Abstract
Objective:
The objective of this study is to analyze the association of diabetes mellitus with progress and outcomes of prostaglandin (PG) labor induction using a retrievable vaginal insert.
Study Design:
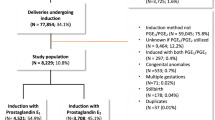
This is a secondary analysis of data collected during the Misoprostol Vaginal Insert Trial (Miso-Obs-004), a multicenter, double-blind, randomized controlled trial of women undergoing induction of labor with PGs. The duration, characteristics and outcomes of labor were compared in women with and without diabetes. Multivariable regression analysis was performed on all outcomes of interest, adjusting for differences in baseline characteristics.
Results:
There were 122 women with diabetes within the sample of 1275 women who delivered during their first admission. The time to reach active labor was significantly prolonged among women with diabetes compared with those without (22.0±13.0 vs 18.5±11.1, P=0.008) as was the time to delivery (30.2±15.0 vs 26.0±12.6, P=0.004). Fewer women with diabetes delivered within 36 h (adjusted odds ratio: 0.41, 95% confidence interval: 0.26 to 0.66, P=0.0003) and 48 h (adjusted odds ratio: 0.36, 95% confidence interval: 0.19 to 0.71, P=0.004). These relationships were significant after a multivariate regression analysis of baseline characteristics that adjusted for age, race, parity, body mass index, baseline modified Bishop Score, gestational age at induction and treatment group allocation.
Conclusion:
After PG labor induction, women with diabetes took longer to reach active labor and to deliver. We emphasize that this result comes from a secondary analysis and needs confirmation with additional studies.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout
Similar content being viewed by others
References
Reddy UM, Laughon SK, Sun L, Troendle J, Willinger M, Zhang J . Prepregnancy risk factors for antepartum stillbirth in the United States. Obstet Gynecol 2010; 116: 1119–1126.
Rosenstein MG, Cheng YW, Snowden JM, Nicholson JM, Doss AE, Caughey AB . The risk of stillbirth and infant death stratified by gestational age in women with gestational diabetes. Am J Obstet Gynecol 2012; 206 (4): 309.e1–7.
American College of Obsetrics & Gynecology. Pregestational Diabetes . Practice Bulletin 60. March 2005 (reaffirmed 2012).
American College of Obstetrics & Gynecology. Gestational Diabetes Mellitus. Practice Bulletin 137. August 2013.
Witkop CT, Neale D, Wilson LM, Bass EB, Nicholson WK . Active compared with expectant delivery management in women with gestational diabetes: a systematic review. Obstet Gynecol 2009; 113: 206–217.
Niu B, Lee VR, Cheng YW, Frias AE, Nicholson JM, Caughey AB . What is the optimal gestational age for women with gestational diabetes type A1 to deliver? Am J Obstet Gynecol 2014; 211 (4): 418.e1–418.e6.
Sutton AL, Mele L, Landon MB, Ramin SM, Varner MW, Thorp JM Jr et al. Delivery timing and cesarean delivery risk in women with mild gestational diabetes mellitus. Am J Obstet Gynecol 2014; 211: 244.e1–244.e7.
Berkley E, Meng C, Rayburn WF . Success rates with low dose misoprostol before induction of labor for nulliparas with severe preeclampsia at various gestational ages. J Matern Fetal Neonatal Med 2007; 20: 825–831.
Pevzner L, Rayburn WF, Rumney P, Wing DA . Factors predicting successful labor induction with dinoprostone and misoprostol vaginal inserts. Obstet Gynecol 2009; 114: 261–267.
Melamed N, Ben-Haroush A, Kremer S, Hod M, Yogev Y . Failure of cervical ripening with prostaglandin-E2 can it be predicted? J Matern Fetal Neonatal Med 2010; 23: 536–540.
Wing DA, Tran S, Paul RH . Factors affecting the likelihood of successful induction after intravaginal misoprostol application for cervical ripening and labor induction. Am J Obstet Gynecol 2002; 186: 1237–1240.
Mbele AM, Makin JD, Pattinson RC . Can the outcome of induction of labour with oral misoprostol be predicted. S Afr Med J 2007; 97: 289–292.
Tan TC, Yan SY, Chua TM, Biswas A, Chong YS . A randomised controlled trial of low-dose misoprostol and dinoprostone vaginal pessaries for cervical priming. BJOG 2010; 117: 1270–1277.
Williams MC, Krammer J, O'Brien WF . The value of the cervical score in predicting successful outcome of labor induction. Obstet Gynecol 1997; 90: 784–789.
Xenakis EM, Piper JM, Conway DL, Langer O . Induction of labor in the nineties: conquering the unfavorable cervix. Obstet Gynecol 1997; 90: 235–239.
Sak ME, Soydinc HE, Evsen MS, Sak S, Gul T . Which factors may influence the duration of misoprostol-induced abortion in the second trimester? Clin Exp Obstet Gynecol 2013; 40 (3): 356–358.
Timofeev J, Huang CC, Singh J, Driggers RW, Landy HJ . Spontaneous labor curves in women with pregnancies complicated by diabetes. J Matern Fetal Neonatal Med 2012; 25 (1): 20–26.
Wing DA . Misoprostol Vaginal Insert Consortium. Misoprostol vaginal insert compared with dinoprostone vaginal insert: a randomized control trial. Obstet Gynecol 2008; 112: 801–812.
WHO. Obesity: Preventing and Managing the Global Epidemic Report on a WHO Consultation on Obesity, Geneva, 3–5 June 1997.
ACOG Committee on Practice Bulletins — Obstetrics. ACOG Practice Bulletin No. 107: induction of labor. Obstet Gynecol 2009; 114: 386–397.
Al-Qahtani S, Heath A, Quenby S, Dawood F, Floyd R, Burdyga T, Wray S . Diabetes is associated with impairment of uterine contractility and high cesarean section rate. Diabetologia 2012; 55: 489–498.
Favaro RR, Salgado RM, Raspantini PR, Fortes ZB, Zorn TM . Effects of long-term diabetes on the structure and cell proliferation of the myometrium in the early pregnancy of mice. Int J Exp Pathol 2010; 91: 426–435.
Reece EA . Maternal fuels, diabetic embryopathy: pathomechanisms and prevention. Semin Reprod Endocrinol 1999; 17: 183–194.
Jawerbaum A, Gonzalez E . The role of alterations in arachidonic acid metabolism and nitric oxide homeostasis in rat models of diabetes during early pregnancy. Curr Pharm Des 2005; 11: 1327–1342.
Al-Matubsi HY, Salim MD, El-Sharaky AS, Kamel MA, Oriquat GA, Helmy MH et al. Activities of cyclooxygenases, and levels of prostaglandins E2 and F2alpha, in fetopathy associated with experimental diabetic gestation. Diabetes Metab 2010; 36: 43–50.
Vidaeff AC, Ramin SM . Potential biochemical events associated with initiation of labor. Curr Med Chem 2008; 15: 614–619.
Gabbe SG, Mestman JH, Freeman RK, Goebelsmann UT, Lowensohn RI, Nochimson D et al. Management and outcome of pregnancy in diabetes mellitus, classes B to R. Am J Obstet Gynecol 1977; 129: 723–732.
Sacks DA, Chen W, Greenspoon JS, Wolde-Tsadik G. Should the same glucose values be targeted for type 1 as for type 2 diabetes in pregnancy? Am J Obstet Gynecol 1997; 177: 1113–1119..
Blackwell SC, Hassan SS, Wolfe HW, Michaelson J, Berry SM, Sorokin Y . Why are cesarean delivery rates so high in diabetic pregnancies? J Perinat Med 2000; 28 (4): 316–320.
Author information
Authors and Affiliations
Ethics declarations
Competing interests
Dr Wing was the primary investigator for this multicenter consortium, which was funded Cytokine Pharmasciences (King of Prussia, PA). Cytokine Pharmasciences was purchased by Ferring Pharmaceuticals in 2012 and Dr Wing serves as a consultant for Ferring. Dr Powers was employed by Cytokine PharmaSciences and is a current consultant for Ferring. All other authors declare no conflicts of interest.
Rights and permissions
About this article
Cite this article
Hawkins, J., Stephenson, M., Powers, B. et al. Diabetes mellitus: an independent predictor of duration of prostaglandin labor induction. J Perinatol 37, 488–491 (2017). https://doi.org/10.1038/jp.2016.270
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/jp.2016.270