Abstract
Oncotype DX™ is a commercially available reverse transcriptase-polymerase chain reaction based assay that provides a Recurrence Score (RS) and has been shown to provide prognostic and predictive information in estrogen receptor-positive lymph node-negative breast cancers. Independent studies of its utility in routine practice are lacking. Slides and surgical pathology reports from 42 cases of breast carcinomas evaluated by Oncotype DX™ were retrospectively reviewed to determine patient age, tumor size, histologic grade, estrogen and progesterone receptor (ER and PR) and ERBB2 (HER-2/neu) data, with ER and PR reported as a semi-quantitative score reflecting both intensity of staining and proportion of positive cells. We show here that Recurrence Score is significantly correlated with tubule formation, nuclear grade, mitotic count, ER immunohistochemical score, PR immunohistochemical score, and HER-2/neu status, and that the equation RS=13.424+5.420 (nuclear grade) +5.538 (mitotic count) −0.045 (ER immunohistochemical score) −0.030 (PR immunohistochemical score) +9.486 (HER-2/neu) predicts the Recurrence Score with an R2 of 0.66, indicating that the full model accounts for 66% of the data variability. Although the Oncotype DX™ Recurrence Score holds potential, further validation of its independent value beyond that of histopathologic analysis is necessary before it can be implemented in clinical decision making.
Similar content being viewed by others
Main
Breast cancer is the most frequent cancer and second most frequent cause of cancer death among women, with an estimated 178,480 new cases and 40,460 deaths in 2007.1 Approximately 50% of breast cancer cases are lymph node-negative and estrogen-receptor positive.2 While there is a well-established role for adjuvant chemotherapy for tumors that are lymph node-positive, or with unfavorable histopathologic features,3, 4 there is limited data on the use of adjuvant chemotherapy in ER-positive, lymph node-negative breast cancers. Fifteen percent of patients treated with tamoxifen alone will recur over a 10-year period; thus, it is estimated that 85% would be overtreated if chemotherapy was given to each patient in this group.5
Treatment decisions in breast cancer traditionally have been made based on combinations of clinical and histopathologic risk factors, which include patient age, tumor size, histologic grade, estrogen and progesterone receptor status, ERBB2 (HER-2/neu) status, and lymph node status. However, histologic grade is considered by some to be subjective6, 7, 8, 9, 10, 11, 12 and as a whole these pathologic parameters are considered insufficient to stratify patients toward or away from adjuvant chemotherapy.5 Oncotype DX™ (Genomic Health, Redwood City, CA, USA) is a commercial assay that is becoming more popular and has been shown to predict tumor recurrence in lymph node-negative ER-positive breast cancers.
Oncotype DX™ is a reverse transcriptase polymerase chain reaction assay (RT-PCR) that analyzes the expression of 21 genes to give a distant disease Recurrence Score (RS). These are categorized as the Estrogen group (ER, PGR, BCL2, SCUBE2), HER2 group (GRB7, HER2), Proliferation group (Ki67, STK15, Survivin, CCNB1, MYBL2), Invasion group (MMP11, CTSL2), Others (GSTM1, CD68, BAG1) and Reference group. Yet, ER, PR, and HER2 genes are already analyzed by either protein expression or gene amplification, and pathologists already analyze the morphologic expression of the proliferation genes by the mitotic count. Thus, the assay includes molecular measures of several features that are already examined in a standard pathologic examination.
Although the Oncotype DX™ assay is a potentially useful tool for the stratification of breast cancer patients toward or away from chemotherapy, the assay costs over $3,000.13 Additionally, correlates of many of the genes it measures are already analyzed in a standard pathology examination. To date, there have been no studies by researchers independent of Genomic Health which examine the relationship between histopathologic variables and the Oncotype DX™ Recurrence Score. We therefore examined 42 cases of breast cancer from the files of Magee-Women's Hospital and analyzed the relation between the clinical/histopathologic variables (patient age, tumor size, tubule formation, nuclear grade, mitotic figures, ER immunohistochemical score, PR score, and HER-2/neu) and the Recurrence Score.
Materials and methods
Forty-two cases of breast carcinomas that had Oncotype DX™ performed were obtained from the pathology files of Magee-Women's Hospital of University of Pittsburgh Medical Center. All cases were ER-positive and node-negative except for 1 ER-negative case that had Oncotype Dx™ performed for unknown reasons. All H&E tumor slides and reports were reviewed. The tumors were graded according to the Elston and Ellis modification of the Nottingham grading system13, 14 using a Nikon eclipse 50i scope with a 0.55 mm high power field (HPF) diameter. The assignment of points for mitotic count was as follows: 1 point (0–8 mitotic figures/10 HPFs), 2 points (9–18 mitotic figures/10 HPFs) and 3 points (19 or more mitotic figures/10 HPFs).14
ER, PR, and HER-2/neu data was obtained from pathology reports. Immunohistochemistry for ER and PR was performed using the 6F11 and 1A6 antibodies, respectively, and IVIEW detection on the Benchmark XT (Ventana, Tucson, AZ, USA). At our institution, ER and PR results are reported using a semi-quantitative immunohistochemical score (previously described as ‘H-score’) which details the percentage of positive cells showing none, weak, moderate, or strong staining.15 The score is given as the sum of the percent staining multiplied by an ordinal value corresponding to the intensity level (0=none, 1=weak, 2=moderate, 3=strong). With four intensity levels, the resulting score ranges from 0 (no staining in the tumor) to 300 (diffuse intense staining of the tumor). HER-2/neu protein was analyzed and scored using CB11 antibody and basic DAB detection on Benchmark XT (Ventana). HER-2/neu was considered positive with either 3+ immunoreactivity or amplification by FISH (with a ratio of HER2 to chromosome 17 centromeric region >2.2, using PathVysion Vysis dual color FISH by Vysis Inc, Downers Grove, IL, USA).
Oncotype DX™ Recurrence Score was obtained from medical records. The RS classifies tumors into three risk categories: low (0–17) intermediate (18–30) and high (31–100).5 The RS was correlated with clinico-pathologic variables using the Pearson product-moment correlation coefficient (r) and coefficient of determination (r2) for continuous variables (patient age, tumor size, ER immunohistochemical score, PR immunohistochemical score) and the Spearman's rank order correlation coefficient (rs and rs2) for ordinal variables (tubule formation, nuclear grade, mitotic figures, and HER-2/neu status), with a two-tailed p-value of <0.05 considered significant. Multiple linear regression analysis was performed to model the prediction of the Oncotype DX™ RS by the same variables using a stepwise approach, with an entry probability of .05 and removal probability of 0.1. Models were also created to include Nottingham Grade or Nottingham Score rather than the individual components, and models were tested for interactions between variables. All data analyses were performed using SPSS version 11.5 (SPSS Inc., Chicago IL, USA).
This study was approved by the Institutional Review Board of University of Pittsburgh Medical Center.
Results
Median patient age was 58 years (range, 33–82). Median tumor size was 1.3 cm (range, 0.2–3.5). Fifteen cases were Nottingham Grade 1, 19 were Nottingham Grade 2, and eight were Nottingham Grade 3.
Table 1 shows the mean values or frequencies of each variable for low, medium, and high RS categories.
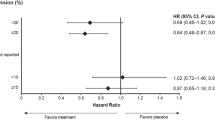
The correlation between Oncotype DX™ Recurrence Score (using the full range from 0–100) and other variables is detailed in Table 2. In a univariate model, tubule formation (1–3), nuclear grade (1–3), mitotic count (1–3), ER immunohistochemical score, PR immunohistochemical score, and HER-2/neu status (amplified vs non-amplified) are significantly correlated with the Oncotype DX™ Recurrence Score (Table 2). Similarly, both the Nottingham Score and Nottingham Grade, which are composite scores of the tubule formation, nuclear grade, and mitotic count, are significantly correlated with the Recurrence Score. Figures 1 and 2 show the correlation between the Recurrence Score and the Nottingham Grade and the ER immunohistochemical score, respectively.
In a multiple linear regression model, nuclear grade, mitotic count, ER immunohistochemical score, PR immunohistochemical score, and HER-2/neu status are significantly correlated with the Oncotype DX™ (Table 3). This model forms the regression equation: RS =13.424+5.420 (nuclear grade) +5.538 (mitotic count) −0.045 (ER immunohistochemical score) −0.030 (PR immunohistochemical score) +9.486 (HER-2/neu), with an R of 0.813 and R2 of 0.66, indicating that the full model accounts for 66% of the data variability. Patient age and tumor size were not significant predictors of Oncotype DX™ RS in either the univariate or multivariate models. Of all models created, which included using the full Nottingham Score or Grade instead of the components, this model had the highest R2. No potential interactions between any of the variables were significant.
Discussion
Currently, the decision to use adjuvant chemotherapy in breast cancer treatment is based primarily on the tumor size and lymph node status. Adjuvant chemotherapy has a well-established role tumors that are lymph node-positive, or tumors with unfavorable features such as lymphovascular space invasion, high nuclear or histologic grade, HER-2/neu overexpression and negativity for estrogen and progesterone receptors;3, 4 however, there is limited data on the use of adjuvant chemotherapy in ER-positive, lymph node-negative breast cancers. Based on the likelihood of distant recurrence in patients treated with tamoxifen alone, it is estimated that 85% of these patients would be overtreated if chemotherapy were given to each one.5 There are currently no consensus guidelines for the use of chemotherapy in this subgroup due to the lack of diagnostic assays that will predict high risk of recurrence.
Oncotype DX™ (Genomic Health Inc. Redwood City, CA, USA) is a commercial assay that has been shown to predict tumor recurrence in node-negative ER-positive breast cancers. It is an RT-PCR assay that analyzes the expression of 21 genes (16 cancer related and five control genes) to give a distant disease Recurrence Score ranging from 0–100. The RS score was created using training sets and a proprietary analytic method.5 The Oncotype DX™ RS was originally validated in 668 lymph node-negative, ER-positive breast cancer patients receiving tamoxifen in NSABP trial B-14, where a multivariate analysis of patient age, tumor size, tumor grade, HER-2 /neu status, hormone receptor status, and RS demonstrated that only tumor grade and Recurrence Score were significant predictors of distant recurrence, and the RS was also significantly correlated with the relapse-free interval and overall survival.5 The RS was subsequently validated as a predictive marker for response to chemotherapy and tamoxifen in 651 patients on NSABP B-20 and 645 patients on NSABP B-14.16
Conventional clinical and histopathologic factors for risk assessment in breast cancer include patient age, tumor size, histologic grade, estrogen and progesterone receptor status, HER-2/neu status, and lymph node status. These have been combined into numerous prognostic indicators, including the Nottingham Prognostic Index, St Gallen criteria, NIH consensus guidelines, and Adjuvant! Online. The Nottingham histologic grade is the most common grading system, and takes into account tubule formation, nuclear grade, and mitotic count, each scored from 1–3.14 Histologic grade is almost universally accepted by clinicians, included in consensus guidelines,4 and used in treatment decision making. The advantages of the Nottingham Grade (either as a composite score or decomposed into subsets of its three components) are that it is simple to determine, inexpensive, and has been shown repeatedly to have prognostic value in breast carcinoma.12, 17, 18, 19 However, histologic grade is considered by some to have poor reproducibility, particularly for nuclear pleomorphism and mitotic count.6, 7, 8, 9, 10, 11, 12 A standard pathology examination also includes analysis of estrogen and progesterone receptor status for the prediction of therapeutic response to hormone therapy, and HER-2/neu status by immunohistochemistry in conjunction with fluorescence in situ hybridization to assess potential response to Herceptin®.
Despite the complexity of the derivation of the Recurrence Score, the biologic basis for this scoring is intuitive. The six gene groups analyzed are categorized as the Estrogen group (ER, PGR, BCL2, SCUBE2), HER2 group (GRB7, HER2), Proliferation group (Ki67, STK15, Survivin, CCNB1, MYBL2), Invasion group (MMP11, CTSL2), Others (GSTM1, CD68, BAG1) and Reference group. Yet, estrogen and progesterone receptor and HER-2/neu genes are already analyzed by protein expression, or gene amplification (HER-2) in a standard surgical pathology examination. In addition, mitotic count, which is the morphologic expression of the proliferation genes, is one of the components of the Nottingham grading.
Given the correlation between clinico-pathologic variables and clinical outcomes, and given that the Oncotype DX™ RS has been shown to have predictive value in a subset of breast cancer patients, we hypothesized that histopathologic risk factors would be significant predictors of the Oncotype DX™ Recurrence Score. In our analysis of 42 breast cancer cases, the Nottingham Score and Grade (as well as their components: tubule formation nuclear grade, mitotic count), ER immunohistochemical score, PR immunohistochemical score, and HER-2/neu status are significantly correlated with the Oncotype DX™ RS. The Recurrence Score can be predicted with the regression equation RS=13.424+5.420 (nuclear grade) +5.538 (mitotic count) −0.045 (ER immunohistochemical score) −0.030 (PR immunohistochemical score)+9.486 (HER-2/neu). This full multivariate model accounts for 66% of the data variability. Thus, RS is fairly well predicted by a combination of nuclear grade, mitotic count, ER immunohistochemical score, PR immunohistochemical score, and HER-2/neu status, where the RS is directly proportional to the nuclear grade, mitotic count, and HER-2/neu status, and inversely proportional to the ER immunohistochemical score and PR immunohistochemical score.
Although we are describing a multivariate model of the Oncotype DX™ RS, it is instructive to examine the univariate relationship between the Nottingham Grade and the RS. Figure 1 and Table 4 show the distribution of cases by Nottingham Grade and Recurrence Score, and Table 5 details those cases which appear discordant, i.e. cases that are Nottingham Grade 1 but do not have a low risk RS, Nottingham Grade 2 cases but do not have a intermediate risk RS, and cases that are Nottingham grade 3 but do not have a high risk RS. Interestingly, the range of Recurrence Scores for Nottingham Grade 1 cases is 7–21, for Grade 2 is 4–47, and for Grade 3 is 30–86. Thus, for Grade 1 cases, the 5 that had an intermediate Recurrence Score rather than low were still in the lowest range of the intermediate category (score of 19–21). Additionally, for Grade 3 cases, the one that had an intermediate Recurrence Score rather than high was in the highest range of the intermediate category (score of 30). Grade 2 cases, on the other hand, have a wide range of Recurrence Scores that appear unpredictable. It is worth noting that there were no two-step discrepancies, that is, there were no cases that were Nottingham Grade 1 and high RS, and none that were Nottingham Grade 3 and low RS.
Clearly the holy grail of breast cancer research is to find prognostic markers that can reliably predict survival and response to therapies, thus allowing individualized therapy for each patient so all receive the maximal therapeutic benefit with minimal toxicity. Histopathologic markers have been criticized as being subjective and insufficient to fully stratify patients; yet, the molecular markers which have been developed are either still in research phases and/or very expensive.13 The most recent ASCO guidelines for use of tumor markers in breast cancer include, for the first time, a lengthy discussion of multiparameter gene expression analysis, including the Oncotype DX™ assay. They indicate that Oncotype DX™ ‘may’ be used to individualize breast cancer treatment and to predict those patients who would benefit most from adjuvant tamoxifen or chemotherapy.20
The most salient question is whether the additional information given by molecular testing independently of traditional histopathologic markers is enough to justify the expense. The few studies that have actually compared the traditional markers to newer molecular ones have found that they perform similarly. Eden et al22 showed that the conventional markers of the Nottingham Prognostic Index performed similarly to gene expression markers (by van’t veer21) for predicting metastasis-free survival. Similarly, in an analysis of breast cancer patients treated with cyclophosphamide, methotrexate, and 5-fluorouracil, Nimeus-Malmstrom et al23 found that gene expression data did not improve prediction of distant recurrence above and beyond the Nottingham Prognostic Index. Other researchers have also concluded that although molecular markers for breast cancer risk assessment, including Oncotype DX™, have strong potential, as of yet they have not been sufficiently validated for clinical practice.24 TAILORx is an ongoing prospective clinical trial specifically designed to evaluate the utility of Oncotype DX™ in clinical decision-making,25 and data from this will be available in the future. Finally, the studies published to date that demonstrate the cost effectiveness of Oncotype DX™ Recurrence Score-guided therapies have been sponsored by Genomic Health, the makers of the Oncotype DX™ assay,26, 27 and there has been no independent verification of this data.
Despite the substantial efforts towards clinical validation of Oncotype DX™, there are still several questions that remain unanswered. For instance, how reproducible is the RS? Is it affected by features such as an inflammatory response adjacent to the tumor, or tumor cellularity? Is it affected by differences in tissue fixation techniques, such as might be found at different hospitals? Cronin et al28 addressed the issue of reproducibility by performing the Oncotype DX™ assay on five levels in each of three tissue blocks taken from different sections of tumors. They found strong correlation in the expression of the 16 genes both between blocks as well as between tumor samples from the same block; however, this study included only two patients, and is the only published study addressing this issue. Regarding the possible effect of inflammation on the RS, one report suggests that in some cases a high Recurrence Score may be more related to peritumoral inflammatory response rather than the tumor itself.29 As the RS measures a group of proliferative genes, it is not surprising that a highly proliferative inflammatory response would elevate the RS. Given that Oncotype DX™ testing may be performed on excised tissue, which has inflammation as a component of prior biopsy site changes, this artifact may be more common than currently reported, and would certainly be of concern. To our knowledge there are no studies that assess the effect of tumor cellularity on RS. Finally, there appears to be no published data regarding the effect on RS of differences in tissue fixation techniques.
Because Oncotype DX™ is very expensive, has several unanswered questions related to its clinical practicability, and has not been shown conclusively to add valuable information independently of clinical and histopathologic markers, we suggest that rather than using the Oncotype DX™ assay indiscriminately in every case of lymph node-negative ER-positive breast cancer, it should be reserved for cases where it is difficult to make a clinical decision based on histopathology and receptor studies. The challenge remains defining the best algorithm for its use. Based on the relationship between Nottingham Grade and the Recurrence Score (Figure 1 and Table 4), it appears that it is unnecessary to perform Oncotype DX™ testing on cases that are Nottingham Grade 1 or 3, as the Recurrence Score in these cases for the most part correlates with the Nottingham Grade. However, the fact remains that at this point, even the cutoffs for the Recurrence Score are not entirely defined; in fact, in the TAILORx trial the Recurrence Score ranges are different from previously defined (low: <11, intermediate: 11–25, and high: >25).24, 25
In addition to defining a judicious algorithm for the use of Oncotype DX™, efforts must be focused on developing and/or refining simple and inexpensive risk factor assessments. For ER and PR, reporting intensity and percentage of cells positive for a particular stain (or using a semi-quantitative scoring method as described above) is more useful than a mere positive or negative report. Counting of mitotic figures must be standardized, and nuclear pleomorphism should be graded uniformly.
In conclusion, we present the correlation between histopathologic variables and the Oncotype DX™ Recurrence Score, as well as a multivariate model that predicts the RS. We are not suggesting that this regression equation actually be used in clinical practice, as this study was performed on a small group of cases and would need extensive additional validation. We suggest, however, that rather than performing Oncotype DX™ on all lymph node negative ER-positive breast cancer cases, Oncotype DX™ testing should be reserved for Nottingham Grade 2 cases as well as equivocal cases where it is difficult to make a clinical decision based on histopathology and receptor studies.
References
Jemal A, Siegel R, Ward E, et al. Cancer statistics, 2007. CA Cancer J Clin 2007;57:43–66.
Dunnwald L, Rossing M, Li C . Hormone receptor status, tumor characteristics, and prognosis: a prospective cohort of breast cancer patients. Breast Cancer Res 2007;9:R6.
Carlson R, Hudis C, Reed E, et al. Breast cancer. NCCN Clinical Practice Guidelines in Oncology™ [Cited 2007 November 7]; V.2.2007. Available from:http://www.nccn.org/professionals/physician_gls/PDF/breast.pdf.
Eifel P, Axelson J, Costa J, et al. National Institutes of Health consensus development conference statement: adjuvant therapy for breast cancer, November 1–3, 2000 J Natl Cancer Inst 2001;93:979–989.
Paik S, Shak S, Tang G, et al. A multigene assay to predict recurrence of tamoxifen-treated, node-negative breast cancer. N Engl J Med 2004;351:2817–2826.
Theissig F, Kunze K, Haroske G, et al. Histological grading of breast cancer. Interobserver, reproducibility and prognostic significance. Pathol Res Pract 1990;186:732–736.
Dalton L, Page D, Dupont W . Histologic grading of breast carcinoma. A reproducibility study. Cancer 1994;73:2765–2770.
Robbins P, Pinder S, de Klerk N, et al. Histological grading of breast carcinomas: A study of interobserver agreement. Hum Pathol 1995;26:873–879.
Frierson H, Wolber R, Berean K, et al. Interobserver reproducibility of the Nottingham modification of the Bloom and Richardson histologic grading scheme for infiltrating ductal carcinoma. Am J Clin Pathol 1995;103:195–198.
Kronqvist P, Montironi R, Kuopio T, et al. Subjective breast cancer grading. Analyses of reproducibility after application of Bayesian belief networks. Anal Quant Cytol Histol 1997;19:423–429.
Boiesen P, Bendahl P-O, Anagnostaki L, et al. Histologic grading in breast cancer: reproducibility between seven pathologic departments. Acta Oncol 2000;39:41–45.
Latinovic L, Heinze G, Birner P, et al. Prognostic relevance of three histological grading methods in breast cancer. Int J Oncol 2001;19:1271–1277.
Paik S . Molecular profiling of breast cancer. Curr Opin Obstet Gynecol 2006;18:59–63.
Elston CW, Ellis IO . Pathological prognostic factors in breast cancer. I. The value of histological grade in breast cancer: experience from a large study with long-term follow-up. Histopathology 1991;19:403–410.
McCarty Jr K, Miller L, Cox E, et al. Estrogen receptor analyses. Correlation of biochemical and immunohistochemical methods using monoclonal antireceptor antibodies. Arch Pathol Lab Med 1985;109:716–721.
Paik S, Tang G, Shak S, et al. Gene expression and benefit of chemotherapy in women with node-negative, estrogen receptor-positive breast cancer. J Clin Oncol 2006;24:3726–3734.
Genestie C, Zafrani B, Asselain B, et al. Comparison of the prognostic value of Scarff-Bloom-Richardson and Nottingham histological grades in a series of 825 cases of breast cancer: major importance of the mitotic count as a component of both grading systems. Anticancer Res 1998;18 (1B):571–576.
Frkovic-Grazio S, Bracko M . Long term prognostic value of Nottingham histological grade and its components in early (pT1N0M0) breast carcinoma. J Clin Pathol 2002;55:88–92.
Volpi A, Bacci F, Paradiso A, et al. Prognostic relevance of histological grade and its components in node-negative breast cancer patients. Mod Pathol 2004;17:1038–1044.
Harris L, Fritsche H, Mennel R, et al. American society of clinical oncology 2007 update of recommendations for the use of tumor markers in breast cancer. J Clin Oncol 2007;25:5287–5312.
van’t Veer LJ, Paik S, Hayes DF . Gene expression profiling of breast cancer: a new tumor marker. J Clin Oncol 2005;23:1631–1635.
Eden P, Ritz C, Rose C, et al. ‘Good Old’ clinical markers have similar power in breast cancer prognosis as microarray gene expression profilers. Eur J Cancer 2004;40:1837–1841.
Nimeus-Malmstrom E, Ritz C, Eden P, et al. Gene expression profilers and conventional clinical markers to predict distant recurrences for premenopausal breast cancer patients after adjuvant chemotherapy. Eur J Cancer 2006;42:2729–2737.
Ioannidis JPA . Is molecular profiling ready for use in clinical decision making? Oncologist 2007;12:301–311.
Sparano JA . The TAILORx trial: individualized options for treatment. Community Oncologist 2006;3:494–496.
Lyman GH, Cosler LE, Kuderer NM, et al. Impact of a 21-gene RT-PCR assay on treatment decisions in early-stage breast cancer. Cancer 2007;109:1011–1018.
Hornberger J, Cosler LE, Lyman GH . Economic analysis of targeting chemotherapy using a 21-gene RT-PCR assay in lymph-node-negative, estrogen-receptor-positive, early-stage breast cancer. Am J Manag Care 2005;11:313–324.
Cronin M, Watson D, Dutta D, et al. Reproducibility of quantitative gene expression analysis by a new RT-PCR assay using fixed paraffin-embedded tissues: a molecular tomographic scanning study [abstract no. 1491]. Mod Pathol 2004;17 (s1):353A.
Grimes M, Coad J, Oliviero B, et al. Comparison of oncotype-DX Recurrence Score and standard immunohistochemical prognostic markers [abstract no. 131]. Mod Pathol 2007;20 (2s):33A.
Author information
Authors and Affiliations
Corresponding author
Additional information
Presented in part at the International Academy of Pathology meeting in Montreal, QC, Canada; September 16–21, 2006.
Disclosure/conflict of interest
None of the authors have any conflict of interest with the materials presented in this paper.
Rights and permissions
About this article
Cite this article
Flanagan, M., Dabbs, D., Brufsky, A. et al. Histopathologic variables predict Oncotype DX™ Recurrence Score. Mod Pathol 21, 1255–1261 (2008). https://doi.org/10.1038/modpathol.2008.54
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/modpathol.2008.54
Keywords
This article is cited by
-
Platelets induce CD39 expression in tumor cells to facilitate tumor metastasis
British Journal of Cancer (2024)
-
Impact of reactive changes on multigene testing: histopathologic analysis of low-grade breast cancers with high-risk 21-gene recurrence scores
Breast Cancer Research and Treatment (2024)
-
A new methodology to predict the oncotype scores based on clinico-pathological data with similar tumor profiles
Breast Cancer Research and Treatment (2023)
-
Conventional and digital Ki67 evaluation and their correlation with molecular prognosis and morphological parameters in luminal breast cancer
Scientific Reports (2022)
-
Use of a supervised machine learning model to predict Oncotype DX risk category in node-positive patients older than 50 years of age
Breast Cancer Research and Treatment (2022)