Abstract
Hepatocellular adenoma is considered to occur exclusively in non-fibrotic livers. It is a heterogeneous entity and a molecular classification is now widely accepted. The most frequent hepatocellular adenoma subtype, namely inflammatory adenoma, harbor somatic activating mutations of genes involved in the interleukin-6 pathway that lead to high C-reactive protein and serum amyloid A expression. The aim of our study was to investigate a series of benign hepatocellular neoplasms developed on cirrhotic livers and characterized by an unequivocal histological diagnosis. We performed a clinical, pathological, and molecular study of 10 benign hepatocellular neoplasms developed in three patients with cirrhosis. Markers allowing hepatocellular adenoma classification were assessed by quantitative real-time PCR and immunohistochemistry. Samples were sequenced for CTNNB1, HNF1A, IL6ST, GNAS, STAT3, and TERT (promoter) mutations. A control series of 32 classical macronodules developed in cirrhosis related to various etiologies was screened by immunohistochemistry and gene sequencing. The three patients had cirrhosis related to metabolic syndrome and/or alcohol intake; two had a single tumor, while the third developed more than 30 lesions. Microscopic examination showed well-differentiated neoplasms sharing features with inflammatory adenoma including inflammatory infiltrates, sinusoidal dilatation, and dystrophic vessels. Sequencing revealed classical hotspot somatic mutations (IL6ST, n=8; STAT3, n=1; and GNAS, n=1) known to be responsible for IL-6/JAK/STAT pathway activation. Two classical high-grade macronodules demonstrated high serum amyloid A and/or C-reactive protein expression, without gene mutations. Altogether, our findings support the existence of rare inflammatory adenoma developed in cirrhosis.
Similar content being viewed by others
Main
Hepatocellular adenoma is a rare and benign neoplasm that typically occurs in young women with a history of long-term use of oral contraceptive drugs.1 It is defined as a monoclonocal proliferation of well-differentiated hepatocytes that show no or mild histological atypia.1 Recent molecular studies have shown that hepatocellular adenoma is a heterogenous entity, and a molecular classification comprising four subgroups has been proposed, and is now widely accepted.2, 3 The first group of hepatocellular adenoma (30% of all hepatocellular adenoma) is defined by bi-allelic, inactivating mutations of a transcription factor involved in liver differentiation and metabolism, HNF1A (hepatocyte nuclear factor 1A).4 HNF1A-inactivated hepatocellular adenomas are histologically usually characterized by a massive steatosis in the tumor.3, 5 Beta-catenin-mutated hepatocellular adenomas (15–20%) are characterized by CTNNB1-activating mutations responsible for constitutive Wnt/Beta-catenin pathway activation.2, 6 This subgroup has the higher risk of malignant transformation,3, 6, 7 and microscopic examination may demonstrate moderate atypia.2, 5 The third group of hepatocellular adenoma, namely inflammatory adenoma (about 50% of all hepatocellular adenomas), harbor somatic gain-of-function mutations in either IL6ST, FRK, JAK1, STAT3, or GNAS genes activating the interleukin-6/JAK/STAT pathway.3, 6, 8, 9 They are histologically characterized by sinusoidal dilation, inflammatory infiltrates, and dystrophic vessels often surrounded by fibrotic tissue. An immunohistochemical panel has been developed to allow pathological identification of all three hepatocellular adenoma subgroups and inflammatory adenomas are characterized by an overexpression of the C-reactive and serum amyloid A proteins in tumor hepatocytes.5 The last hepatocellular adenoma subgroup is unclassified hepatocellular adenoma.
Although hepatocellular carcinoma usually develops in patients with chronic liver disease and fibrotic or cirrhotic liver,1 hepatocellular adenoma is usually diagnosed in non-fibrotic, non-cirrhotic parenchyma.1, 10 Recently, Sasaki et al11, 12 reported cases of benign hepatocellular nodules in patients with alcoholic cirrhosis that displayed serum amyloid A immunohistochemical expression and shared overlapping histological features with inflammatory adenoma. Moreover, an activating somatic STAT3 mutation was identified in 2 out of 17 cases. Authors suggested that these lesions might represent a new subtype of inflammatory hepatocellular tumors that may develop in the setting of alcoholic cirrhosis.11, 12
In the present study, we report a series of 10 hepatocellular neoplasms developed in three patients with cirrhosis that shared immunohistochemical and molecular features with inflammatory adenoma. In order to determine whether ‘classical’ cirrhotic nodules may also belong to this particular subset of lesions, we also further investigated a series of 32 macronodules developed on cirrhosis of various etiologies.
Materials and methods
Patients and Samples
The 10 hepatocellular tumors studied were addressed for diagnostic expertise at our departments between 2004 and 2012. They were retrospectively analyzed. One of the cases was included in a former study.13
A total of 32 classical cirrhotic macronodules developed in patients that underwent liver resection or transplantation in our two hospitals (Pellegrin, Bordeaux, France; and Henri Mondor, Creteil, France) were further included in the study. The nodules were identified during gross examination of the surgical specimens and frozen samples were available in all cases. Each patient has signed a written consent to allow tumor molecular analysis. For each nodule, diagnosis (low- or high-grade dysplastic macrodule) was established by a collective reviewing during a former study using established criteria of the International Working Party and of the International Consensus Group for Hepatocellular Neoplasia.14, 15
Immunohistochemistry
Immunostaining was performed on whole sections of tumor and non-tumoral liver with the following antibodies: anti-liver-fatty acid-binding protein (polyclonal AB, Abcam, 1/50), anti-β-catenin (monoclonal mouse AB, BD Biosciences, 1/200), anti-glutamine synthetase (monoclonal mouse AB, BD Biosciences, 1/400), anti-serum amyloid A (monoclonal mouse AB, Dako, 1/50), anti-C-reactive protein (610517, BD Biosciences-Pharmigen, 1/1000), anti-Glypican 3 (clone IG12, Biomosaics, 1/100), and anti-Ki67 (RBK027, Zytomed, 1/100). Slides were processed in an automated immunostainer (Leica BondMax or Dako) according to the manufacturer’s instructions.
RNA Extraction and Quantitative Real-Time PCR
RNA was extracted from frozen samples using the Qiagen Rneasy kit. Quantitative RT–PCR was performed as previously described,16 using primers and probe sets from Applied Biosystems: R18S (Ribosomal 18S; 4352930), FABP1 (Hs00203685_m1), UGT2B7 (Hs00426592_m1), GLUL (Hs00374213_m1), LGR5 (Hs00173664_m1), CRP (Hs00265044_m1), and SAA2 (Hs01667582_m1). Gene expression was normalized to ribosomal 18S mRNA, and expression level of the tumor sample was compared with the mean level of the corresponding gene expression in normal liver tissues (n=4), and expressed as an n-fold ratio. The relative amount of RNA was calculated with the 2-delta delta CT method.
DNA Extraction and Sequencing
For all samples, tumor and non-tumor DNA was extracted using a salting-out procedure. DNA sequencing was performed as previously described,6 and all samples were systematically sequenced for CTNNB1 (exons 2, 3, 4, 6, 7, and 8), HNF1A (exons 1–10), IL6ST (exon 6), GNAS (exon 8), STAT3 (exons 2, 5, 16, and 20), FRK (exon 6), and TERT promoter.16, 17
Results
Clinical and Imaging Features of the Index Patients
We identified atypical nodules in three index patients with chronic liver disease (Table 1). Patients 1 (#958, female, 51 years) and 2 (#708, male, 54 years) developed a unique nodule during surveillance of cirrhosis related to metabolic syndrome associated with alcohol intake (Table 1). The third patient (#2369), a 37-year-old male with metabolic syndrome, consulted for abdominal pain due to intra-tumor bleeding and more than 30 nodules were identified in a steatotic liver, 8 of which were resected and underwent complete pathological and molecular investigation (Table 1).
Computerized tomography showed in patient 2 a hypervascular nodule without washout; magnetic resonance imaging was performed for patient 3 and revealed a steatotic liver with numerous nodules characterized by a T2 hypersignal (Figure 1).
Magnetic resonance imaging was performed in patient 3 (#2369) and revealed a steatotic liver with numerous nodules characterized by a T2 hypersignal (a). Computerized tomography showed in patient 2 (#708) a hypervascular nodule without washout (b, arterial phase). At gross examination, tumor no. 3c (#2372) had a yellowish-red appearance (c), while tumor no. 2 (#708) had a multinodular architecture (d).
The two first patients did not show tumor recurrence 57 and 80 months after surgical removal of the tumors, whereas the third patient deceased from acute liver failure within a few days after surgery.
Pathological Findings of the Index Patients
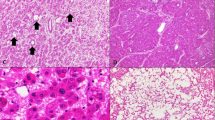
Gross examination of the surgical specimens revealed brown or yellowish-red nodules that were well demarcated from the surrounding parenchyma (Figure 1). In all cases, histological examination showed well-differentiated neoplasms composed of hepatocytes arranged in thin trabeculae without significant atypia and normal nuclear-to-cytoplasmic ratio. No mitotic figures were observed. Inflammatory infiltrates, foci of sinusoidal dilatation, dystrophic vessels, or fibrotic bands were identified in 8, 7, 7, and 7 cases, respectively (Table 2 and Figure 2). If microscopic appearance of the multiple tumors developed in third patient (#2369) was all highly suggestive of inflammatory adenoma, histological diagnosis of the other lesions was not straightforward: the first tumor (#958) was initially diagnosed as a focal nodular hyperplasia-like nodule and with thick fibrous bands and a jigsaw-puzzle appearance reminiscent of what is usually observed in congenital hepatic fibrosis, while the second tumor (#708), divided by thin fibrotic bands forming large incomplete irregular pseudo-nodules, lacked other hallmark histological features of inflammatory adenoma and was diagnosed as a regenerative macronodule (Figure 2).
At low magnification, tumor no. 3c (#2372) (a) and tumor no. 1 (#958) (b) were relatively well demarcated from the adjacent cirrhotic parenchyma (hematein–eosin–saffron (HES), × 20). Tumor no. 2 (#708) was relatively ill defined (arrows) and had a multinodular architecture, with thin fibrotic bands surrounding the nodules (c) (HES, × 20). Histological appearance of tumors that developed in patient no. 3 (#2369) were suggestive of IHCA, with inflammatory infiltrates, dystrophic vessels, and ductular reaction (d) (HES, × 200). Tumor no. 1 (#958) had an atypical histological appearance, with thick fibrotic bands and a jigsaw-puzzle pattern reminiscent of what is observed in congenital hepatic fibrosis (e) (HES, × 200). Tumor no. 2 (#708) featured fibotic bands and inflammatory infiltrates (f) (HES, × 200).
Microscopic examination of non-tumoral livers showed in all cases destruction of the lobular architecture, with regenerative nodules entirely surrounded by fibrotic connective tissue (Figure 3). Histological features suggesting alcoholic or non-alcoholic liver disease were also observed: steatosis (n=3), inflammation/activity (n=3), and ballooning (n=2; Table 2 and Figure 3).
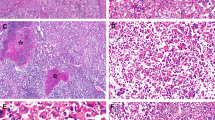
Immunohistochemical experiments demonstrated high and diffuse C-reactive protein expression by neoplastic cells in tumor no. 2 (#708) (a, × 20) and no. 3c (#2372) (b, × 200). Tumor no. 1 (#958) showed an atypical zonated C-reactive protein staining, with expression restricted to perifibrotic areas (c, × 100).
Immunohistochemical staining of the tumors demonstrated C-reactive protein (3/3) and serum amyloid A (2/3) overexpression by neoplastic cells (Figure 4). Tumor #958 exhibited a particular focal and patchy C-reactive protein staining, with expression restricted only to perifibrotic areas (Figure 4c). L-FABP immunostaining intensity was similar to that of adjacent, non-tumoral liver. Glutamine synthetase expression was heterogeneous and weak, with a lack of beta-catenin nuclear accumulation. Glypican 3 immunostaining was negative. The proliferation index, assessed by Mib-1 immunohistochemistry, was below 1% in all cases.
Molecular Analyses
The mRNA expression profile of the tumors was also suggestive of inflammatory adenoma, with elevated C-reactive protein and serum amyloid A mRNA levels and a lack of significant GLUL upregulation or FABP1 downregulation (Table 3).
Sequencing of the tumor DNA extracted from frozen samples of the 10 nodules identified in all cases a heterozygous somatic mutation at hotspots previously described in inflammatory adenoma and known to activate the IL-6/JAK/STAT pathway (Table 3). Tumor no. 1 and no. 2 harbored a mutation in GNAS and STAT3 genes, respectively. For patient no. 3, all the eight nodules were mutated in the same gene, IL6ST (five different mutations across the eight nodules; Table 3). All the mutations involved the binding site of IL6ST for IL-6, and out of the five different mutations identified two have not been reported before in inflammatory adenoma (c.565_579del, c.569_577del).18 Identical mutations were identified in three (c.565_579del) and two (c.557_571del) tumors. If c.557_571del is the second most frequent mutation reported in inflammatory adenoma, the variant c.565_579del was not identified before, and whether the three nodules harboring this alteration result or not from an independent monoclonal proliferation of hepatocytes remains to be determined.
No additional mutations in CTNNB1, HNF1A, FRK, JAK1, or TERT promoter were identified.
Cirrhotic Macronodules
The identification of these nodules with an inflammatory adenoma molecular pattern developed in cirrhotic patients prompted us to analyze a series of 32 cirrhotic nodules developed in 18 patients. Median age was 55 years (range 47–69), sex ratio was M/F=15/3. The underlying chronic liver diseases were related to hepatitis C virus infection (n=7), alcohol (n=6), non-alcoholic steatohepatitis (n=2), and rare diseases (hemochromatosis n=1, unknown etiology n=2). Pathological reviewing identified low-grade dysplastic macronodules (LGDN, n=21) or high-grade dysplastic macronodules (HGDN, n=11). Immunohistochemical C-reactive protein and serum amyloid A staining were performed in all cases, and C-reactive protein or serum amyloid A diffuse overexpression compared with adjacent cirrhotic parenchyma was identified in two HGDN (CHC1780T and CHC2354T). In both cases, small foci of hepatocytes expressing C-reactive protein and/or serum amyloid A were also identified in the adjacent liver tissue. No mutations in IL6ST, STAT3, JAK1, FRK, or GNAS were identified.
Discussion
Our study identified a series of benign inflammatory hepatocellular neoplasms developed in the setting of cirrhosis. In the three index patients, these tumors were atypical for cirrhotic macronodules and showed overlapping phenotypical features of inflammatory adenoma and gene mutations specific of this tumor subtype. Indeed, if the microscopic appearance of the lesions was highly suggestive of inflammatory adenoma in the patient with multiple nodules, the suggested diagnoses for the other tumors were regenerative macronodule and focal nodular hyperplasia-like nodule.
In cases 2 and 3, the immunophenotype and molecular features of the lesions was similar to those observed in inflammatory adenoma, with diffuse C-reactive protein and serum amyloid A overexpression related to IL6ST-, STAT3-, or GNAS-activating mutations. For case 1, C-reactive protein expression was restricted to perifibrotic areas, with a negative serum amyloid A immunostaining and quantitative PCR experiments demontrated a relatively moderate increase of C-reactive protein and serum amyloid A mRNA levels compared with the other cases. A GNAS somatic mutation was identified in this tumor, and its particular phenotype is probably related to the lower activation of the IL-6/JAK/STAT pathway induced by GNAS in comparison to that induced by IL6ST or STAT3 (ref. 13).
Interestingly, in the patient with multiple nodules, we identified different IL6ST mutation in five out of the eight analyzed nodules. These results showed that at least half of the nodules resulted from an independent monoclonal proliferation of hepatocytes with a specific genetic alteration. Altogether, the clinical (no tumor recurrence), histological (lack of atypia), phenotypical (no Glypican 3 expression), and molecular (no TERT promoter mutations) features of the 10 nodules supported their benign nature.
If hepatocellular adenoma is known to arise in non-fibrotic, non-cirrhotic liver, our observations show that inflammatory adenoma and inflammatory liver adenomatosis may also rarely develop in the setting of chronic liver disease and cirrhosis. Interestingly, all three patients had chronic liver disease related to well-established risk factors for inflammatory adenoma development in patients without fibrotic livers, namely metabolic syndrome and alcohol intake.3, 19 These results also underlined the key role of non-tumor liver assessment in front of an inflammatory adenoma diagnosed on tumor biopsy because it will change the therapeutic approach due to the higher risk of liver failure after major hepatectomy. The rising incidence of NASH in the population may increase the numbers of inflammatory adenoma developed on cirrhosis and consequently we have to pay attention to such cases in the future.
Next, we showed that the inflammatory phenotype, ie, serum amyloid A or C-reactive protein diffuse overexpression in tumor hepatocytes, is rare in classical LGDN or HGDN cirrhotic nodules (2/32) and these tumors did not show any mutations of genes involved in the IL-6/JAK/STAT pathway. These results suggest that immunophenotype alone is not a sufficient diagnostic criterion to identify an inflammatory adenoma developed in a cirrhotic liver.
Cirrhotic nodules strongly expressing serum amyloid A have been formerly reported by Sasaki et al11, 12 in patients with alcoholic cirrhosis. Interestingly, these nodules also shared similar histological features with inflammatory adenoma but only two cases demonstrated a classical STAT3-activating mutation. These results indicate that other molecular alterations leading to IL-6/JAK/STAT pathway activation could be involved in the development of inflammatory nodules within cirrhosis, and their identification will probably require novel high-throughput approaches, such as whole-exome or whole-genome sequencing. However, it is not rare to observe focal C-reactive protein or serum amyloid A expression in macronodules as well as in ‘regular’ cirrhotic nodules. These proteins are known to be produced by hepatocytes in response to a wide range of cytokines, and may be overexpressed in cirrhotic nodules under local or systemic inflammatory conditions.
In conclusion, our study supports the existence of inflammatory adenomas developed in the setting of chronic liver disease and cirrhosis. If these tumors may not harbor all the histological hallmark features of classical inflammatory adenoma developed in non-fibrotic liver, they share common risks factors and molecular alterations, and might thus be classified as inflammatory adenoma. Further studies will have to determine whether other hepatocellular adenoma subtypes may also occur on fibrotic livers and whether these tumors have a higher risk of malignant transformation than hepatocellular adenoma developed in non-fibrotic livers, as it was recently observed in patients with vascular liver diseases.20
References
Bioulac-Sage P, Balabaud C, Wanless I . Focal nodular hyperplasia and hepatocellular adenoma. In: Bosman FT, Carneiro F, Hruban RH, Theise ND (eds). WHO Classification of Tumours of the Digestive System, 4th edn. International Agency for Research on Cancer: Lyon, France, 2010, pp 198–204.
Zucman-Rossi J, Jeannot E, Nhieu JT et al. Genotype-phenotype correlation in hepatocellular adenoma: new classification and relationship with HCC. Hepatology 2006;43:515–524.
Nault JC, Bioulac-Sage P, Zucman-Rossi J . Hepatocellular benign tumors-from molecular classification to personalized clinical care. Gastroenterology 2013;144:888–902.
Bluteau O, Jeannot E, Bioulac-Sage P et al. Bi-allelic inactivation of TCF1 in hepatic adenomas. Nat Genet 2002;32:312–315.
Bioulac-Sage P, Laumonier H, Couchy G et al. Hepatocellular adenoma management and phenotypic classification: the Bordeaux experience. Hepatology 2009;50:481–489.
Pilati C, Letouze E, Nault JC et al. Genomic profiling of hepatocellular adenomas reveals recurrent FRK-activating mutations and the mechanisms of malignant transformation. Cancer Cell 2014;25:428–441.
Farges O, Ferreira N, Dokmak S et al. Changing trends in malignant transformation of hepatocellular adenoma. Gut 2011;60:85–89.
Rebouissou S, Amessou M, Couchy G et al. Frequent in-frame somatic deletions activate gp130 in inflammatory hepatocellular tumours. Nature 2009;457:200–204.
Pilati C, Amessou M, Bihl MP et al. Somatic mutations activating STAT3 in human inflammatory hepatocellular adenomas. J Exp Med 2011;208:1359–1366.
Goodman ZD, Terraciano LM . Tumours and tumour-like lesions of the liver. In: MacSween RNM, Burt AD, Portmann B, Ferrell LD (eds). MacSween's Pathology of the Liver, 6th edn. Churchill Livingstone: Edinburgh, Scotland, 2011, pp 762–764.
Sasaki M, Yoneda N, Kitamura S, Sato Y, Nakanuma Y . A serum amyloid A-positive hepatocellular neoplasm arising in alcoholic cirrhosis: a previously unrecognized type of inflammatory hepatocellular tumor. Mod Pathol 2012;25:1584–1593.
Sasaki M, Yoneda N, Sawai Y et al. Clinicopathological characteristics of serum amyloid A-positive hepatocellular neoplasms/nodules arising in alcoholic cirrhosis. Histopathology 2015;66:836–845.
Nault JC, Fabre M, Couchy G et al. GNAS-activating mutations define a rare subgroup of inflammatory liver tumors characterized by STAT3 activation. J Hepatol 2012;56:184–191.
International Consensus Group for Hepatocellular Neoplasia. The International Consensus Group for Hepatocellular N. Pathologic diagnosis of early hepatocellular carcinoma: a report of the international consensus group for hepatocellular neoplasia. Hepatology 2009;49:658–664.
Nault JC, Calderaro J, Di Tommaso L et al. Telomerase reverse transcriptase promoter mutation is an early somatic genetic alteration in the transformation of premalignant nodules in hepatocellular carcinoma on cirrhosis. Hepatology 2014.
Calderaro J, Labrune P, Morcrette G et al. Molecular characterization of hepatocellular adenomas developed in patients with glycogen storage disease type I. J Hepatol 2013;58:350–357.
Nault JC, Mallet M, Pilati C et al. High frequency of telomerase reverse-transcriptase promoter somatic mutations in hepatocellular carcinoma and preneoplastic lesions. Nat Commun 2013;4:2218.
Poussin K, Pilati C, Couchy G et al. Biochemical and functional analyses of gp130 mutants unveil JAK1 as a novel therapeutic target in human inflammatory hepatocellular adenoma. Oncoimmunology 2013;2:e27090.
Paradis V, Champault A, Ronot M et al. Telangiectatic adenoma: an entity associated with increased body mass index and inflammation. Hepatology 2007;46:140–146.
Sempoux C, Paradis V, Komuta M et al. Hepatocellular nodules expressing markers of hepatocellular adenomas in Budd-Chiari syndrome and other rare hepatic vascular disorders. J Hepatol 2015; epub ahead of print 25 June 2015; doi: 10.1016/j.jhep.2015.06.017.
Author information
Authors and Affiliations
Corresponding authors
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Rights and permissions
About this article
Cite this article
Calderaro, J., Nault, J., Balabaud, C. et al. Inflammatory hepatocellular adenomas developed in the setting of chronic liver disease and cirrhosis. Mod Pathol 29, 43–50 (2016). https://doi.org/10.1038/modpathol.2015.119
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/modpathol.2015.119
This article is cited by
-
β-Catenin-activated inflammatory hepatocellular adenoma with pigmentation and atypical features: a case report
Clinical Journal of Gastroenterology (2023)
-
Benign liver tumours: understanding molecular physiology to adapt clinical management
Nature Reviews Gastroenterology & Hepatology (2022)
-
Autofluorescence imaging within the liver: a promising tool for the detection and characterization of primary liver tumors
European Radiology (2022)
-
Hepatic nodules with arterial phase hyperenhancement and washout on enhanced computed tomography/magnetic resonance imaging: how to avoid pitfalls
Abdominal Radiology (2020)
-
Hepatocellular nodules in vascular liver diseases
Virchows Archiv (2018)