Abstract
Objective:
Compared with pressure-controlled ventilation (PCV), volume-targeted ventilation is associated with decreased neonatal complications, including the combined outcome of death or bronchopulmonary dysplasia. However, little is known about its effect on neurodevelopmental outcome. We evaluated the hypothesis that as compared with PCV, volume-targeted ventilation reduces the risk of the combined outcome of neurodevelopmental impairment or death in very low birth weight infants.
Study Design:
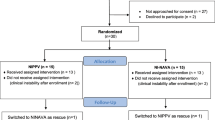
We studied a cohort of extremely preterm infants managed with either volume guarantee pressure support ventilation (VGPSV; n=135) or PCV (n=135). Infants were evaluated at 18 months adjusted age with a standardized neurological examination and the Bayley Scales of Infant and Toddler Development-third edition. Logistic regression models were used to evaluate the association of ventilation mode and neurodevelopmental outcome.
Result:
Rates of pulmonary interstitial emphysema (odds ratio 0.6; 95% confidence limits: 0.4, 0.8), hypotension (odds ratio: 0.7; 95% confidence limits: 0.5, 0.9) and mortality (odds ratio 0.45; 95% confidence limits: 0.22, 0.9) were lower among infants treated with VGPSV. The infants in the VGPSV group had a significantly shorter duration on mechanical ventilation compared with infants in the PCV group (log-rank test P<0.01). Seventy percent (155/221) of survivors were evaluated at 18 months adjusted age. A trend towards benefit for the combined outcome of death or neurodevelopmental impairment was seen in the VGPSV group but did not reach statistical significance (odds ratio: 0.59; 95% confidence limits: 0.32, 1.08).
Conclusion:
VGPSV was associated with a decreased risk of short-term complications but not long-term developmental impairment in this modest-sized cohort.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout


Similar content being viewed by others
References
Stoll BJ, Hansen NI, Bell EF, Shankaran S, Laptook AR, Walsh MC et al. Neonatal outcomes of extremely preterm infants from the NICHD Neonatal Research Network. Pediatrics 2010; 126 (3): 443–456.
Philip AG . Bronchopulmonary dysplasia: then and now. Neonatology 2012; 102 (1): 1–8.
Skidmore MD, Rivers A, Hack M . Increased risk of cerebral palsy among very low birth weight infants with chronic lung disease. Dev Med Child Neurol 1990; 32: 325.
Goldsmith & Karoktin Assisted Ventilation of the Neonate, 5th edn, Saunders Elsevier, St Louis, Missouri, 2011.
Jobe AH, Ikegami M . Mechanisms initiating lung injury in the preterm. Early Hum Dev 1998; 53 (1): 81–94.
Dreyfuss D, Saumon G . Ventilator-induced lung injury: lessons from experimental studies. Am J Respir Crit Care Med 1998; 157: 294–323.
Clark RH, Gerstmann DR, Jobe AH, Moffitt ST, Slutsky AS, Yoder BA . Lung injury in neonates: causes, strategies for prevention, and long-term consequences. J Pediatr 2001; 139: 478–486.
Dreyfuss D, Saumon G . Role of tidal volume, FRC, and end-inspiratory volume in the development of pulmonary edema following mechanical ventilation. Am Rev Resp Dis 1993; 148: 1194–1203.
Sinha S, Donn S . Minimizing ventilator induced lung injury in preterm infants. Arch Dis Child Fetal Neonatal Ed 2006; 91: F226–F230.
Wheeler KI, Klingenberg C, Morley CJ, Davis PG . Volume-targeted versus pressure-limited ventilation for preterm infants: a systematic review and meta-analysis. Neonatology 2011; 100 (3): 219–227.
Greisen G, Munck H, Lou H . May hypocarbia cause ischaemic brain damage in the preterm infant? Lancet 1986; 2 (8504): 460.
Erickson SJ, Grauaug A, Gurrin L, Swaminathan M . Hypocarbia in the ventilated preterm infant and its effect on intraventricular haemorrhage and bronchopulmonary dysplasia. J Paediatr Child Health 2002; 38: 560–562.
Giannakopoulou C, Korakaki E, Manoura A, Bikouvarakis S, Papageorgiou M, Gourgiotis D et al. Significance of hypocarbia in the development of periventricular leukomalacia in preterm infants. Pediatr Int 2004; 46: 268–273.
Keszler M, Abubakar K . Volume guarantee: stability of tidal volume and incidence of hypocarbia. Pediatr Pulmonol 2004; 38: 240–245.
Cheema IU, Sinha AK, Kempley ST, Ahluwalia JS . Impact of volume guarantee ventilation on arterial carbon dioxide tension in newborn infants: a randomized controlled trial. Early Hum Dev 2007; 83: 183–189.
Singh J, Sinha SK, Alsop E, Gupta S, Mishra A, Donn SM . Long term follow-up of very low birthweight infants from a neonatal volume versus pressure mechanical ventilation trial. Arch Dis Child Fetal Neonatal Ed 2009; 94: F360–F362.
D’Angio CT, Chess PR, Kovacs SJ, Sinkin RA, Phelps DL, Kendig JW et al. Pressure-regulated volume control ventilation vs synchronized intermittent mandatory ventilation for very low-birth-weight infants: a randomized controlled trial. Arch Pediatr Adolesc Med 2005; 159: 868–875.
Palisano R, Rosenbaum P, Walter S, Russell D, Wood E, Galuppi B . Development and reliability of a system to classify gross motor function in children with cerebral palsy. Dev Med Child Neurol 1997; 39: 214–223.
Vohr BR, Wright LL, Dusick AM, Mele L, Verter J, Steichen JJ et al. Neurodevelopmental and functional outcomes of extremely low birth weight infants in the National Institute of Child Health and Human Development Neonatal Research Network, 1993-1994. Pediatrics 2000; 105: 1216–1226.
Bayley N . Technical Manual of the Bayley Scales of Infant and Toddler Development, 3rd edn, Harcourt Assessment Inc: San Antonio, TX, USA, 2006.
Gordon PV, Swanson JR, Attridge JT, Clark R . Emerging trends in acquired neonatal intestinal disease: is it time to abandon Bell’s criteria? J Perinatol 2007; 11: 661–671.
Klein JO . Bacterial sepsis and meningitis. In: Remington JS, Klein JO (eds). Infectious Diseases of Fetus and Newborn Infant, 5th edn, Sauders: Philadelphia, PA, USA, 2001; 943–998.
Papile LA, Burstein J, Burstein R, Koffler H . Incidence and evolution of subependymal and intraventricular hemorrhage: a study of infants with birth weights less than 1,500 gm. J Pediatr 1978; 92: 529–534.
Committee for the Classification of Retinopathy of Prematurity. The international classification of retinopathy of prematurity revisited. Arch Ophthalmol 2005; 123: 991–999.
Engle WD . Definition of normal blood pressure range: the elusive target. In: Kleinman CS, Seri I (eds). Neonatology Questions and Controversies: Hemodynamics and Cardiology. Saunders/Elsevier Co: Philadelphia, PA, USA, 2008; 39–66.
Pryds O . Control of cerebral circulation in the high-risk neonate. Ann Neurol 1991; 30: 321–329.
Swamy R, Gupta S, Singh J, Donn SM, Sinha SK . Tidal volume delivery and peak inspiratory pressure in babies receiving volume targeted or time-cycled, pressure limited ventilation: a randomized controlled trial. J Neonatal Perinatal Med 2008; 4: 239–243.
Nafday SM, Green RS, Lin J, Brion LP, Ochshorn I, Holzman IR . Is there an advantage of using pressure support ventilation with volume guarantee in the initial management of premature infants with respiratory distress syndrome? A pilot study. J Perinatol 2005; 25: 193–197.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Additional information
Supplementary Information accompanies the paper on the Journal of Perinatology website
Supplementary information
Rights and permissions
About this article
Cite this article
Stefanescu, B., Frewan, N., Slaughter, J. et al. Volume guarantee pressure support ventilation in extremely preterm infants and neurodevelopmental outcome at 18 months. J Perinatol 35, 419–423 (2015). https://doi.org/10.1038/jp.2014.228
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/jp.2014.228
This article is cited by
-
Volume-targeted ventilation vs pressure-controlled ventilation for very low birthweight infants: a protocol of a randomized controlled trial
Trials (2023)
-
Volume guarantee pressure support ventilation in extremely preterm infants and neurodevelopmental outcome at 18 months
Journal of Perinatology (2015)