presence of lymphoma or a manifestation of lymphoma–microenvironmental interactions.
Using a commercially available monoclonal BRAF V600E specific antibody (VE-1), the results were negative in six cases of Langerhans cell histiocytosis, but positive in one case (case 5). The reason for the discrepancy between the immunohistochemistry result and molecular results in this case is uncertain. We used a pyrosequencing-based assay in all our cases to identify BRAF V600E mutation similar to most published studies.8, 35, 36 This case was also assessed by whole-exome sequencing and was negative for mutations involving 134 genes that included BRAF and MAP2K1. Furthermore, the BRAF antibody has been shown to have a high sensitivity and specificity for the BRAF mutation and represents an excellent tool for screening tissue samples.36 It is possible, however, that the BRAF V600E antibody uncommonly may yield false positive results. In a large study of colorectal carcinomas performed at our institution, Estrella and colleagues showed that 7 of 323 (2%) carcinomas shown to be wild type for BRAF V600E mutation by sequencing analysis were diffusely positive using the VE-1 antibody.37 It is important to mention that the case of Langerhans cell histiocytosis positive for BRAF V600E by immunohistochemistry was negative for p-ERK, indicating that that RAS/RAF/MAPK pathway was not active in this case.
The most frequent lymphoma associated with Langerhans cell histiocytosis in this case series was classical Hodgkin lymphoma, in accord with data reported in the literature.23, 24, 25, 26 To our knowledge, we report for the first time an association of Langerhans cell histiocytosis with mantle cell lymphoma and angioimmunoblastic T-cell lymphoma. In keeping with the literature, none of the six patients with follow-up data developed recurrent Langerhans cell histiocytosis or systemic Langerhans cell histiocytosis. This behavior, the often focal nature of the Langerhans cell component, and the absence of BRAF and MAP2K1 mutations suggest that Langerhans cell histiocytosis associated with lymphoma is a benign process, at least in most cases. For this reason, perhaps these lesions would be better designated as ‘Langerhans cell hyperplasia,’ as has been suggested by others.2, 23, 24, 25, 29 Christie et al and others have suggested that these lesions be designated as ‘Langerhans cells-like lesions.’29 Furthermore, some authors have suggested that this type of Langerhans cell lesion may be driven by chemokine/cytokine or other stimuli produced by the associated neoplastic conditions.2, 23, 24, 25, 29 This hypothesis could be the explanation for why classical Hodgkin lymphoma, a lymphoma that is characterized by the production of a storm of chemokines and cytokines, is the most common lymphoma with associated incidental Langerhans cell histiocytosis. Although this suggestion is reasonable for the concurrent findings of these two lesions, we do not have sufficient data to address this idea adequately.
In conclusion, we did not detect BRAF V600E or MAP2K1 mutations in all seven cases of Langerhans cell histiocytosis associated with lymphoma assessed. These data, combined with the small size of these lesions, their almost invariable incidental nature, and the absence of systemic Langerhans cell histiocytosis or recurrence, suggests that Langerhans cell histiocytosis associated with lymphoma is benign, as has been suggested by others. Nevertheless, p-ERK was positive in three of seven cases suggesting activation of the RAS/RAF/MAPK pathway in a subset of cases. Although the explanation for p-ERK activation is not entirely clear, it seems likely the activation of the pathway may occur via mechanisms unrelated to gene mutations, possibly induced by the presence of lymphoma.
References
Bechan GI, Egeler RM, Arceci RJ . Biology of Langerhans cells and Langerhans cell histiocytosis. Int Rev Cytol 2006; 254: 1–43.
Jaffe R . Langerhans cell histiocytosis and Langerhans cell sarcoma. In:Jaffe ES,Harris NL,Vardiman JWet al(eds).Hematopathology. Philadelphia: Elsevier, 2011, pp811–826.
Willman CL, Busque L, Griffith BB et al, Langerhans cell histiocytosis (histiocytosis X)—a clonal proliferative disease. N Engl J Med 1994; 331: 154–160.
Yu RC, Chu C, Buluwela L et al, Clonal proliferation of Langerhans cells in Langerhans cell histiocytosis. Lancet 1994; 343: 767–768.
Badalian-Very G, Vergilio JA, Degar BA et al, Recurrent BRAF mutations in Langerhans cell histiocytosis. Blood 2010; 116: 1919–1923.
Haroche J, Charlotte F, Arnaud L et al, High prevalence of BRAF V600E mutations in Erdheim-Chester disease but not in other non-Langerhans cell histiocytoses. Blood 2012; 120: 2700–2703.
Roden AC, Hu X, Kip S et al, BRAF V600E expression in Langerhans cell histiocytosis: clinical and immunohistochemical study on 25 pulmonary and 54 extrapulmonary cases. Am J Surg Pathol 2014; 38: 548–551.
Sahm F, Capper D, Preusser M et al, BRAFV600E mutant protein is expressed in cells of variable maturation in Langerhans cell histiocytosis. Blood 2012; 120: e28–e34.
Satoh T, Smith A, Sarde A et al, B-RAF mutant alleles associated with Langerhans cell histiocytosis, a granulomatous pediatric disease. PLoS One 2012; 7: e33891.
Montagut C, Settleman J . Targeting the RAF-MEK-ERK pathway in cancer therapy. Cancer Lett 2009; 283: 125–134.
Wellbrock C, Karasarides M, Marais R . The RAF proteins take centre stage. Nat Rev Mol Cell Biol 2004; 5: 875–885.
Young A, Lyons J, Miller AL et al, Ras signaling and therapies. Adv Cancer Res 2009; 102: 1–17.
Brown NA, Furtado LV, Betz BL et al, High prevalence of somatic MAP2K1 mutations in BRAF V600E-negative Langerhans cell histiocytosis. Blood 2014; 124: 1655–1658.
Chakraborty R, Hampton OA, Shen X et al, Mutually exclusive recurrent somatic mutations in MAP2K1 and BRAF support a central role for ERK activation in LCH pathogenesis. Blood 2014; 124: 3007–3015.
Greaves WO, Verma S, Patel KP et al, Frequency and spectrum of BRAF mutations in a retrospective, single-institution study of 1112 cases of melanoma. J Mol Diagn 2013; 15: 220–226.
Rahman MA, Salajegheh A, Smith RA et al, B-Raf mutation: a key player in molecular biology of cancer. Exp Mol Pathol 2013; 95: 336–342.
Tiacci E, Trifonov V, Schiavoni G et al, BRAF mutations in hairy-cell leukemia. N Engl J Med 2011; 364: 2305–2315.
Schindler G, Capper D, Meyer J et al, Analysis of BRAF V600E mutation in 1320 nervous system tumors reveals high mutation frequencies in pleomorphic xanthoastrocytoma, ganglioglioma and extra-cerebellar pilocytic astrocytoma. Acta Neuropathol 2011; 121: 397–405.
Marks JL, Gong Y, Chitale D et al, Novel MEK1 mutation identified by mutational analysis of epidermal growth factor receptor signaling pathway genes in lung adenocarcinoma. Cancer Res 2008; 68: 5524–5528.
Murugan AK, Dong J, Xie J, Xing M . MEK1 mutations, but not ERK2 mutations, occur in melanomas and colon carcinomas, but none in thyroid carcinomas. Cell Cycle 2009; 8: 2122–2124.
Wagle N, Emery C, Berger MF et al, Dissecting therapeutic resistance to RAF inhibition in melanoma by tumor genomic profiling. J Clin Oncol 2011; 29: 3085–3096.
Waterfall JJ, Arons E, Walker RL et al, High prevalence of MAP2K1 mutations in variant and IGHV4-34-expressing hairy-cell leukemias. Nat Genet 2014; 46: 8–10.
Burns BF, Colby TV, Dorfman RF . Langerhans' cell granulomatosis (histiocytosis X) associated with malignant lymphomas. Am J Surg Pathol 1983; 7: 529–533.
Egeler RM, Neglia JP, Arico M et al, The relation of Langerhans cell histiocytosis to acute leukemia, lymphomas, and other solid tumors. The LCH-Malignancy Study Group of the Histiocyte Society. Hematol Oncol Clin North Am 1998; 12: 369–378.
Egeler RM, Neglia JP, Puccetti DM et al, Association of Langerhans cell histiocytosis with malignant neoplasms. Cancer 1993; 71: 865–873.
Greaves WO, Bueso-Ramos C, Fayad L . Classical Hodgkin's lymphoma associated with Langerhans cell histiocytosis: multiagent chemotherapy resulted in histologic resolution of both the classical Hodgkin's lymphoma and Langerhans cell proliferation components. J Clin Oncol 2011; 29: e76–e78.
Adu-Poku K, Thomas DW, Khan MK et al, Langerhans cell histiocytosis in sequential discordant lymphoma. J Clin Pathol 2005; 58: 104–106.
Almanaseer IY, Kosova L, Pellettiere EV . Composite lymphoma with immunoblastic features and Langerhans' cell granulomatosis (histiocytosis X). Am J Clin Pathol 1986; 85: 111–114.
Christie LJ, Evans AT, Bray SE et al, Lesions resembling Langerhans cell histiocytosis in association with other lymphoproliferative disorders: a reactive or neoplastic phenomenon? Hum Pathol 2006; 37: 32–39.
Licci S, Boscaino A, De Palma M et al, Concurrence of marginal zone B-cell lymphoma MALT-type and Langerhans cell histiocytosis in a thyroid gland with Hashimoto disease. Ann Hematol 2008; 87: 855–857.
Capper D, Preusser M, Habel A et al, Assessment of BRAF V600E mutation status by immunohistochemistry with a mutation-specific monoclonal antibody. Acta Neuropathol 2011; 122: 11–19.
Verma S, Greaves WO, Ravandi F et al, Rapid detection and quantitation of BRAF mutations in hairy cell leukemia using a sensitive pyrosequencing assay. Am J Clin Pathol 2012; 138: 153–156.
Davies H, Bignell GR, Cox C et al, Mutations of the BRAF gene in human cancer. Nature 2002; 417: 949–954.
Chakraborty R, Burke TM, Hampton OA et al, Alternative genetic mechanisms of BRAF activation in Langerhans cell histiocytosis. Blood 2016; 128: 2533–2537.
Alayed K, Medeiros LJ, Patel KP et al, BRAF and MAP2K1 mutations in Langerhans cell histiocytosis: a study of 50 cases. Hum Pathol 2016; 52: 61–67.
Jabbar KJ, Luthra R, Patel KP et al, Comparison of next-generation sequencing mutation profiling with BRAF and IDH1 mutation-specific immunohistochemistry. Am J Surg Pathol 2015; 39: 454–461.
Estrella JS, Tetzlaff MT, Bassett RL et al, Assessment of BRAF V600E in coloreactal carcinoma: tissue-specific discordance between immunohistochemistry and seqie3ncing. Mol Cancer Ther 2015; 14: 2887–2895.
Acknowledgements
We thank Jawad Manekia and Mohammad Mohammad for technical assistance in the next-generation sequencing study.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Rights and permissions
About this article
Cite this article
Pina-Oviedo, S., Medeiros, L., Li, S. et al. Langerhans cell histiocytosis associated with lymphoma: an incidental finding that is not associated with BRAF or MAP2K1 mutations. Mod Pathol 30, 734–744 (2017). https://doi.org/10.1038/modpathol.2016.235
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/modpathol.2016.235
This article is cited by
-
Frequency detection of BRAF V600E mutation in a cohort of pediatric langerhans cell histiocytosis patients by next-generation sequencing
Orphanet Journal of Rare Diseases (2021)
-
Focal Rosai–Dorfman disease coexisting with lymphoma in the same anatomic site: a localized histiocytic proliferation associated with MAPK/ERK pathway activation
Modern Pathology (2019)
-
Immunohistochemistry Innovations for Diagnosis and Tissue-Based Biomarker Detection
Current Hematologic Malignancy Reports (2019)
-
Langerhans cell histiocytosis associated with classical Hodgkin lymphoma contains BRAF V600E mutation
Annals of Hematology (2019)
-
Histiocytic cell neoplasms involving the bone marrow: summary of the workshop cases submitted to the 18th Meeting of the European Association for Haematopathology (EAHP) organized by the European Bone Marrow Working Group, Basel 2016
Annals of Hematology (2018)