Abstract
Intraepithelial tumor-infiltrating T cells have been correlated with improved outcomes in ovarian carcinoma, however, it is not known whether there is an association with disease stage, histological subtype, or BRCA mutation/expression. Two case series of ovarian carcinomas were included in the study; a retrospective series of 500 patients, and 40 prospectively collected cases fully characterized for BRCA1 mutation status and expression. Intraepithelial immune cells were assessed as present or absent by immunohistochemical staining of tissue microarrays. In the retrospective case series, the presence of intraepithelial CD8+ T-cells correlated with improved disease-specific survival (P=0.027), whereas intraepithelial CD3+ T cells did not (P=0.49). For serous ovarian carcinomas, the presence of intraepithelial CD3+ and CD8+ T-cells correlated with improved disease-specific survival (P=0.0016 and P≤0.0001, respectively). The presence of intraepithelial CD8+ T cells was not associated with improved survival in endometrioid or clear cell carcinomas. On multivariate analysis, disease stage and CD8+ T cells were found to be independently predictive of improved disease-specific survival, whereas grade, age at surgery, and type of adjuvant treatment were not. In the prospective patient cohort, intraepithelial CD8+ T-cells correlated with the presence of mutation or loss of expression of BRCA1 through promoter methylation (P=0.019). Intraepithelial CD8+ tumor-infiltrating T-cells correlate with improved clinical outcomes for all stages of ovarian cancer; this association is restricted to the serous ovarian cancer subtype, and is an independent prognostic factor on multivariate analysis. The presence of intraepithelial CD8+ T cells also significantly correlates with loss of BRCA1.
Similar content being viewed by others
Main
Ovarian cancer is the leading cause of mortality among gynecologic malignancies and the fifth leading cause of cancer death in women.1 Clinical prognostic factors include factors reflecting intrinsic tumor biology (stage and grade), patient factors (eg age, fitness to tolerate treatment), treatment factors (eg extent of surgical debulking), and the response to first line treatment.2 Despite high initial response rates to chemotherapy and the demonstrated improvements in median overall survival, fewer than 40% of patients with advanced disease survive to 5 years.3
Many potential molecular prognostic factors in ovarian cancer have been investigated (eg HER2, TP53).4 Most factors were identified in small studies and have not been reproduced or independently validated, precluding clinical utility. In addition, mutations of the BRCA1 and 2 tumor suppressor genes have been associated with improved clinical outcomes5, 6, 7 but the biologic mechanisms underlying these findings are not well understood to date.
The prognostic significance of the host immune response, as defined by the presence of tumor-infiltrating lymphocytes, has been studied in ovarian cancer8, 9, 10, 11 and other cancers12, 13, 14, 15, 16, 17, 18 Zhang et al10 identified intratumoral (later named intraepithelial) CD3+ T-cell infiltration to be an independent prognostic factor in 186 advanced ovarian cancers. Curiel et al8 demonstrated that infiltration of CD4+ CD25+ regulatory T-cells carried a worse prognosis in ovarian cancer. More recently, immunohistochemical evaluation of intraepithelial tumor-infiltrating lymphocytes in two cohorts of epithelial ovarian cancer of all cell types and stages showed that cases having a higher frequency of intraepithelial CD8+ tumor-infiltrating lymphocytes rather than CD3+ cells had improved survival compared to patients with lower frequencies.9, 11 Therefore, the immune response to ovarian cancer may serve as a novel prognostic marker. However, it remains unknown whether tumor histotype, stage or molecular pathogenesis affect the presence or the predictive value of intraepithelial tumor-infiltrating lymphocytes.
We used a large, population-based, clinically annotated, retrospective cohort of ovarian carcinomas treated according to standardized protocols from the province of British Columbia to assess for immune cell infiltrates using immunohistochemistry on tissue microarrays. The results were correlated with patient outcomes. In addition, we used an unselected, consecutive series of nonmucinous epithelial ovarian carcinomas that were extensively characterized for BRCA1 and BRCA2 mutation and expression status to determine whether T-cell infiltration is associated with BRCA status.19
Materials and methods
Patients
Most women diagnosed with ovarian cancer in British Columbia are referred to a British Columbia Cancer Agency-affiliated cancer treatment center, and provincial therapy guidelines are widely followed. We included all 832 epithelial ovarian cancer cases seen in the province of British Columbia from 1984 to 2000 that were stage I, grades 2 and 3, or stages II–III, any grade, and surgically cytoreduced to microscopic residual. All cases with residual macroscopic disease following surgery were excluded from this analysis. Histopathological features of this case series have been described in detail previously.20 Blocks for tissue microarray construction were available for 500 cases and these cases constitute the retrospective case series. Tumor grade was assigned according to the Silverberg grading system,21 but all clear cell carcinomas were considered to be high grade (grade 3). All mucinous carcinomas were of intestinal type; there were no mucinous carcinomas of endocervical type.
A second cohort consisted of 49 consecutive patients with stages I–III nonmucinous epithelial ovarian carcinoma recruited into a prospective study examining BRCA1 expression and mutation status at Vancouver General Hospital, as recently reported.19 A third cohort consisted of 29 cases of ovarian surface epithelial carcinoma where the number of intraepithelial CD8+ tumor-infiltrating lymphocytes was compared in whole sections vs tissue microarrays, constructed as described below. Approval for the study was obtained from the research ethics committee of the University of British Columbia.
Tissue Microarrays
Following pathology review, a representative area of each tumor was selected and duplicate 0.6 mm core tissue microarrays were constructed, as described previously.22
Immune Marker Analysis
Tissue microarrays were subjected to immunohistochemical analysis using antibodies against human CD3 (polyclonal, 1:300; Cell Marque), CD4 (clone 4B12, 1:50; Novocastra), CD8 (clone C8/144B, 1:50; Dako), CD20 (clone L26, 1:250; Dako), CD43 (clone MT1, 1:100; Vector), CD117 (polyclonal, 1:200; Dako), and granzyme-B (clone GrB-7, 1:25; Dako). Each 0.6 mm core was examined at × 20 magnification and scored simultaneously by two pathologists, who reached a score by consensus. Intraepithelial cells were defined strictly as being those within the epithelial component of the tumor (tumor islets), and were reported as being either present (ie one or more intraepithelial lymphocytes present in the two 0.6 mm cores for a given case) or absent. In the case of mast cells (CD117), the presence of any mast cells, whether stromal or epithelial, was recorded as a positive result. Data on immunostaining are not available for all 500 cases for all markers, primarily because of cores not containing tumor or not adhering to slides during processing. A second tissue microarray comprising the prospective case series was stained for CD8 exactly as above.
Unstained sections from the 500-case retrospective series described above were also transferred to a second laboratory, where they were interpreted independently, as described previously.10 Briefly, tissue sections were stained using polyclonal rabbit antihuman CD3 (Dako) and intraepithelial CD3+ tumor-infiltrating lymphocytes were classified as either present or absent.
In a cohort of 29 cases, whole sections were stained for CD8 and intraepithelial CD8+ cells were counted in 10 consecutive high power fields. This was carried out in five sets of 10 high power fields (total of 50 high power fields), and the results expressed as the average count per 10 high power fields for these five sets, to allow comparison with the results of assessment of intraepithelial CD8+ T cells in tissue microarray cores from the same blocks.
BRCA Analyses
The prospective cohort cases were previously characterized for BRCA1 and BRCA2 mutation status (germline and somatic), BRCA1 promoter hypermethylation, and BRCA1 mRNA and protein expression, as described elsewhere.19 Results for all assays were available for 47 cases and based on these results the tumors were divided into five groups: (1) tumors with a BRCA1 mutation (n=9); (2) tumors with epigenetic loss of BRCA1 expression (no BRCA1 or BRCA2 mutation, methylation of the BRCA1 promoter, absence of immunostaining for BRCA1 in the tumor cells, and decreased BRCA1 mRNA expression; n=9); (3) tumors with no abnormalities of BRCA1 or BRCA2 (n=22); (4) tumors equivocal for BRCA1 epigenetic loss (no mutations or methylation of the BRCA1 promoter, but decreased BRCA1 mRNA, protein, or both; n=4); and (5) tumors with a BRCA2 mutation (n=3). The cases with BRCA2 mutation or equivocal for BRCA1 loss (n=7) were excluded from further analysis as there were too few cases in these two groups, leaving a cohort of 40 cases for analysis of intratumoral T-cell infiltrates.
Gene Expression Analysis
In 34 cases of high-grade serous carcinoma from the Vancouver General Hospital prospective case series of 49 cases, tumor tissue was snap frozen at the time of primary surgery and gene expression profiling was performed. Only high-grade serous carcinomas were studied by gene expression profiling based on data presented herein showing that intraepithelial tumor-infiltrating lymphocytes are of prognostic significance primarily in this subtype of ovarian cancer. The Human Exonic Evidence-Based Oligonucleotide (HEEBO; Stanford) microarrays used in the study contained 44 544 70mer probes that were designed using a transcriptome-based annotation of exonic structure for genomic loci (http://www.microarray.org/sfgf/). After confirmation of the presence of viable tumor by frozen section, the tissue fragment was homogenized in Trizol reagent (Invitrogen, Carlsbad, CA, USA) and total RNA was extracted. Microarray hybridization and washing was performed using standard procedures.23, 24 Only spots with a ratio of signal over background of at least 1.3 in the Cy5 and 1.5 in the Cy5 channel were included. For data analysis, a set of standard filtering criteria was employed using only genes with 80% available good data that showed a minimum of fourfold variation from the mean expression level across all samples in at least three samples.
Statistical and Biocomputational Analyses
Statistical analyses of immune markers were performed with JMP v6.0.3 (SAS Institute, Carey, NC, USA) software. Univariable survival analysis was computed using the Kaplan–Meier method and statistical differences were determined using the log-rank test. Multivariable disease-specific survival analysis was carried out using the proportional hazards model. Immunohistochemical marker associations with histopathologic subtype and BRCA status were compared with the Pearson χ2-statistic. Multivariate correlations between various immunohistochemical markers were computed with the Kendall τb-statistic. P-values <0.05 were regarded as significant for all analyses. For comparison of interlaboratory assessment of intraepithelial T cells, κ-statistics were calculated.
For the gene expression study, unsupervised hierarchical clustering analysis was used to produce dendrograms that depict the degree of relatedness between tumor specimens based on their gene expression profiles.25 Significance analysis of microarrays26 was performed to identify differentially expressed genes between groups of tumor specimens. A false discovery rate of less than 0.05 was considered significant. Gene Ontology Term Finder analysis was performed using the online program from Stanford Microarray Database (http://smd.stanford.edu/cgi-bin/ontology/showTermFinder.pl) to identify enrichment of genes related to specific biological processes in each gene subcluster and a corrected P-value of <0.05 was considered significant.
Results
Patient Characteristics for the Retrospective Case Series
The median age at diagnosis was 58.1 years (range: 25.4–89.0 years). Patient characteristics are summarized in Supplementary Table 1. Of the 500 patients, 205 (41.0%) had stage I disease, 211 (42.2%) had stage II disease, and 84 (16.8%) had stage III disease. Of the four major tumor cell types, 212 cases were serous, 132 clear cell, 125 endometrioid, and 31 were mucinous carcinoma. When the cohort was divided into early (stages I and II) and late stage (stage III) cases, there were 143 serous cancers, 124 clear cell carcinomas, 119 endometrioid carcinomas, and 30 mucinous carcinomas in the early stage group, and 69 serous carcinomas, 8 clear cell, 6 endometrioid, and 1 mucinous in the advanced stage group. The median duration of follow-up was 5.3 years (range 0.1–18.0 years).
Prevalence of Immune Cell Infiltrates
Intraepithelial T cells
Intraepithelial CD3+, CD8+, and CD4+ T cells were detected in 60.4, 57.0, and 26.6% of cases, respectively (Supplementary Table 2). The frequency of CD8+ T-cell infiltration according to stage, grade, and histology is summarized in Table 1. Of note, CD8+ T cells were more commonly present in serous carcinomas, compared to either endometrioid or clear cell carcinomas (P=0.0016 and P<0.001, respectively).
Other intraepithelial immune/inflammatory cells
The frequency of the presence of other immune cells in the retrospective case series is shown in Supplementary Table 2. Correlations between the presence of the different immune cells within these cases are presented in Table 2, with the Kendall τ-statistic presented for each pairwise comparison; significant correlations are indicated in bold (P<0.05). This analysis shows that there are significant positive correlations between expression of all markers of immune cell infiltrates in ovarian carcinoma studied, with the exception of mast cells (CD117); the presence of CD117+ mast cells does not significantly correlate with the presence of any of the other cells.
Intraepithelial T Cells and Correlation with Patient Outcome
The presence of intraepithelial CD8+ tumor-infiltrating lymphocytes correlated with clinical outcomes when the cohort of 500 cases was analyzed. None of the other markers correlated with survival in the entire retrospective dataset. Intraepithelial CD8+ tumor-infiltrating lymphocytes correlated with improved disease-specific survival (disease-specific survival; P=0.027; Figure 1a) but not with progression-free survival (P=0.13) or overall survival (P=0.34) in the entire cohort.
Kaplan–Meier analysis of intraepithelial CD8+ T cells and disease-specific survival in the entire retrospective study cohort (a); in stage III cases (b); in stages I and II cases (c); and in serous carcinomas (d). For each graph the blue line (‘0’ in the figure legend) indicates those cases without intraepithelial CD8+ T cells and the red line (‘1’ in the figure legend) indicates those cases with intraepithelial CD8+ T cells.
Univariate analysis according to stage and cell type demonstrated that the presence of intraepithelial CD8+ tumor-infiltrating lymphocytes was significantly correlated with improved disease-specific survival (P=0.012), PFS (P=0.027) and OS (P=0.010) for stage III cancers, most of which (69/84, 82%) were of serous type (Figure 1b). Presence of intraepithelial CD8+ tumor-infiltrating lymphocytes approached significance as a correlate of disease-specific survival in early stage (stages I and II) cancers (P=0.052; Figure 1c). Analysis based on primary cell type showed that CD8+ tumor-infiltrating lymphocytes correlated with improved disease-specific survival in serous (P=0.0001; Figure 1d) and mucinous (P=0.01, data not shown) cancers, but not in endometrioid (P=0.79) or clear cell (P=0.6) cancers.
The presence of intraepithelial CD3+ tumor-infiltrating lymphocytes did not correlate with outcome when the entire cohort was examined by Kaplan–Meier survival analyses (P=0.49; Figure 2a). However, intraepithelial CD3+ tumor-infiltrating lymphocytes correlated with improved progression-free survival (P=0.01) and disease-specific survival (P=0.0087) in the subset of advanced stage (stage III) ovarian cancers (Figure 2b); as noted previously, the stage III cancers in this series consisted of a disproportionately high number of serous carcinomas. Intraepithelial CD3+ TILs were also significantly correlated with improved disease-specific survival in serous carcinomas of any stage (P=0.005, data not shown). A significant relationship between the presence of intraepithelial CD3+ TILs and disease-specific survival was not observed with the other histological cell types (clear cell (P=0.32); endometrioid (P=0.62); mucinous (P=0.51)).
Kaplan–Meier disease-specific survival analysis of intraepithelial CD3+ T cells in all cases (a); and in stage III cases (b). For each graph the blue line (‘0’ in the figure legend) indicates those cases without intraepithelial CD3+ T cells and the red line (‘1’ in the figure legend) indicates those cases with intraepithelial CD3+ T cells.
No correlation was identified between clinical outcome and the presence of immune/inflammatory cells identified by CD4, CD20, CD43, CD117, or granzyme-B immunostaining (data not shown).
On multivariate analysis, stage (P<0.0001), tumor cell type (P=0.048), and intraepithelial CD8+ TILs (P=0.0074) were found to be significantly correlated with disease-specific survival whereas the remaining variables tested (cell type, grade, age, intraepithelial CD3+ tumor-infiltrating lymphocytes, and treatment protocol) were not (Table 3).
Independent Assessment of CD3+ T Cells
Intraepithelial CD3+ TILs were prognostically significant for disease-specific survival in the subset of serous ovarian cancers, in univariate analysis, when staining and interpretation were performed in an independent laboratory (P=0.046 for the second laboratory, compared to P=0.013 in the original laboratory). The interlaboratory agreement in identification of intraepithelial CD3+ tumor-infiltrating lymphocytes was high (κ=0.71±0.03).
Intraepithelial T-Cell Infiltration and BRCA Status in the Prospective Series
A second cohort of patients, identified prospectively, underwent detailed analysis to assess BRCA1 and BRCA2 mutation status and BRCA1 promoter hypermethylation and expression (both RNA and protein). Eighteen cases (all high-grade serous carcinomas) showed either BRCA1 mutation (n=9), or epigenetic loss of BRCA1 (BRCA1 promoter hypermethylation with transcriptional silencing; n=9). Twenty-two cases, including all of the nonhigh-grade serous carcinomas (five endometrioid carcinomas, four clear cell carcinomas, and two grade 1 serous carcinomas), showed no BRCA1 or BRCA2 mutation, unmethylated BRCA1 promoter and normal BRCA1 mRNA and protein expression. Seventeen of 18 cases with BRCA1 mutation or loss of BRCA1 expression through epigenetic silencing had intraepithelial CD8+ tumor-infiltrating lymphocytes, compared to 11 of 19 cases without BRCA1 abnormalities (P=0.019). Considering only the high-grade serous carcinomas in this series, the association between the presence of CD8+ T cells and loss of BRCA1 was of borderline significance (P=0.05, single sided); this analysis should be repeated in a larger, independent case series.
Gene Expression Profile Analysis
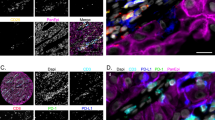
Unsupervised hierarchical clustering of 34 high-grade serous ovarian carcinomas from the prospective series separated the tumors into two main groups, designated groups A and B (Figure 3) and the genes were separated into five clusters (designated gene clusters 1–5). Carcinomas in group A showed relatively high level expression of genes in gene clusters 2 and 3. Gene Ontology Term Finder analysis showed that gene cluster 3 showed significant enrichment of genes involved in several biological processes that included immune response, antigen processing and presentation, and T-cell activation (Supplementary Table 3), including genes that were shown previously to be highly expressed in a subset of ovarian carcinomas.27 Comparison between the two groups of ovarian carcinomas identified by gene expression profiling revealed that all group A ovarian carcinomas (10 of 10) contained intraepithelial CD8+ tumor-infiltrating lymphocytes, unlike the carcinomas in group B (17 of 24 contained intraepithelial CD8+ tumor-infiltrating lymphocytes), with the difference being statistically significant (P<0.05). Thus, the tumors characterized by higher level expression of a range of immune response related genes are consistently positive for CD8+ T cells.
Hierarchical clustering of 34 high-grade serous carcinomas. Unsupervised hierarchical clustering based on 4192 filtered genes separates the carcinomas into two main groups, indicated as groups A and B on the dendrogram. The accompanying heatmap shows the expression profiles across the 4192 filtered genes, which cluster into five main groups (gene clusters 1–5) on hierarchical clustering analysis. The heatmap is a visual representation of the data with the x axis corresponding to the tumor specimens and the y axis corresponding to the genes. The level of gene expression in a tumor specimen for a specific gene relative to the mean expression level for that gene across all samples is shown colorimetrically from bright green (lowest gene expression) to bright red (highest gene expression). Gray color indicates missing data point (spot that did not fulfill the filtering criteria).
SAM analysis was subsequently performed to identify genes that are differentially expressed between carcinomas that are positive and negative for intraepithelial CD8+ tumor-infiltrating lymphocytes. The results of the significance analysis of microarrays are shown in Supplementary Table 4 (false discovery rate <0.05). Gene Ontology Term Finder analysis of the significantly upregulated genes identified in the CD8+ carcinomas by significance analysis of microarrays revealed a significant enrichment of genes involved in immune response (corrected P-value <0.05), which are listed in Table 4.
Discussion
Beyond the most basic clinical predictors of outcome (stage, debulking status, etc), ovarian cancers, and in particular high-grade serous ovarian cancers (the most commonly diagnosed histological subtype of ovarian cancer) have not been further subdivisible into prognostic categories. In this study, the use of a large, independent, population-based cohort of ovarian cancer cases debulked to microscopic residual disease provides definitive results on the prognostic significance of immune infiltration in a population of patients with intermediate-risk ovarian cancer, and defines novel associations of T-cell infiltration with ovarian cancer histologic subtype. Furthermore, we describe for the first time the association between the presence of T-cell infiltration and BRCA loss, suggesting a possible link to molecular mechanisms of genetic instability.
Prior work has demonstrated that high-grade serous tumors are frequently associated with BRCA mutation or epigenetic loss.19 We observed a significant association between intraepithelial tumor-infiltrating lymphocytes and BRCA mutation or epigenetic loss. Therefore, we have established a novel association between intraepithelial T cells, serous ovarian cancer histology, and BRCA mutation status. Similar observations have been made in medullary and atypical medullary breast carcinomas, which are also associated with BRCA1 mutation and are characterized by a dense lymphocytic infiltrate;28, 29 these breast cancers are noted for their relatively favorable prognosis despite being high grade, with numerous mitoses. Similarly, colorectal cancers with microsatellite instability are characterized by tumor-infiltrating lymphocytes and also carry a relatively favorable prognosis in spite of being higher grade.30 Whether the presence of immune infiltration is itself the mechanism responsible for the improvement in prognosis or it simply represents an epiphenomenon of other molecular processes linked with better clinical outcomes remains unknown.
We demonstrate that all immune cells covary with one another, possibly clarifying why multiple T-cell markers have been associated with clinical outcomes in ovarian cancer in previous studies.16, 17, 18 Like Zhang et al,10 we demonstrate (in two separate laboratories using independent testing and analysis) that intraepithelial CD3+ tumor-infiltrating lymphocytes correlate with disease-specific survival in serous ovarian carcinomas. Likewise, we have confirmed the results of two recent studies9, 11 by demonstrating that intraepithelial CD8+ tumor-infiltrating lymphocytes correlate with disease-specific survival in the entire study cohort (including all stages and histologies), as well as in the subset of serous ovarian carcinomas. We have demonstrated that the best marker of immune infiltration (from the panel of immune markers chosen for this study) is CD8, as it is the only marker to significantly predict outcome on multivariate analysis.
Our observation that CD8 is superior to CD3 as a marker of immune cell infiltrates highlights the fact that we do not yet know what the best marker of a prognostically significant immune response in ovarian cancer will prove to be. Unsupervised hierarchical clustering analysis separated 34 cases of high-grade serous carcinoma into two groups (A and B), one of which was characterized by expression of a set of genes involved in immune response, antigen processing and presentation, and T-cell activation. It is likely that a marker or combination of markers superior to CD8 will be discovered, particularly when the mechanism underlying the correlation between immune response and patient outcome is better understood.
In conclusion, we have validated that the presence of intraepithelial CD8+ T-cells correlates with improved clinical outcomes in a large cohort of ovarian cancer patients. This association is particularly linked to the serous histology, and this is an important molecular subdivision of this histological subtype. We also observed that intraepithelial tumor-infiltrating lymphocytes were associated with BRCA mutation or epigenetic loss, suggesting a possible link to chromosomal instability within tumors. Further studies are needed to understand the underlying molecular pathways responsible for this association between intraepithelial tumor-infiltrating lymphocytes and favorable prognosis.
References
Jemal A, Siegel R, Ward E, et al. Cancer statistics, 2006. CA Cancer J Clin 2006;56:106–130.
Agarwal R, Kaye SB . Prognostic factors in ovarian cancer: how close are we to a complete picture? Ann Oncol 2005;16:4–6.
Ozols RF . Systemic therapy for ovarian cancer: current status and new treatments. Semin Oncol 2006;33:S3–S11.
Crijns AP, Boezen HM, Schouten JP, et al. Prognostic factors in ovarian cancer: current evidence and future prospects. The ECCO 12 Educational Book of Eur J Cancer 2003;127–145.
Ben David Y, Chetrit A, Hirsh-Yechezkel G, et al. Effect of BRCA mutations on the length of survival in epithelial ovarian tumors. J Clin Oncol 2002;20:463–466.
Boyd J, Sonoda Y, Federici MG, et al. Clinicopathologic features of BRCA-linked and sporadic ovarian cancer. JAMA 2000;283:2260–2265.
Chiba T, Ohtani H, Mizoi T, et al. Intraepithelial CD8+ T-cell-count becomes a prognostic factor after a longer follow-up period in human colorectal carcinoma: possible association with suppression of micrometastasis. Br J Cancer 2004;91:1711–1717.
Curiel TJ, Coukos G, Zou L, et al. Specific recruitment of regulatory T cells in ovarian carcinoma fosters immune privilege and predicts reduced survival. Nat Med 2004;10:942–949.
Sato E, Olson SH, Ahn J, et al. Intraepithelial CD8+ tumor-infiltrating lymphocytes and a high CD8+/regulatory T cell ratio are associated with favorable prognosis in ovarian cancer. Proc Natl Acad Sci USA 2005;102:18538–18543.
Zhang L, Conejo-Garcia JR, Katsaros D, et al. Intratumoral T cells, recurrence, and survival in epithelial ovarian cancer. N Engl J Med 2003;348:203–213.
Hamanishi J, Mandai M, Iwasaki M, et al. Programmed cell death 1 ligand 1 and tumor-infiltrating CD8+ T lymphocytes are prognostic factors of human ovarian cancer. Proc Natl Acad Sci USA 2007;104:3360–3365.
Clemente CG, Mihm Jr MC, Bufalino R, et al. Prognostic value of tumor infiltrating lymphocytes in the vertical growth phase of primary cutaneous melanoma. Cancer 1996;77:1303–1310.
Jass JR . Lymphocytic infiltration and survival in rectal cancer. J Clin Pathol 1986;39:585–589.
Naito Y, Saito K, Shiiba K, et al. CD8+ T cells infiltrated within cancer cell nests as a prognostic factor in human colorectal cancer. Cancer Res 1998;58:3491–3494.
Nakano O, Sato M, Naito Y, et al. Proliferative activity of intratumoral CD8(+) T-lymphocytes as a prognostic factor in human renal cell carcinoma: clinicopathologic demonstration of antitumor immunity. Cancer Res 2001;61:5132–5136.
Schumacher K, Haensch W, Roefzaad C, et al. Prognostic significance of activated CD8(+) T cell infiltrations within esophageal carcinomas. Cancer Res 2001;61:3932–3936.
Fukunaga A, Miyamoto M, Cho Y, et al. CD8+ tumor-infiltrating lymphocytes together with CD4+ tumor-infiltrating lymphocytes and dendritic cells improve the prognosis of patients with pancreatic adenocarcinoma. Pancreas 2004;28:e26–e31.
Galon J, Costes A, Sanchez-Cabo F, et al. Type, density, and location of immune cells within human colorectal tumors predict clinical outcome. Science 2006;313:1960–1964.
Press JZ, De Luca A, Boyd N, et al. Ovarian carcinomas with genetic and epigenetic BRCA1 loss have distinct molecular abnormalities. BMC Cancer 20008;8:17.
Silverberg SG . Histopathologic grading of ovarian carcinoma: a review and proposal. Int J Gynecol Pathol 2000;19:7–15.
Gilks CB, Ionescu D, Kalloger SE, et al. Tumor cell type can be reproducibly diagnosed and is of independent prognostic significance in patients with maximally debulked ovarian carcinoma. Hum Pathol 2008;39:1239–1251.
Makretsov NA, Huntsman DG, Nielsen TO, et al. Hierarchical clustering analysis of tissue microarray immunostaining data identifies prognostically significant groups of breast carcinoma. Clin Cancer Res 2004;10:6143–6151.
Perou CM, Jeffrey SS, van de Rijn M, et al. Distinctive gene expression patterns in human mammary epithelial cells and breast cancers. Proc Natl Acad Sci USA 1999;96:9212–9217.
Perou CM, Sorlie T, Eisen MB, et al. Molecular portraits of human breast tumours. Nature 2000;406:747–752.
Eisen MB, Spellman PT, Brown PO, et al. Cluster analysis and display of genome-wide expression patterns. Proc Natl Acad Sci USA 1998;95:14863–14868.
Tusher VG, Tibshirani R, Chu G . Significance analysis of microarrays applied to the ionizing radiation response. Proc Natl Acad Sci USA 2001;98:5116–5121.
Schaner ME, Ross DT, Ciaravino G, et al. Gene expression patterns in ovarian carcinomas. Mol Biol Cell 2003;14:4376–4386.
Lakhani SR . The pathology of familial breast cancer: morphological aspects. Breast Cancer Res 1999;1:31–35.
Kuroda H, Tamaru J, Sakamoto G, et al. Immunophenotype of lymphocytic infiltration in medullary carcinoma of the breast. Virchows Arch 2005;446:10–14.
Buckowitz A, Knaebel HP, Benner A, et al. Microsatellite instability in colorectal cancer is associated with local lymphocyte infiltration and low frequency of distant metastases. Br J Cancer 2005;92:1746–1753.
Acknowledgements
CBG was supported by the National Cancer Institute of Canada (no. 017051) and an unrestricted educational grant from Sanofi-Aventis. GC was supported by NIH P50-CA083638 Ovarian Cancer SPORE. Blaise Clarke was recipient of a fellowship from Eli Lilly. CBG, SK, and DH received support OvCaRe. Patient outcome data and support in data analysis was provided by the Cheryl Brown Ovarian Cancer Outcomes Unit of the British Columbia Cancer Agency.
Author information
Authors and Affiliations
Corresponding author
Additional information
Disclosure/conflict of interest
The authors have no potential conflicts to report.
Supplementary Information accompanies the paper on Modern Pathology website (http://www.nature.com/modpathol)
Supplementary information
Rights and permissions
About this article
Cite this article
Clarke, B., Tinker, A., Lee, CH. et al. Intraepithelial T cells and prognosis in ovarian carcinoma: novel associations with stage, tumor type, and BRCA1 loss. Mod Pathol 22, 393–402 (2009). https://doi.org/10.1038/modpathol.2008.191
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/modpathol.2008.191
Keywords
This article is cited by
-
Single-cell tumor-immune microenvironment of BRCA1/2 mutated high-grade serous ovarian cancer
Nature Communications (2022)
-
Prognostic immunologic signatures in epithelial ovarian cancer
Oncogene (2022)
-
Neoadjuvant chemotherapy alters the balance of effector to suppressor immune cells in advanced ovarian cancer
Cancer Immunology, Immunotherapy (2021)
-
Clinical characteristics and prognostic implications of BRCA-associated tumors in males: a pan-tumor survey
BMC Cancer (2020)
-
Differences in immune-related gene expressions and tumor-infiltrating lymphocytes according to chemotherapeutic response in ovarian high-grade serous carcinoma
Journal of Ovarian Research (2020)