Abstract
Objective:
To investigate the effect of targeted neonatal echocardiography (TnEcho) on heart rate, arterial oxygen saturation (SPO2), cerebral regional oxygen saturation (CrSO2) and cerebral fractional oxygen extraction (CFOE) in extremely preterm infants during the first 3 postnatal days.
Study Design:
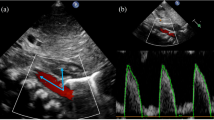
As a nested study in a prospective observational study, we acquired continuous data on heart rate, SPO2, CrSO2 and CFOE. Data averaged for the duration of TnEcho study were compared with the data collected during a baseline period immediately before the start of echocardiography. The duration of the baseline and study periods was the same. TnEcho evaluation included assessment of preload, afterload, contractility, left and right ventricular output, patent ductus arteriosus and foramen ovale.
Result:
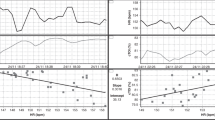
We analyzed 138 data pairs before and during TnEcho in 22 extremely preterm infants (gestational age 25.9±1.2 weeks; range 23 to 27). There was no significant difference in heart rate between baseline and TnEcho period. There was a statistical, but clinically negligible, difference between baseline and TnEcho in SPO2 (median (quartile) 91.4% (88.9, 94.2) vs 91.3% (88.9, 94), P=0.048), CrSO2 (76.8% (70.7, 81.5) vs 74.9% (69.5, 80.1), P<0.0001) and CFOE (15.8% (9.8, 23.6) vs 17.5% (11.3, 24.7), P<0.0001). The changes in the parameters monitored were similar in preterm infants who developed peri/intraventricular hemorrhage and in those who did not.
Conclusion:
Although there were statistically significant changes in SPO2, CrSO2 and CFOE, the alterations were minimal and unlikely of clinical relevance. Thus, cerebral hemodynamics and systemic and cerebral oxygenation are not perturbed during TnEcho and the procedure is well tolerated by the extremely preterm infants during the postnatal transitional period.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout

Similar content being viewed by others
References
De Boode W-P . Clinical monitoring of systemic hemodynamics in critically ill newborns. Early Hum Dev 2010; 86: 137–141.
Noori S, Stavroudis TA, Seri I . Principles of developmental cardiovascular physiology and pathophysiology. In: Hemodynamics and Cardiology Neonatology Questions and Controversies. 2nd edn. Saunders, Elsevier: Philadelphia, PA, USA, 2012.
Mertens L, Seri I, Marek J, Arlettaz R, Barker P, McNamara P et al. Targeted Neonatal Echocardiography in the Neonatal Intensive Care Unit: practice guidelines and recommendations for training. Writing Group of the American Society of Echocardiography (ASE) in collaboration with the European Association of Echocardiography (EAE) and the Association for European Pediatric Cardiologists (AEPC). J Am Soc Echocardiogr 2011; 24: 1057–1078.
El-Khuffash A, Herbozo C, Jain A, Lapointe A, McNamara PJ . Targeted neonatal echocardiography (TnECHO) service in a Canadian neonatal intensive care unit: a 4-year experience. J Perinatol 2013; 33: 687–690.
Perlman JM, McMenamin JB, Volpe JJ . Fluctuating cerebral blood-flow velocity in respiratory-distress syndrome. Relation to the development of intraventricular hemorrhage. N Engl J Med 1983; 309: 204–209.
Bada HS, Korones SB, Perry EH, Arheart KL, Ray JD, Pourcyrous M et al. Mean arterial blood pressure changes in premature infants and those at risk for intraventricular hemorrhage. J Pediatr 1990; 117: 607–614.
Groves AM, Kuschel CA, Knight DB, Skinner JR . Cardiorespiratory stability during echocardiography in preterm infants. Arch Dis Child 2005; 90: 86–87.
Limperopoulos C, Gauvreau KK, O’Leary H, Moore M, Bassan H, Eichenwald EC et al. Cerebral hemodynamic changes during intensive care of preterm infants. Pediatrics 2008; 122: e1006–e1013.
Van Alfen-van der Velden AAEM, Claessen VPJ, Hopman JCW, Klaessens JHGM, Sengers RCA, Liem KD . Changes in cerebral oxygenation and hemodynamics during cranial ultrasound in preterm infants. Brain Dev 2009; 31: 427–434.
Noori S, McCoy M, Anderson MP, Ramji F, Seri I . Changes in cardiac function and cerebral blood flow in relation to peri/intraventricular hemorrhage in extremely preterm infants. J Pediatr 2013; 164: 264–270.
Van Bel F, Lemmers P, Naulaers G . Monitoring neonatal regional cerebral oxygen saturation in clinical practice: value and pitfalls. Neonatology 2008; 94: 237–244.
Acknowledgements
Somanetics Corporation (now Covidien) provided the near-infrared spectroscopy monitors and sensors for the duration of the study.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Rights and permissions
About this article
Cite this article
Noori, S., Seri, I. Does targeted neonatal echocardiography affect hemodynamics and cerebral oxygenation in extremely preterm infants?. J Perinatol 34, 847–849 (2014). https://doi.org/10.1038/jp.2014.127
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/jp.2014.127
This article is cited by
-
Point-of-care ultrasound (POCUS) protocol for systematic assessment of the crashing neonate—expert consensus statement of the international crashing neonate working group
European Journal of Pediatrics (2022)
-
Implementing point of care ultrasound in the neonatal intensive care unit: a safety study
Journal of Perinatology (2021)
-
Introduction to neonatologist-performed echocardiography
Pediatric Research (2018)
-
Correlations between near-infrared spectroscopy, perfusion index, and cardiac outputs in extremely preterm infants in the first 72 h of life
European Journal of Pediatrics (2018)
-
Early treatment versus expectative management of patent ductus arteriosus in preterm infants: a multicentre, randomised, non-inferiority trial in Europe (BeNeDuctus trial)
BMC Pediatrics (2018)