Abstract
Distinguishing ulcerative colitis (UC) from Crohn’s disease (CD) is normally based on evaluation of a variety of clinical, radiologic, serologic and pathologic findings, the latter in biopsy and/or resection specimens. Unfortunately, some patients with IBD show overlapping pathologic features of UC and CD, which makes definite distinction between these two disorders difficult or even impossible. In most instances of uncertainty, the patient shows clinical and pathologic features of UC, but in addition, the patient’s colon resection specimen reveals one or more CD-like features. In this setting, a diagnosis of indeterminate colitis (IC) is often rendered. IC is not a distinct disease entity, and, thus, it has no diagnostic criteria. The most common causes of uncertainty in IBD pathology that may lead to a diagnosis of IC in a colon resection specimen includes the presence of fulminant (severe and toxic) colitis, insufficient radiologic, endoscopic, or pathologic information (including analysis of prior biopsies) on the patient, failure to utilize major diagnostic criteria as hard evidence in favor of CD, failure to recognize unusual variants of UC and CD that may mimic each other, failure to recognize non-IBD mimics and other superimposed diseases that cause unusual pathologic features in a resection specimen, an attempt to distinguish UC from CD in mucosal biopsies of the colon and ileum, or an attempt to change the patients diagnosis (of UC or CD) based on pouch or diversion-related complications. Details of each of these causes of uncertainty are discussed, in detail, in this review article. A diagnosis of IC should never be made clinically or by pathologists based on evaluation of pre-resection colonic mucosal biopsies. Ultimately, the majority of indeterminate cases represent UC, and, thus, most of these patient can be treated safely with a colectomy combined with an ileal pouch anal anastomosis procedure.
Similar content being viewed by others
General comments, definition and terminology
Distinguishing ulcerative colitis (UC) from Crohn’s disease (CD) is normally based on evaluation of a variety of clinical, radiologic, endoscopic and pathologic findings in biopsy and/or resection specimens.1 In certain circumstances, particularly when there are overlapping clinical features, it becomes incumbent on the pathologist to help establish a definitive diagnosis of either UC or CD (or other types of IBD) in resection specimens.2, 3 In most instances, these two disorders may be readily distinguished from each other, particularly when each exhibits classic gross and microscopic features (Table 1).3 Unfortunately, some patients with IBD show overlapping pathologic features of UC and CD, which makes definite distinction between these two disorders difficult, or even impossible. When a pathologist cannot make a definite diagnosis of UC or CD (or any of the other type of IBD that mimics UC or CD), a diagnosis of ‘indeterminate colitis’ (IC) is often rendered.3 Some of the other terms that are used in this setting include ‘uncertain colitis,’ ‘idiopathic chronic colitis,’ ‘IBD-unclassified,’ ‘IBD-nos’ and ‘IBD-unknown etiology’.1, 4 In 2005, an international working party of IBD physicians indicated a preference for the term ‘IBD unclassified’ for patients with chronic colitis (IBD) without definitive features of UC or CD.1 Regardless of the term used to describe this condition, it is important to realize that IC is not a distinct disease entity, and, thus, has no diagnostic criteria. IC should be regarded as an interim diagnosis until further information (clinical, radiologic or pathologic), or follow-up data, allows definite classification of the patient’s true IBD type.
The prevalence rate of establishing an interim diagnosis of IC is highly variable among institutions and individual pathologists.3, 5 Previously reported rates of diagnosis range from 1 to 20% of IBD cases.3, 5 The frequency of establishing this diagnosis is often related to the level of awareness of the broad spectrum of pathologic features that may occur in UC and CD (see below section on causes of uncertainty in IBD pathology). For instance, in a study by Farmer et al,6 24 university medical center pathologists from 8 institutions evaluated 84 colectomy specimens and 35 sets of biopsies from 119 consecutive patients with colonic IBD. An experienced IBD pathologist subsequently reviewed these cases without knowledge of clinical data or the patient’s prior diagnosis, and rendered his own diagnosis. The ‘GI pathologist’s’ diagnosis differed from the initial diagnosis in 45% of surgical specimens. For instance, of the 70 cases initially diagnosed as UC, 43% were changed to CD or IC, whereas of the 23 cases initially diagnosed as CD, 17% were changed to either UC or IC. These authors concluded that more accurate diagnostic criteria are needed to facilitate IBD patient care and to optimize treatment outcome.
Unfortunately, there is also a lack of consistency and clarity among pathologists with regard to the meaning, significance and definition of IC.5, 6 For instance, in an informal survey of 10 GI pathologists (unpublished data), five pathologists defined IC as “IBD: unclear if UC or Crohn’s pathologically”, three defined it as “acute fulminant colitis (with fissures),” and two defined it as “IBD, unclear either clinically and pathologically.” Of the 10 GI pathologists, 8 believed that this diagnosis should only be rendered in resection specimens, but two suggested that it can be rendered in biopsies as well, a practice that is not recommended (see below). An attempt to establish a diagnosis of IC based on evaluation of preoperative biopsy specimens should be avoided, as this practice has a high potential for diagnostic error (see further below).7
There are many reasons why establishing a correct diagnosis of UC or CD in patients with IBD is important.1, 8 These two diseases have (presumably) different etiology, natural history, potential need for further surgical procedures, forms of medical management and response rates to individual drugs, risk for other disorders (such as PSC) and incidence of involvement of other portions of the GI tract.1 Furthermore, there are differences in rates of familial involvement. Finally, and perhaps most importantly, UC patients are generally considered good candidates for a total colectomy and ileal pouch anal anastomosis (IPAA) procedure, whereas CD is generally considered a contraindication for this procedure because of the high risk of severe pouch complications.9, 10
This review will address many of the challenges associated with interpretation of pathology resection specimens that demonstrate mixed features of UC or CD, and provides information that will help distinguish these entities. It is the hope that with more specific and extensive knowledge of the broad range of pathologic manifestations of UC and CD, pathologists will lower their rate of IC diagnoses.
Historical perspective
The term ‘indeterminate colitis’ was first introduced in 1970 by Kent et al11 in a retrospective study of colectomies from 222 patients with IBD, a small proportion of which presented with fulminant disease. In this study, 14 cases were categorized as IC because of ‘overlapping features and/or data insufficient to make a final decision.’ Price12 evaluated 30 colectomy specimens from patients with nonspecific IBD, 27 of which presented with fulminant colitis and a requirement for urgent surgery. In fact, 21 of these patients (70%) also had toxic distension of the colon, termed megacolon. In that study, many of the specimens contained overlapping features, such as cases seemingly UC, but with discontinuous disease, fissuring ulceration, transmural inflammation or relative rectal sparing. Interestingly, in that study, none of the patients had granulomas. Based on the presence of overlapping UC/CD features in these specimens, Price concluded that colonic resection specimens from patients with fulminant colitis are often indeterminate with regard to the specific diagnosis. It is now known that patients with fulminant UC may reveal unusual CD-like features, such as relative rectal sparing, transmural inflammation and superficial fissuring ulcers.3, 13 These IBD patients follow a clinical course similar to UC, and have high success rate after total colectomy and IPAA procedure.4, 9, 14, 15 Unfortunately, since the original studies by Kent and Price, the term ‘IC’ has been inappropriately expanded by both clinicians and pathologists for a variety of different reasons (see Table 2).4, 5, 15 In my experience, lack of sufficient clinical information, lack of awareness of unusual pathologic variants of UC or CD, failure to diagnose CD when one or more major diagnostic criteria are present and failure to recognize non-IBD mimics and superimposed diseases are the most frequent reasons why pathologists diagnose IC. Furthermore, clinicians and pathologists often have different criteria for UC and CD. For instance, in an article written by a colorectal surgeon in 2002, titled ‘The Case for IPAA for Indeterminate Colitis,’ it is apparent that many patients who would normally be diagnosed clinically as IC (based on clinicians interpretation of pathologic findings), would normally be able to be diagnosed accurately as either UC or CD by pathologists with expertise in IBD.15 For example, the author of that paper indicated that resection specimens with microscopic skip areas, longitudinal ulcers or mild transmural inflammation (not transmural lymphoid aggregates) focally, in a specimen that otherwise appears similar to UC, would be considered ‘indeterminate.’ However, several studies have shown that UC resection specimens may reveal any, or all, of these histologic features under certain circumstances, and thus, these are not considered valid reasons to change a diagnosis of UC to CD.6, 13, 16 Close cooperation between clinicians and pathologists is essential when faced with an IBD resection specimen with overlapping or unusual features.1
Causes of uncertainty in IBD pathology
Table 2 outlines the most frequent causes of uncertainty among pathologists when faced with a colonic IBD resection specimen in which UC or CD are considered the most likely clinical diagnoses. These reasons are discussed, in detail, in this section, with particular emphasis on pathologic features that can help distinguish UC from CD (and other diseases) more readily.
Fulminant Colitis
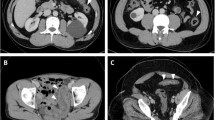
Fulminant colitis is a clinical condition in which patients present with severe, usually diffuse, colitis combined with ‘toxic’ symptoms and signs, such as fever, distended and tender abdomen, profuse bloody diarrhea, tachycardia, hypotension, and, in some cases, sepsis.13, 17 Many of these patients develop marked dilatation of the colon (megacolon) usually most noticeable in the transverse colon.13 In all, 5–20% of IBD patients (1.6–2.4/100 000 adults and 0.2/100 000 children) present clinically with fulminant colitis.1, 17, 18 Fulminant colitis develops more commonly at the time of patient’s first presentation of IBD. It occurs much less commonly in patients with a known history of chronic IBD.12, 13, 17, 18 Most cases of fulminant IBD represent UC with some CD-like pathologic features in their resected colon.6, 12, 13, 19 These include relative, or even absolute, rectal sparing, early fissuring ulceration and transmural inflammation (but not transmural lymphoid aggregates) (Figure 1). As mentioned above, most of these patients are treated adequately by total colectomy and IPAA, and have a low pouch complication rate, indicating that the diagnosis of UC is probably accurate. A small proportion of IBD patients who present with fulminant colitis have CD, or a non-UC/non-CD IBD mimic, such as ischemic colitis, radiation colitis, drug-induced colitis, or diverticular disease or a superimposed infection such as CMV or Clostridium difficile (see below).6, 10, 16, 17 Some patients perforate their colon and develop serositis, mimicking CD clinically and pathologically.17, 19 In a detailed clinical and pathologic analysis of 77 IBD patients who presented with fulminant colitis and in whom follow-up information was available, Swan et al19 noted that after utilizing all clinical and follow-up information, 40 were diagnosed as UC, 16 CD and 11 remained indeterminate. In that study, granulomas and transmural lymphoid aggregates revealed a sensitivity and specificity for CD of 88% and 94%, and 50% and 98%, respectively. Of the 40 patients ultimately diagnosed with UC, none had granulomas in their resection specimen, and only two had transmural lymphoid aggregates. However, 80% had fissuring ulcers and 60% had transmural inflammation (non-aggregated). In a study by Yantiss et al,13 the clinical and prognostic significance of early fissuring ulceration was evaluated in 79 patients with fulminant UC. Of the 79 patients, 21 presented with fulminant colitis combined with fissuring ulcers in their resection specimen, and 58 had fulminant colitis without fissures (control group). Patients with fulminant colitis and fissuring ulcers had a higher rate of pancolitis, serositis, backwash ileitis and pouchitis after surgery compared with patients with fulminant colitis but without fissures. However, none of the patients, in either group, developed CD upon follow-up. The results of this study suggested that in patients with fulminant UC, the diagnosis should not be changed to CD on the basis of finding fissuring ulcers in the colon resection specimen.
(a, b) Images from a patient with fulminant UC. (a) The mucosa shows diffuse ulceration with inflammatory polyps (edge of field). Islands of residual submucosa are separated by fissure-like ulcers, some of which may extend into the superficial muscularis propria, as seen in b. Note that in cases of fulminant colitis, with deep ulceration, pockets of inflammation may extend into the muscularis propria (transmural inflammation). However, the inflammation is not in the form of discrete lymphoid aggregates, as in CD.
Insufficient Clinical, Radiologic, Endoscopic and/or Pathologic Information
In some instances, definite distinction between UC and CD in a resected colon from a patient with IBD is difficult because the pathologist does not have sufficient clinical, radiologic, endoscopic or pathologic (prior biopsies) information available at the time of surgical sign out. As, ultimately, the pathologic features of UC and CD are etiologically nonspecific, these diagnoses can often only be established on the basis of combined clinical and pathologic information (Table 3). Useful clinical information includes knowledge of the patient’s family history of (type) of IBD, presence or absence of primary sclerosing cholangitis, type of symptoms and signs, serologic profile (see below), prior diagnoses (rendered on prior surgical samples), and the presence or absence of complicated perianal disease.1, 20, 21 Radiologists are often helpful in differentiating UC from CD in complicated cases.22 The presence or absence of segmental versus diffuse disease, upper GI or distal small intestinal involvement, the presence or absence of strictures, or fistulas, and the thickness of the intestinal wall, are some of the features radiologists use to diagnose UC or CD. Endoscopically, the type and appearance, and distribution, of ulcers, as well as the distribution of disease and the appearance of the ileum are often helpful as well. For instance, a patient with bloody diarrhea, either with or without obstructive symptoms, diffuse involvement of the colon but without involvement of the upper GI tract or distal small intestine, and complicated perianal disease (such as deep fissures, fistulas or strictures), is highly suggestive of CD rather than UC.23 When evaluating diagnostically difficult IBD specimens, it is usually of benefit to evaluate all prior biopsies from the patient’s prior endoscopies, and particularly specimens obtained from the patient’s initial endoscopy, before treatment, in order to help separate UC from CD. For instance, absence of rectal involvement or patchiness of disease would strongly favor CD if these signs were present in the colon before institution of medical management.16, 23, 24 Of course, the presence of CD-like granulomas anywhere in the colon, at any time during the course of the patient’s illness, would also be supportive evidence for CD.7, 18, 25, 26 Obtaining and evaluating important clinical, radiologic and endoscopic information is often best performed by direct face to face contact with the physician at the microscope.
Failure to Utilize Major Diagnostic Criteria as Evidence in Favor of CD
Historically, classic teaching emphasizes that UC and CD show characteristic macroscopic and microscopic features (Table 1).3 Classic features of UC include diffuse continuous disease of the colonic mucosa, with rectal involvement, inflammation that is worse in the most distal segment of colon and an absence (with few exceptions) of deep fissuring ulceration, transmural lymphoid aggregates, long segments or patchy segments of chronic or chronic active disease in the distal ileum, and an absence of granulomas.1, 6, 16, 27, 28 Thus, UC is diagnosed most readily by a characteristic distribution of disease in the absence of major features of CD.16 Major features of CD (ie, features that, essentially, exclude UC in a previously untreated and non-fulminant patient) include segmental disease, absence of rectal involvement, deep fissures, sinuses, and/or fistulous tracts, transmural lymphoid aggregates (distant from deep ulcers) (Figure 2), epithelioid granulomas (unrelated to infection, foreign material or ruptured crypts), upper GI (with few exceptions) and/or lower small intestine involvement (unrelated to backwash ileitis, drugs, infection or bowel prep) and complicated perianal disease.1, 27 Upper GI involvement (esophagus, stomach and or duodenum) is much more often related to CD than UC, particularly if the inflammatory changes are patchy, or associated with deep fissuring ulceration, or granulomas.29, 30, 31, 32 Unfortunately, recognition of these major features may be difficult, particularly when the findings are limited, or masked, by extensive ulceration. Nevertheless, failure to recognize or accept any one or combination of these features as definitive evidence of CD, even in a patient who otherwise appears to have pathologic changes of UC, may lead to a potential erroneous diagnosis of either UC or IC. In the study by Farmer et al6 cited above of 119 IBD patients, the results showed that most errors in pathologic interpretation of IBD cases results from a failure to recognize characteristic changes of CD, such as transmural inflammation and granulomas. In my personal experience, I have found that many cases of IC diagnosed in the community are related to lack of awareness of the pathologist that one or more of these major CD-related features represent sufficient evidence for establishing a diagnosis of CD, despite the fact that many or all of the other inflammatory changes appear UC-like. Thus, the failure to recognize and utilize major criteria as diagnostic of CD can eliminate many apparently diagnostically difficult cases.
Failure to Recognize Unusual Pathologic Variants of IBD
There is increasing recognition of subtypes of UC and CD that are diagnostically challenging and, historically, would likely result in a diagnosis of IC. Whether the prevalence of these subtypes has truly increased, perhaps due to the more widespread use of immunomodulatory therapy, or whether the increase is due to increased recognition is unclear. Unusual subtypes may be broadly classified as (1) UC with CD-like features and (2) CD with UC-like features. A summary of these variants is listed in Table 4.
UC with Crohn’s-like Features
There are several instances in which UC resections may reveal CD-like pathologic features. These are discussed more thoroughly in the following few paragraphs.
Fulminant UC. As discussed more thoroughly above, patients with fulminant UC may reveal relative, or even absolute, rectal sparing, superficial fissuring ulcers and transmural inflammation (but without transmural lymphoid aggregates), all of which can simulate CD.12, 13 The reasons why patients with fulminant UC develop atypical inflammatory changes is unknown, but one potential reason may be related to the fact that the transverse colon is more severely involved in fulminant UC compared with non-fulminant UC where the inflammatory effects of the colon are typically most severe in the rectum.
In cases of toxic megacolon, the bowel wall appears thin, dilated and congested, which can lead to the development of deep mucosal ulcerations similar to CD.17 The serosal surface may demonstrate a fibrinous exudate, but only rarely is there evidence of perforation. The mucosal surface is often extensively denuded, ulcerated and hemorrhagic. Inflammation can extend deep into the wall of the bowel in areas of deep ulceration. These features should not exclude a diagnosis of UC when they occur in a patient with fulminant colitis.
UC with Discontinuous (patchy) Disease. Although UC is normally a disease that affects the colon in a diffuse and continuous manner, there are several situations in which inflammation may be discontinuous or patchy, similar to CD. These include: (1) the tissue-healing effect of topical or oral medical therapy.24, 33, 34, 35 (2) The quiescent phase of mild chronic UC.24, 33, 34, 35 (3) Initial presentation of pediatric UC patients before treatment36, 37, 38, 39 and (4) periappendiceal or cecal patches of inflammation in a patient with subtotal (left-sided) colitis.40, 41, 42, 43, 44, 45
Odze et al24 evaluated 123 rectal mucosal biopsies from 14 patients with UC prospectively treated with 5-aminosalicylic acid enemas. In that study, during the course of treatment, 29% of rectal biopsies from 64% of patients were histologically normal after treatment. Patients treated with 5-ASA enemas showed a significantly higher prevalence rate of histologically normal rectal biopsy specimens compared with those who did not receive enemas. Subsequent studies by other investigators have confirmed and further expanded the findings by Odze et al (Table 5).33, 34, 35 Overall, 30–59% of patients, many of whom are treated with either oral sulphasalazine or steroids, develop patchiness of disease, or rectal sparing, at some point during the course of their illness. It is well known that patients in the chronic (quiescent) phase of disease, without active signs or symptoms, may show minimal, or even complete absence, of features of activity or chronicity, (including architectural distortion) in mucosal biopsies of the colon.24, 33, 34, 35 Biopsies may appear entirely normal, even in areas of prior inflammation. Thus, evaluation of disease continuity by analysis of mucosal biopsy specimens is not a useful method to distinguish UC from CD of the colon, particularly in previously treated IBD patients or those in clinical remission.
Several studies have documented the presence of relative, or even absolute, rectal sparing at initial presentation of pediatric patients with UC.36, 37, 38, 39 For instance, in a study by Glickman et al37 who compared rectal mucosal biopsy findings of 70 pediatric patients and 44 adult patients at initial presentation, before treatment, pediatric patients showed significantly fewer instances of chronic and/or active disease, and a greater number of patients with microscopic skip areas and relative rectal sparing, compared with adults. In that study, 2 of the 70 pediatric patients showed completely normal rectal biopsy specimens at initial presentation. In adults, relative rectal sparing, defined by the presence of less severe inflammation in the rectum compared with the proximal colon, may also occur rarely at initial presentation, but complete rectal sparing is extremely rare.46, 47 In one study, although a 31% prevalence rate of relative rectal sparing was noted in 46 adult UC patients at initial presentation, histologic features of chronicity, such as architectural distortion, were almost always present in the rectal mucosa at the time of diagnosis.47
Focal and/or patchy involvement of the periappendiceal mucosa, cecum or ascending colon may occur in patients with left-sided UC and, therefore, appear as a colon with segmental involvement, which may be falsely interpreted as evidence in favor of CD.40, 41, 42, 43, 44, 45, 48 For instance, in a prospective study of 271 patients with UC, including 63 with left-sided or subtotal colitis, periappendiceal and/or cecal mucosal involvement was identified in 32% of patients.47 In another study by Mutinga et al,45 14 patients with left-sided UC and pathologically confirmed right-sided chronic active inflammation were compared with 35 control patients who had only left-sided UC (without right-sided involvement). These two groups of patients showed similar clinical and demographic features, including the presence and frequency of extra-intestinal manifestations, and an absence of development of CD upon long-term follow-up, which suggests that patchy right-sided inflammation in patients with left-sided colitis has little clinical significance.
Patients who have left-sided or subtotal colitis, an absence of involvement of the ascending colon and/or cecum, but with involvement of the appendix, represents another type of ‘skip’ lesion in UC.43, 44 In one study by Groisman et al,44 ulcerative appendicitis was present in 86% and 87% of patients with non-universal and universal UC, respectively. In another study by Davison and Dixon,43 the appendix was found to be involved with UC in 21% of 62 cases of distal UC.
UC with Granulomas. Although granulomas are typical of CD, up to 30% of patients with UC develop epitheloid granulomas related to degenerated collagen, particulate or fecal matter, superimposed infection, drug reaction and of course, ruptured crypts (Figure 3).18, 25, 49, 50, 51, 52, 53 The latter are more common in patients with moderate or severe disease, and these granulomas may be indistinguishable from CD-associated granulomas. Crypt rupture-related granulomas develop, presumable as a result of mucin extravasation, but this is unclear because in many cases mucous cannot be identified by histochemical stains.18 Since crypt rupture generally occurs more often in the base of mucosa, granulomas associated with UC occur more commonly in that part of the mucosa, whereas CD-associated granulomas occur anywhere in the mucosa, superficial or deep.52, 53 Up to 30% of CD patients contain granulomas in colonic biopsies, and this figure approaches 60% in resection specimens.54
UC with Inflammation in the Distal Ileum (‘Ileitis’). There are several circumstances in which the distal ileum may be involved in patients with UC (Table 6). These include backwash-induced inflammation (backwash ileitis), infection (typically viral), the effects of drugs (such as NSAIDs), or the effects of bowel preparatory agents.53, 54, 55, 56, 57, 58, 59, 60, 61 Backwash ileitis represents inflammation of the distal few centimeters of ileum because of inflammation-induced incompetence of the ileocecal valve and subsequent reflux of colonic contents into the ileum, which, presumably, causes inflammation.54, 56, 57 Thus, backwash ileitis should only be considered in UC patients who have at least moderate-to-severe involvement of the cecum, and with involvement of the area of mucosa surrounding the ileocecal valve. In one study of 200 UC resection specimens, active ileitis was found in 17% of patients, and most of the inflammation was confined to the distal 1–2 cm of ileum.56 Pathologically, backwash ileitis is most often characterized by the presence of mild (neutrophilic) inflammation, focal cryptitis or crypt abscesses, and partial villous atrophy in the distal ileum. Inflammation is most severe distally in areas of mucosa close to or at the ileocecal valve. In rare instances, surface ulceration, or even changes of chronicity, such as pyloric gland metaplasia be present as well.
Non-backwash-related ileitis in patients with UC is not uncommon. In one study55, 58, 59, 60, 61 consisting of 50 patients with UC, 16% had ileal inflammation without involvement of the cecum indicating that backwash was not the cause of ileitis.61 As mentioned above, the effects of bowel preparatory agents, and/or drug such as NSAIDs should be considered in these circumstances, particularly when the inflammation is focal and involving the distal ileum in a focal or patchy manner.58, 59, 60 Pyloric gland metaplasia occurs in NSAIDs-induced ileitis as well.
Other rare causes of ileitis in UC include bacterial overgrowth and ischemia. Primary involvement of the ileum by UC has also been proposed by some authorities.58, 59, 61 Regardless, from a pathologist’s perspective, a diagnosis of CD should be considered when a long stretch of ileal mucosa (generally >5–10 cm) is involved, is deeply ulcerating, patchy or segmental in distribution, shows established features of chronicity, or is associated with granulomas. If any one or more of these features are associated with radiologic abnormalities, such as thickening of the bowel wall or stricturing of the lumen, CD is the most likely diagnosis.
UC with Upper GI Involvement. Gastric and/or duodenal involvement has, rarely, been reported in association with UC.29, 30, 62, 63, 64, 65, 66 For instance, in a recent study by Lin et al,65 esophageal, gastric and duodenal biopsies in 69 UC patients were compared with 97 non-UC controls. In that study, UC patients showed a higher prevalence rate of focal gastritis, basal mucosal mixed inflammation, superficial plasmacytosis and diffuse chronic, or chronic active, duodenitis (Figure 4). In some circumstances, duodenal involvement may be severe and diffuse, and as a result, necessitate surgical resection. The cause of upper GI involvement in UC is unclear, and a diagnosis of the latter should only be considered in patients who have unequivocal UC in the distal colon, without any major CD features.
Patient with known UC, without ileitis, and without any major features of CD who developed a 15 cm segment of severe chronic active duodenitis. In this medium-power photograph of a portion of the duodenum, there is near complete villous atrophy, ulceration, diffuse lymphoplasmacytosis of the lamina propria, crypt distortion and basal plasmacytosis, all features consistent with involvement by UC. In other areas of the mucosa, there are foci of cryptitis and crypt abscesses. There was no evidence of CD, such as transmural lymphoid aggregates, fissuring ulceration, granulomas unrelated to ruptured crypts or segmental distribution of disease.
Crohn’s Disease with UC-Like Features
Up to 20% of CD patients show disease limited to the colon.1 A small percentage of patients with clinically and/or serologically defined CD, with involvement of the colon, or the colon and distal ileum, may show UC-like pathologic changes in their resection specimen, such as mucosal-only disease (without mural involvement), isolated rectal involvement, or diffuse colonic disease.67, 68, 69, 70 Patients with these features have been termed ‘superficial’ (UC-like) CD (Figure 5). Essentially, patients with superficial (UC-like) CD have either ambiguous, or CD-like features, clinically, and UC-like features pathologically. In these cases, a diagnosis of CD may be established by noting the presence of typical changes of CD in other regions of the GI tract, or by the presence of major features of CD in the colon, such as granulomas, rectal sparing from onset of disease, or most commonly, severe anal or perianal disease. In a recent study by Soucy et al,69 UC-like CD was noted in 14% and 13% of patients with isolated colonic CD and ileocolonic CD, respectively. Overall, patients with UC-like CD were younger in age and had a higher incidence of limited left-sided colitis compared with patients with classic CD. The outcome of patients with UC-like CD after colectomy and IPAA is controversial. In the study by Soucy et al, there was no difference in the frequency of development of adverse outcomes of the pouch, such as fistula formation, pouch anastomosis breakdown, chronic pouchitis or recurrence of disease, in patients with UC-like colonic CD compared with those with classic colonic CD. However, in another study of 21 CD patients with UC-like pancolitis at presentation, all of whom underwent a pouch procedure, only 14% had pouch complications that necessitated pouch resection, which is substantially lower than published rates of pouch complications in patients with classic features of CD in the colon.70 Thus, more research is needed in order to determine if patients with UC-like colonic CD can be treated safely and reliably with total colectomy and IPAA.
Failure to Recognize Non-IBD Mimics and Superimposed Diseases
Table 7 lists the most common, non-UC/non-CD types of ‘IBD’ that may mimic the pathologic changes of UC and/or CD in biopsies and/or resection specimens.7, 27 Table 8 lists the most common superimposed diseases that may develop in patients with established UC, which may result in changes in the pattern or distribution of inflammation that mimic CD. A complete review of the pathologic features of each of these disorders, and how each of them may mimic UC or CD, is beyond the scope of this review. However, certain general guidelines and principles are offered here. IBD patients who have a sudden change in their symptoms and signs, develop fulminant colitis, or sudden resistance to medical therapy, should be evaluated thoroughly for the accuracy of the diagnosis (of UC or CD) and for the presence of a secondary disorder, such as CMV infection, C. difficile-induced pseudomembranous colitis, ischemia or a drug reaction (eg, NSAIDs, ipilimumab and mycophenolate),71, 72, 73, 74, 75, 76, 77, 78, 79, 80 among others (Figure 6). IBD patients are at increased risk for CMV infection, and should always be considered in suddenly refractory IBD patients. In all, 21–34% of IBD patients with acute severe colitis, and 33–36% of steroid refractory patients have CMV detected in their colon.75, 76 Furthermore, the presence of superimposed CMV, in a UC patient, may induce a flare that is segmental in distribution and disproportionately severe in the right colon and/or ileum. Immunohistochemistry for CMV is the gold standard method of detection. Detection of CMV is important because antiviral therapy remission rates range from 67 to 100%.76
(a–d) Disorders that mimic IBD, or cause changes in the pattern and severity of inflammation in patients with known IBD. (a) Patient with known UC who developed C. difficile-associated pseudomembranous colitis and CMV infection, which caused the patient to become refractory to medical treatment. Classic C. difficile-associated pseudomembranes are seen in this image, which are occurring on a background of mucosa that is consistent with UC. (b) High-power magnification of one portion of the mucosa shows multiple CMV inclusions within stromal cells. (c) Ipilimumab-associated diffuse pancolitis with features similar to IBD. In this photograph, the mucosa shows diffuse ulceration and superficial fissuring ulceration. An associated inflammatory polyp is noted in the right side of the field. (d) Elderly patient with severe atherosclerotic disease developed segmental areas of severe chronic active colitis with ulceration, features that mimic IBD. In other areas of the resected colon, there are arterial thrombi involving small and medium-sized blood vessels in various stages of organization. This patient had no history of IBD before development of chronic recurrent ischemic colitis.
It is well known that patients with IBD, particularly those with UC, have an increased risk of intestinal ischemia.71, 72 Recently, it has become apparent that patients with clinically and histologically confirmed microscopic colitis, either lymphocytic or collagenous, at some point in the natural course of illness, may develop clinical and/or histologic features of IBD, particularly UC.81, 82 Whether the presence of microscopic colitis renders patients at increased risk for IBD is unknown. Conversely, patients with clinically and histologically established IBD may at some point during the course of their illness, develop either focal or diffuse histologic manifestations of microscopic colitis, and in some cases, this may be associated with non-bloody (watery) diarrhea and an absence of endoscopic abnormalities.83, 84, 85 Most patients with IBD sustain periods of inactive or quiescent disease. During the quiescent phase of disease, the bowel remains at risk for other diseases, particularly those that may be related to the treatment of IBD, such as microscopic colitis or drug-induced colitis. In addition, patients with established microscopic colitis, may show histologic features that mimic IBD, such as cryptitis, crypt abscesses, basal lymphoid aggregates, crypt distortion and Paneth cell metaplasia, all of which are typically mild and/or patchy in distribution, in contrast to IBD where these changes are more often diffuse (Figure 7).85
Patient with diffuse severe collagenous colitis. In this medium-power image, the crypts appear linear, but foreshortened, and there is evidence of plasmacytosis in the base of the mucosa similar to UC. In addition, there are superficial erosions and surface epithelial degeneration, thickening and irregularity of the subepithelial collagen layer, and multiple giant cells related to degenerated collagen, some forming loose granulomas.
Diverticular disease-associated colitis, also referred to as ‘segmental colitis,’ is a disorder of unknown etiology that causes a UC-like appearance to the mucosa in the interdiverticular, and even diverticular, mucosa in regions of bowel involved by diverticuli (Figure 8).86 Mucosal biopsies from this region are indistinguishable from UC.7 However, this disorder does not involve the rectum, and does not involve portions of the colon proximal to the region of diverticulosis, both of which are features that can be used to distinguish this disorder from UC.86, 87, 88
Medium-power image of a patient with diverticular disease-associated colitis showing involvement of the mucosa (only in the area of diverticular disease), and diverticular out-pouches as well. In this image, there is diffuse lymphoplasmacytosis of the lamina propria, loose granulomatous inflammation related to a ruptured crypt, basal plasmacytosis, and foreshortening and slight distortion of the crypts, similar to UC.
Rarely, acute diverticulitis may mimic CD in resection specimens.89, 90 This phenomenon may be recognized by the fact that CD-like changes are isolated to the segment of colon involved with diverticular disease. In one study of 29 patients with CD-like diverticulitis, only two developed CD, and both of these occurred in other regions of the bowel.89
As mentioned above, many types of drugs may cause chronic or chronic active colitis that mimics IBD, in both biopsy and resection specimens. Ipilimumab, a drug used for the treatment of metastatic melanoma, has been reported to show UC-like inflammatory changes in the colon.91 Mycophenolate, a drug used to prevent kidney allograft rejection, is also well known to induce chronic diarrhea and histologic features that mimic IBD, particularly CD.78 Mycophenolate-induced chronic colitis often shows prominent apoptosis, apoptotic crypt abscesses and increased eosinophilic inflammation in the absence of lymphoplasmacytosis.78 NSAIDs may cause focal or diffuse changes that mimic UC in biopsies and resection specimens, but in these patients, other portions of the GI tract are usually involved as well.92
Attempt to Distinguish UC from CD in Biopsies
Mucosal biopsy specimens are typically superficial in nature, and, thus, provide little information regarding important histologic features used to discriminate UC from CD, such as depth of disease activity, the presence or absence of transmural inflammation or the type of ulcers present. Unfortunately, the mucosal features of UC and CD are often indistinguishable, and thus, none can be used to reliably separate these two disorders. Features typically associated with CD, such as relative or absolute rectal sparing, skip areas of inflammation, and ileal involvement, may also occur in UC, particularly in previously treated patients. Uneven healing of disease, and/or the therapeutic effects of drugs or enemas used for treatment, may cause discontinuous (patchy) inflammation mimicking CD.24, 33, 34, 35 As a result, in UC patients who have been treated medically, pathologists cannot consider either patchiness of disease or rectal sparing as features indicative of CD. Thus, in previously treated patients, unless the patient reveals evidence of anal or perianal CD, granulomas unrelated to ruptured crypts or foreign material, or definite evidence of CD-like chronic active ileitis or upper GI involvement, it is virtually impossible to distinguish UC from CD in biopsies. Therefore, the major role of pathologists in this setting is to help clinicians determine the true extent and distribution of disease, the severity of disease, and the presence or absence of dysplasia or cancer.23 Surgical pathology signouts should remain ‘generic,’ utilizing terminology that provides this information without committing to a specific diagnosis (of UC or CD). An example of a typical colonic mucosal biopsy signout of an IBD patient is ‘severe chronic active colitis, no granulomas or dypslasia identified.’ As mentioned above, if granulomas (unrelated to ruptured crypts or foreign material) are identified in one or more biopsies, or if CD-like chronic active ileitis or upper GI involvement is present, then a note indicating ‘Crohn’s disease is favored’ or ‘consistent with Crohn’s disease’ (if the patient has already had this diagnosis established clinically) is considered sufficient.
In contrast, in previously untreated IBD patients, pathologists may be able to offer more guidance to the clinician regarding the patients specific diagnosis. In this instance, individual biopsies should also follow the same ‘generic’ reporting format as described above for treated IBD patients. However, if patchy disease, rectal sparing (in an adult), CD-like ileal or upper GI involvement, granulomas or anal/perianal CD are identified, then a note indicating ‘The findings are suggestive (or consistent) with CD’ is considered reasonable. Alternatively, if none of these features are present, but, in contrast, the colon biopsies reveal either diffuse colon involvement, or continuous (non-patchy) left-sided or sub-total colitis, and an absence of anal/perianal disease, a note indicating that ‘UC is favored’ is also reasonable. Since CD may, in fact, reveal all of these features in a small proportion of patients, indicating that ‘UC is favored’ leaves open the possibility of other disorders, such as CD. Regardless of whether the patient has been treated before colonoscopy, IC should never be diagnosed (or ‘favored’) by pathologists on the basis of analysis of mucosal biopsies of the colon and ileum.
Attempt to Change the Diagnosis of UC to CD Based on Pouch Complications
A discussion of the clinical manifestations, etiology and natural history of pouchitis is beyond the scope of this review. However, a few comments are important with regard to IBD pathology. Up to 50% of UC patients who undergo an IPAA procedure develop at least one episode of symptomatic pouchitis within the first year after surgery.79, 93, 94, 95 A diagnosis of pouchitis is based on a combination of specific clinical, endoscopic and pathologic features.95 Histologically, pouchitis most often shows active inflammation in the lamina propria and crypt epithelium, either with or without ulceration.94, 95 A mild degree of architectural distortion, villous shortening, increased chronic inflammation, transmural inflammation and even pseudopyloric metaplasia may develop in UC patients with pouchitis, especially in the early post-operative period.96, 97, 98, 99 Some of these changes may represent a form of adaptation of the mucosa to the new luminal environment in contact with pouch mucosa.97, 99 Unfortunately, some patients with treatment unresponsive pouchitis may develop clinical and pathologic complications that mimic CD.96 These include strictures, pouch stenosis or fistulas, granulomas, perianal fissures and fistulas, and even extraintestinal manifestations such as arthritis or pyoderma gangrenosum. In these settings, pathologists may question the validity of their original diagnosis of UC and entertain the possibility of CD instead. Several studies have addressed this issue and have found that, in most instances, the patients original diagnosis of UC is, in fact, correct.96, 98, 100, 101 For instance, Goldstein et al96 evaluated eight cases of presumed UC who developed one or more CD-like pouch complications after an IPAA procedure. The histologic findings in the patient’s original colectomy specimen were indistinguishable from those of UC patients who did not develop complications, and, therefore, this author concluded that CD-like complications do not necessarily represent a mistaken diagnosis of UC. In another study by Subramani et al,100 no pathologic features could be identified that reliably distinguished UC-related refractory pouchitis from CD of the pouch. Non-necrotic epithelial granulomas unassociated with ruptured crypts may also be seen in pouch biopsies from patients with established UC and does not necessarily imply CD.96 However, this is controversial, since in one study published only in abstract form, most patients with granulomas of the pouch were subsequently reclassified as CD based upon re-review of the patient’s colectomy specimen and follow-up information.98 One study suggested that ulcers in the afferent limb of patients who had an IPAA procedure were predictive of CD.102 Thus, when faced with a patient with severe pouch complications, knowledge of the patient’s prior and current clinical, radiologic, endoscopic and pathologic information, the latter both in pouch and in pre-pouch proximal ileal mucosa, should be carefully examined before changing the patient’s original diagnosis of UC to CD.102 Under these circumstances, evaluation of the patient’s prior biopsies and colectomy specimens for evidence of CD is considered essential.
Use of serology in IC
There are a variety of serologic markers that have been tested in patients with UC, and in some cases, IC as well.103, 104, 105, 106, 107, 108, 109, 110 Markers that have been most extensively studied include ANCA, ASCA, OMPc, cBIR-1 and anti I2. Of these markers, ANCA and ASCA have been most extensively studied. For instance, ANCA is detected in the serum of 60–70% of patients with UC, but in only 10–40% of CD patients.106, 109, 110 Conversely, ASCA is present in 50–60% of CD patients, but in <10% of UC patients.106, 109, 110 As a serum marker for CD, ASCA has a reported sensitivity of approximately 60%, and specificity over 90%.110 In a meta-analysis designed to evaluate the diagnostic usefulness of ANCA and ASCA in IBD patients, these serologic tests were shown to be quite specific, but not very sensitive, in distinguishing CD from UC.107 In that study, a combination of ASCA positivity and ANCA negativity offered the best overall sensitivity and specificity for CD (55% and 43%, respectively). A higher degree of sensitivity and specificity has been reported in pediatric patients. OMPc has been correlated with an increased risk of fibrostenosing and internal penetrating CD (present in about 55% of CD cases) and cBIR-1 in about 44% of cases and anti-I2 in about 54% of cases.108, 109 All of these three peptides are present in <10% of UC patients. Unfortunately, these serologic tests have not been extensively studied in diagnostically difficult cases, such as in patients with IC.103, 105, 106, 110 In one prospective follow-up study by Joossens et al,110 the value of ANCA and ASCA serologic markers were evaluated in 97 IBD patients with IC. In that study, 49% of IC patients were negative for both ANCA and ASCA.111 The remaining patients who had one or both of these peptides positive, ANCA and ASCA helped establish a definite diagnosis of CD (ASCA positive and ANCA negative) or UC (ASCA negative and ANCA positive) in only a minority of patients. Unfortunately, in most patients there was insufficient clinical, radiologic or pathologic information available in order to accurately classify IC patients as having either CD or UC. The sensitivities and specificities of ASCA/ANCA combinations ranged from 67% to 78%, respectively. Therefore, based on this one study, there appears to be limited clinical utility for these markers in separating IC cases into CD or UC. Further studies utilizing larger panels of serologic tests in patients with known UC and CD, and in those with IC needs to be performed in order to determine the true value of serologic tests in patients with IC.
Outcome of patients with IC
There have been many studies that have evaluated outcome of IC patients after total colectomy and IPAA.9, 10, 14, 112, 113, 114, 115, 116, 117 Some of these are listed in Table 9. Unfortunately, the results among these mainly retrospective studies are quite variable, and this is likely related to the fact that these studies utilized heterogeneous study populations, and inconsistent and/or poorly defined inclusion criteria for IC. Many studies lacked sufficient follow-up information. Regardless, pouch failure rates in patients with IC average about 20%.14 This value is, not surprisingly, intermediate in value between patients with UC (approximately 10%) and those with CD (30–60%), but is closer to the former. The finding of pouch failure rates in IC patients that range in between UC and CD is not surprising given that most published IC study groups consist of a mixture of true UC and CD patients. However, many studies failed to show a significant difference in outcome between patients with IC and UC, and this is likely related to the fact that most IC patients either have, or end up being diagnosed with, UC.9, 14, 112, 115, 116 For instance, in a study by Delaney et al,116 of 79 IC patients and 565 UC patients, all of whom have had a total colectomy and IPAA procedure, there was no significant differences in the frequency of pouch strictures, fistulas, pouchitis, pouch loss or regarding the development of CD upon follow-up, between these two patient groups. In a large follow-up study of 82 patients with IC and 1437 patients with UC, all of which who had an IPAA procedure, 12 of the initial 82 patients (15%) were ultimately diagnosed with CD.46 When these patients were removed from the analysis, there was a statistically similar rate of pelvic sepsis, pouch fistula, pouch failure or any one or more of the above-described pouch complications, in patients with a persistent diagnosis of IC after follow-up compared with patients with known UC. The pouch complication rates were 49% and 48% in these two groups, respectively. Similar results were detected by Pishori et al114 (pouch complications; IC: 31% and UC: 38%) and Rudolph et al115 (pouch failure rates; IC: 0% and UC: 8%). Gramlich et al10 evaluated 115 patients with IC compared with 231 UC controls. After a more detailed pathologic analysis, IC patients were separated into those in which UC was favored, those in which neither diagnosis was favored and those in which CD was favored (99, 8 and 8 cases, respectively). In that study, only patients with IC who developed deep ulcers, (which were suggestive of CD) developed unequivocal CD upon follow-up, pelvic abscesses or complex fistulas. None of the patients with IC who lacked deep ulcers had an increased risk of pouch failure, above the rate of the control (UC) patients. This study also further emphasizes that in the majority of IC patients, after careful analysis, a diagnosis of UC is usually favored. Finally, in one study by Meucci et al,118 50 of 1113 IBD patients were diagnosed with IC (4.6%) clinically (before surgical resection). Upon follow-up, 73% of the IC patients had a definitive diagnosis of either UC or CD established (54% UC and 46% CD). The cumulative probability of establishing a final diagnosis of either UC or CD was 80% after 8 years. However, in that study, a diagnosis of IC was based on clinical, radiologic and endoscopic (including biopsy) parameters, but not resection specimens, a method of diagnosis of IC that is highly discouraged.
Summary
IC is not a discrete disease entity. It represents an interim diagnosis that pathologists make when faced with a UC-like colonic resection specimen that shows one or more CD-like features. Most causes of uncertainty are due to overlapping features as a result of fulminant colitis, insufficient clinical, radiologic, endoscopic or pre-resection biopsy information, or failure to recognize unusual pathologic variants of UC that mimic CD, and variants of CD that mimic UC. Features such as transmural lymphoid aggregates, deep fissuring ulceration, granulomas (unrelated to infection, foreign material or ruptured crypts etc) and rectal sparing before treatment, are considered major features of CD. Any one or more of these features identified in a colonic resection specimen from an IBD patient should evoke strong suspicion for CD. Not all cases of IBD are due to UC and CD. Other diseases, such as drug reactions, certain infections, ischemia, diverticulitis-associated colitis and even radiation colitis, can mimic IBD and should be considered in the differential diagnosis of diagnostically difficult ‘IBD’ cases. Furthermore, superimposed diseases and infections in patients with previously established UC can render the patient difficult to diagnose accurately because of the formation of a CD-like pattern of inflammation in the colon. A diagnosis of IC should never be made clinically, or in pre-resection mucosal biopsies. Caution should be used when changing an IBD diagnosis based on pouch complications. Ultimately, the majority of IC cases represent UC, and, thus, most of these patients can be treated safely with a colectomy combined with an IPAA procedure.
References
Silverberg MS, Satsangi J, Ahmad T et al. Toward an integrated clinical, molecular and serological classification of inflammatory bowel disease: report of a working party of the 2005 Montreal World Congress of Gastroenterology. Can J Gastroenterol 2005;19 Suppl A:5A–36A
Geboes K, Van Eyken P . Inflammatory bowel disease unclassified and indeterminate colitis: the role of the pathologist. J Clin Pathol 2009;62:201–205
Yantiss RK, Odze RD . Diagnostic difficulties in inflammatory bowel disease pathology. Histopathology 2006;48:116–132
Geboes K, Colombel JF, Greenstein A et al. Indeterminate colitis: a review of the concept—what’s in a name?. Inflamm Bowel Dis 2008;14:850–857
Tremaine WJ . Is indeterminate colitis determinable?. Curr Gastroenterol Rep 2012;14:162–165
Farmer M, Petras RE, Hunt LE et al. The importance of diagnostic accuracy in colonic inflammatory bowel disease. Am J Gastroenterol 2000;95:3184–3188
Yantiss RK, Odze RD . Pitfalls in the interpretation of nonneoplastic mucosal biopsies in inflammatory bowel disease. Am J Gastroenterol 2007;102:890–904
Geboes K . Crohn’s disease, ulcerative colitis or indeterminate colitis–how important is it to differentiate?. Acta Gastroenterol Belg 2001;64:197–200
Yu CS, Pemberton JH, Larson D . Ileal pouch-anal anastomosis in patients with indeterminate colitis: long-term results. Dis Colon Rectum 2000;43:1487–1496
Gramlich T, Delaney CP, Lynch AC et al. Pathological subgroups may predict complications but not late failure after ileal pouch-anal anastomosis for indeterminate colitis. Colorectal Dis 2003;5:315–319
Kent TH, Ammon RK, DenBesten L . Differentiation of ulcerative colitis and regional enteritis of colon. Arch Pathol 1970;89:20–29
Price AB . Overlap in the spectrum of non-specific inflammatory bowel disease—‘colitis indeterminate’. J Clin Pathol 1978;31:567–577
Yantiss RK, Farraye FA, O’Brien MJ et al. Prognostic significance of superficial fissuring ulceration in patients with severe ‘indeterminate’ colitis. Am J Surg Pathol 2006;30:165–170
McIntyre PB, Pemberton JH, Wolff BG et al. Indeterminate colitis. long-term outcome in patients after ileal pouch-anal anastomosis. Dis Colon Rectum 1995;38:51–54
Wolff BG . Is ileoanal the proper operation for indeterminate colitis: the case for. Inflamm Bowel Dis 2002;8:362–365discussion 368-9
Odze RD . Pathology of indeterminate colitis. J Clin Gastroenterol 2004;38:S36–S40
Heppell J, Farkouh E, Dube S et al. Toxic megacolon. An analysis of 70 cases. Dis Colon Rectum 1986;29:789–792
Mahadeva U, Martin JP, Patel NK et al. Granulomatous ulcerative colitis: a re-appraisal of the mucosal granuloma in the distinction of Crohn’s disease from ulcerative colitis. Histopathology 2002;41:50–55
Swan NC, Geoghegan JG, O'Donoghue DP et al. Fulminant colitis in inflammatory bowel disease: detailed pathologic and clinical analysis. Dis Colon Rectum 1998;41:1511–1515
Matsui T, Yao T, Sakurai T et al. Clinical features and pattern of indeterminate colitis: Crohn’s disease with ulcerative colitis-like clinical presentation. J Gastroenterol 2003;38:647–655
Loftus EV . Clinical epidemiology of inflammatory bowel disease: incidence, prevalence, and environmental influences. Gastroenterology 2004;126:1504–1517
Carucci LR, Levine MS . Radiographic imaging of inflammatory bowel disease. Gastroenterol Clin North Am 2002;31:93–117ix
Odze RD . IBD: role of the pathologist in the diagnosis and management of IBD. Nat Rev Gastroenterol Hepatol 2013;10:625–626
Odze R, Antonioli D, Peppercorn M et al. Effect of topical 5-aminosalicylic acid (5-ASA) therapy on rectal mucosal biopsy morphology in chronic ulcerative colitis. Am J Surg Pathol 1993;17:869–875
Warren BF, Shepherd NA, Price AB et al. Importance of cryptolytic lesions and pericryptal granulomas in inflammatory bowel disease. J Clin Pathol 1997;50:880–881
Petri M, Poulsen SS, Christensen K et al. The incidence of granulomas in serial sections of rectal biopsies from patients with Crohn’s disease. Acta Pathol Microbiol Immunol Scand A 1982;90:145–147
Patil D, Greenson J, Odze R . Inflammatory disorders of the large intestineIn: Odze R, Goldblum J, (eds) Surgical Pathology of the GI Tract, Liver, Biliary Tract, and Pancreas 3rd edn. Elsevier: Philadelphia 2014
Farmer RG, Easley KA, Rankin GB . Clinical patterns, natural history, and progression of ulcerative colitis. A long-term follow-up of 1116 patients. Dig Dis Sci 1993;38:1137–1146
Tobin JM, Sinha B, Ramani P et al. Upper gastrointestinal mucosal disease in pediatric Crohn disease and ulcerative colitis: a blinded, controlled study. J Pediatr Gastroenterol Nutr 2001;32:443–448
Sonnenberg A, Melton SD, Genta RM . Frequent occurrence of gastritis and duodenitis in patients with inflamm bowel dis. Inflamm Bowel Dis 2011;17:39–44
Ruuska T, Vaajalahti P, Arajarvi P et al. Prospective evaluation of upper gastrointestinal mucosal lesions in children with ulcerative colitis and Crohn’s disease. J Pediatr Gastroenterol Nutr 1994;19:181–186
Lenaerts C, Roy CC, Vaillancourt M et al. High incidence of upper gastrointestinal tract involvement in children with Crohn disease. Pediatrics 1989;83:777–781
Kleer CG, Appelman HD . Ulcerative colitis: patterns of involvement in colorectal biopsies and changes with time. Am J Surg Pathol 1998;22:983–989
Bernstein CN, Shanahan F, Anton PA et al. Patchiness of mucosal inflammation in treated ulcerative colitis: a prospective study. Gastrointest Endosc 1995;42:232–237
Kim B, Barnett JL, Kleer CG et al. Endoscopic and histological patchiness in treated ulcerative colitis. Am J Gastroenterol 1999;94:3258–3262
Markowitz J, Kahn E, Grancher K et al. Atypical rectosigmoid histology in children with newly diagnosed ulcerative colitis. Am J Gastroenterol 1993;88:2034–2037
Glickman JN, Bousvaros A, Farraye FA et al. Pediatric patients with untreated ulcerative colitis may present initially with unusual morphologic findings. Am J Surg Pathol 2004;28:190–197
Washington K, Greenson JK, Montgomery E et al. Histopathology of ulcerative colitis in initial rectal biopsy in children. Am J Surg Pathol 2002;26:1441–1449
Robert ME, Tang L, Hao LM et al. Patterns of inflammation in mucosal biopsies of ulcerative colitis: perceived differences in pediatric populations are limited to children younger than 10 years. Am J Surg Pathol 2004;28:183–189
D'Haens G, Geboes K, Peeters M et al. Patchy cecal inflammation associated with distal ulcerative colitis: a prospective endoscopic study. Am J Gastroenterol 1997;92:1275–1279
Okawa K, Aoki T, Sano K et al. Ulcerative colitis with skip lesions at the mouth of the appendix: a clinical study. Am J Gastroenterol 1998;93:2405–2410
Yang SK, Jung HY, Kang GH et al. Appendiceal orifice inflammation as a skip lesion in ulcerative colitis: an analysis in relation to medical therapy and disease extent. Gastrointest Endosc 1999;49:743–747
Davison AM, Dixon MF . The appendix as a ‘skip lesion’ in ulcerative colitis. Histopathology 1990;16:93–95
Groisman GM, George J, Harpaz N . Ulcerative appendicitis in universal and nonuniversal ulcerative colitis. Mod Pathol 1994;7:322–325
Mutinga ML, Odze RD, Wang HH et al. The clinical significance of right-sided colonic inflammation in patients with left-sided chronic ulcerative colitis. Inflamm Bowel Dis 2004;10:215–219
Robert ME, Skacel M, Ullman T et al. Patterns of colonic involvement at initial presentation in ulcerative colitis: a retrospective study of 46 newly diagnosed cases. Am J Clin Pathol 2004;122:94–99
Spiliadis CA, Spiliadis CA, Lennard-Jones JE . Ulcerative colitis with relative sparing of the rectum. clinical features, histology, and prognosis. Dis Colon Rectum 1987;30:334–336
Ladefoged K, Munck LK, Jorgensen F et al. Skip inflammation of the appendiceal orifice: a prospective endoscopic study. Scand J Gastroenterol 2005;40:1192–1196
Kanda K, Kume K, Yoshikawa I et al. [A case of non-steroidal anti-inflammatory drug-induced colitis with granulomas. Nihon Shokakibyo Gakkai Zasshi 2002;99:289–294
Pulimood AB, Peter S, Ramakrishna B et al. Segmental colonoscopic biopsies in the differentiation of ileocolic tuberculosis from Crohn’s disease. J Gastroenterol Hepatol 2005;20:688–696
Mayorga M, Castro F, Fernandez F et al. Radiohistology and histochemistry of barium granuloma of the colon and rectum. Histol Histopathol 1992;7:625–628
Lee FD, Maguire C, Obeidat W et al. Importance of cryptolytic lesions and pericryptal granulomas in inflammatory bowel disease. J Clin Pathol 1997;50:148–152
Kapuller LL, Konovich EA . Nonspecific granulomatous inflammation in Crohn’s disease. Arkh Patol 2012;74:57–60
Denoya P, Canedo J, Berho M et al. Granulomas in Crohn’s disease: does progression through the bowel layers affect presentation or predict recurrence?. Colorectal dis 2011;13:1142–1147
Mc CF, Bargen JA . Involvement of the ileum in chronic ulcerative colitis. New Eng J Med 1949;240:119–127
Haskell H, Andrews CW Jr, Reddy SI et al. Pathologic features and clinical significance of ‘backwash’ ileitis in ulcerative colitis. Am J Surg Pathol 2005;29:1472–1481
Goldstein N, Dulai M . Contemporary morphologic definition of backwash ileitis in ulcerative colitis and features that distinguish it from Crohn disease. Am J Clin Pathol 2006;126:365–376
Abdelrazeq AS, Wilson TR, Leitch DL et al. Ileitis in ulcerative colitis: is it a backwash?. Dis Colon Rectum 2005;48:2038–2046
Saltzstein SL, Rosenberg BF . Ulcerative colitis of the ileum, and regional enteritis of the colon. A comparative histopathologic study. Am J Clin Pathol 1963;40:610–623
Makrauer F, Golden K, Friedman S et al. Prevalence and significance of ileal inflammation in ulcerative colitis: a prospective controlled study. Gastroenterology 2013;144:S-769
Yamamoto T, Maruyama Y, Umegae S et al. Mucosal inflammation in the terminal ileum of ulcerative colitis patients: endoscopic findings and cytokine profiles. Dig Liver Dis 2008;40:253–259
Valdez R, Appelman HD, Bronner MP et al. Diffuse duodenitis associated with ulcerative colitis. Am J Surg Pathol 2000;24:1407–1413
Terashima S, Hoshino Y, Kanzaki N et al. Ulcerative duodenitis accompanying ulcerative colitis. J Clin Gastroenterol 2001;32:172–175
Ikeuchi H, Hori K, Nishigami T et al. Diffuse gastroduodenitis and pouchitis associated with ulcerative colitis. World J Gastroenterol 2006;12:5913–5915
Lin J, McKenna BJ, Appelman HD . Morphologic findings in upper gastrointestinal biopsies of patients with ulcerative colitis: a controlled study. Am J Surg Pathol 2010;34:1672–1677
Yao K, Yao T, Iwashita A et al. Microaggregate of immunostained macrophages in noninflamed gastroduodenal mucosa: a new useful histological marker for differentiating Crohn’s colitis from ulcerative colitis. Am J Gastroenterol 2000;95:1967–1973
McQuillan ACAH . Superficial Crohn’s dsiease: a study of 10 patients. Surg Pathol 1989;2:231–239
Harpaz N, Friedman SGJ . Superifical Crohn’s colitis: pathological and clinical features including long-term follow-up. Mod Pathol 2001;14:86A
Soucy G, Wang HH, Farraye FA et al. Clinical and pathological analysis of colonic Crohn’s disease, including a subgroup with ulcerative colitis-like features. Mod Pathol 2012;25:295–307
Morpurgo E, Petras R, Kimberling J et al. Characterization and clinical behavior of Crohn’s disease initially presenting predominantly as colitis. Dis Colon Rectum 2003;46:918–924
Wilson MZ, Connelly TM, Tinsley A et al. Ulcerative colitis is associated with an increased risk of venous thromboembolism in the postoperative period: the results of a matched cohort analysis. Ann Surgadvance online publication, 30 June 2014 (e-pub ahead of print)
Novacek G, Haumer M, Schima W et al. Aortic mural thrombi in patients with inflammatory bowel disease: report of two cases and review of the literature. Inflamm Bowel Dis 2004;10:430–435
Garcia-Osogobio S, Takahashi T, Gamboa-Dominguez A et al. Toxic pseudomembranous colitis in a patient with ulcerative colitis. Inflamm Bowel Dis 2000;6:188–190
Wang A, Takeshima F, Ikeda M et al. Ulcerative colitis complicating pseudomembranous colitis of the right colon. J Gastroenterol 2002;37:309–312
Hommes DW, Sterringa G, van Deventer SJ et al. The pathogenicity of cytomegalovirus in inflammatory bowel disease: a systematic review and evidence-based recommendations for future research. Inflamm Bowel Dis 2004;10:245–250
Kambham N, Vij R, Cartwright CA et al. Cytomegalovirus infection in steroid-refractory ulcerative colitis: a case-control study. Am J Surg Pathol 2004;28:365–373
Kishore J, Ghoshal U, Ghoshal UC et al. Infection with cytomegalovirus in patients with inflammatory bowel disease: prevalence, clinical significance and outcome. J Med Microbiol 2004;53:1155–1160
Star KV, Ho VT, Wang HH et al. Histologic features in colon biopsies can discriminate mycophenolate from GVHD-induced colitis. Am J Surg Pathol 2013;37:1319–1328
Papadakis KA, Tung JK, Binder SW et al. Outcome of cytomegalovirus infections in patients with inflammatory bowel disease. Am J Gastroenterol 2001;96:2137–2142
McCurdy JD, Jones A, Enders FT et al. A model for identifying cytomegalovirus in patients with inflammatory bowel disease. Clin Gasstroenterol Hepatol 2014pii: S1542-3565(14)00926-4 doi:10.1016/j.cgh.2014.05.026 (e-pub ahead of print)
Ayata G, Ithamukkala S, Sapp H et al. Prevalence and significance of inflammatory bowel disease-like morphologic features in collagenous and lymphocytic colitis. Am J Surg Pathol 2002;26:1414–1423
Saurine TJ, Brewer JM, Eckstein RP . Microscopic colitis with granulomatous inflammation. Histopathology 2004;45:82–86
Goldstein NS, Gyorfi T . Focal lymphocytic colitis and collagenous colitis: patterns of Crohn’s colitis?. Am J Surg Pathol 1999;23:1075–1081
Pokorny CS, Kneale KL, Henderson CJ . Progression of collagenous colitis to ulcerative colitis. J Clin Gastroenterol 2001;32:435–438
Schulte S, Khor T, Hagen C et al. Long term outcome study of patients with both inflammatory bowel disease and microscopic colitis during the course of illness. Mod Pathol 2013;26:178
Peppercorn MA . Drug-responsive chronic segmental colitis associated with diverticula: a clinical syndrome in the elderly. Am J Gastroenterol 1992;87:609–612
Imperiali G, Meucci G, Alvisi C et al. Segmental colitis associated with diverticula: a prospective study. gruppo di studio per le malattie infiammatorie intestinali (GSMII). Am J Gastroenterol 2000;95:1014–1016
Makapugay LM, Dean PJ . Diverticular disease-associated chronic colitis. Am J Surg Pathol 1996;20:94–102
Goldstein NS, Leon-Armin C, Mani A . Crohn’s colitis-like changes in sigmoid diverticulitis specimens is usually an idiosyncratic inflammatory response to the diverticulosis rather than Crohn’s colitis. Am J Surg Pathol 2000;24:668–675
Petros JG, Happ RA . Crohn’s colitis in patients with diverticular disease. Am J Gastroenterol 1991;86:247–248
Garcia-Varona A, Odze RD, Makrauer F . Lymphocytic colitis secondary to ipilimumab treatment. Inflamm Bowel Dis 2013;19:E15–E16
Puspok A, Kiener HP, Oberhuber G . Clinical, endoscopic, and histologic spectrum of nonsteroidal anti-inflammatory drug-induced lesions in the colon. Dis Colon Rectum 2000;43:685–691
Hurst RD, Molinari M, Chung TP et al. Prospective study of the incidence, timing and treatment of pouchitis in 104 consecutive patients after restorative proctocolectomy. Arch Surg 1996;131:497–500discussion 501-2
Stocchi L, Pemberton JH . Pouch and pouchitis. Gastroenterol Clin North Am 2001;30:223–241
Shen B, Achkar JP, Lashner BA et al. Endoscopic and histologic evaluation together with symptom assessment are required to diagnose pouchitis. Gastroenterology 2001;121:261–267
Goldstein NS, Sanford WW, Bodzin JH . Crohn’s-like complications in patients with ulcerative colitis after total proctocolectomy and ileal pouch-anal anastomosis. Am J Surg Pathol 1997;21:1343–1353
Fruin AB, El-Zammer O, Stucchi AF et al. Colonic metaplasia in the ileal pouch is associated with inflammation and is not the result of long-term adaptation. J Gastrointest Surg 2003;7:246–253discussion 253-4
MacNeill K, Guindi M, Riddell RH . Is transmural inflammation in the ileoanal pouch significant?. Mod Pathol 2004;17:123A
Apel R, Cohen Z, Andrews CW Jr et al. Prospective evaluation of early morphological changes in pelvic ileal pouches. Gastroenterology 1994;107:435–443
Subramani K, Harpaz N, Bilotta J et al. Refractory pouchitis: does it reflect underlying Crohn’s disease?. Gut 1993;34:1539–1542
Korsgen S, Keighley MR . Causes of failure and life expectancy of the ileoanal pouch. Int J Colorectal Dis 1997;12:4–8
Wolf JM, Achkar JP, Lashner BA et al. Afferent limb ulcers predict Crohn’s disease in patients with ileal pouch-anal anastomosis. Gastroenterology 2004;126:1686–1691
Kekilli M, Beyazit Y, Tas A et al. Atypical pANCA as a marker of indeterminate colitis for the prediction of ulcerative colitis and Crohn’s disease. Wien Klin Wochenschr 2013;125:279–282
Joossens S, Colombel JF, Landers C et al. Anti-outer membrane of porin C and anti-I2 antibodies in indeterminate colitis. Gut 2006;55:1667–1669
Castillo S, Ramaiah B, Blum S et al. The value of serologic markers in indeterminate colitis: a prospective follow-up study. Gastroenterology 2003;125:999 author reply 999-1000
Papadakis KA, Targan SR . Serologic testing in inflammatory bowel disease: its value in indeterminate colitis. Curr Gastroenterol Rep 1999;1:482–485
Reese GE, Constantinides VA, Simillis C et al. Diagnostic precision of anti-saccharomyces cerevisiae antibodies and perinuclear antineutrophil cytoplasmic antibodies in inflammatory bowel disease. Am J Gastroenterol 2006;101:2410–2422
Targan SR, Landers CJ, Yang H et al. Antibodies to CBir1 flagellin define a unique response that is associated independently with complicated Crohn’s disease. Gastroenterology 2005;128:2020–2028
Zholudev A, Zurakowski D, Young W et al. Serologic testing with ANCA, ASCA, and anti-OmpC in children and young adults with Crohn’s disease and ulcerative colitis: diagnostic value and correlation with disease phenotype. Am J Gastroenterol 2004;99:2235–2241
Joossens S, Reinisch W, Vermeire S et al. The value of serologic markers in indeterminate colitis: a prospective follow-up study. Gastroenterology 2002;122:1242–1247
Silverberg MS, Satsangi J, Ahmad T et al. Toward an integrated clinical, molecular and serological classification of inflammatory bowel disease: report of a working party of the 2005 montreal world congress of gastroenterology. Can J Gastroenterol 2005;19 Suppl A:5a–36a
Brown CJ, Maclean AR, Cohen Z et al. Crohn’s disease and indeterminate colitis and the ileal pouch-anal anastomosis: outcomes and patterns of failure. Dis Colon Rectum 2005;48:1542–1549
Tekkis PP, Heriot AG, Smith O et al. Long-term outcomes of restorative proctocolectomy for Crohn’s disease and indeterminate colitis. Colorectal Dis 2005;7:218–223
Pishori T, Dinnewitzer A, Zmora O et al. Outcome of patients with indeterminate colitis undergoing a double-stapled ileal pouch-anal anastomosis. Dis Colon Rectum 2004;47:717–721
Rudolph WG, Uthoff SM, McAuliffe TL et al. Indeterminate colitis: the real story. Dis Colon Rectum 2002;45:1528–1534
Delaney CP, Remzi FH, Gramlich T et al. Equivalent function, quality of life and pouch survival rates after ileal pouch-anal anastomosis for indeterminate and ulcerative colitis. Ann Surg 2002;236:43–48
Schoetz JDJ . Is ileoanal the proper operation for indeterminate colitis: the case against. Inflamm Bowel Dis 2002;8:366–367discussion 368-9
Meucci G, Bortoli A, Riccioli FA et al. Frequency and clinical evolution of indeterminate colitis: a retrospective multi-centre study in northern italy. GSMII (gruppo di studio per le malattie infiammatorie intestinali). Eur J Gastroenterol Hepatol 1999;11:909–913
Dayton MT, Larsen KR, Christiansen DD . Similar functional results and complications after ileal pouch-anal anastomosis in patients with indeterminate vs ulcerative colitis. Arch Surg 2002;137:690–694
Murrell ZA, Melmed GY, Ippoliti A et al. A prospective evaluation of the long-term outcome of ileal pouch-anal anastomosis in patients with inflammatory bowel disease-unclassified and indeterminate colitis. Dis Colon Rectum 2009;52:872–878
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The author declares no conflict of interest.
Rights and permissions
About this article
Cite this article
Odze, R. A contemporary and critical appraisal of ‘indeterminate colitis’. Mod Pathol 28 (Suppl 1), S30–S46 (2015). https://doi.org/10.1038/modpathol.2014.131
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/modpathol.2014.131
This article is cited by
-
The role of biopsy protocol in inflammatory bowel disease: getting the diagnosis right first time
Internal and Emergency Medicine (2023)
-
Racial or ethnic differences on treatment adherence and persistence among patients with inflammatory bowel diseases initiated with biologic therapies
BMC Gastroenterology (2022)
-
Non-celiac wheat sensitivity: rationality and irrationality of a gluten-free diet in individuals affected with non-celiac disease: a review
BMC Gastroenterology (2021)
-
The incidence and prevalence of inflammatory bowel disease in UK primary care: a retrospective cohort study of the IQVIA Medical Research Database
BMC Gastroenterology (2021)
-
Diagnostic dilemmas in chronic inflammatory bowel disease
Virchows Archiv (2018)