Abstract
Retinoic acid receptor-related orphan receptor-α (RORα) plays a key role in the regulation of lipid and cholesterol metabolism that has been implicated in the development of chronic obstructive pulmonary disease (COPD). The aim of this study was to determine the frequencies of single-nucleotide polymorphisms (SNPs) in RORα gene in a Chinese population and their possible association with COPD susceptibility. Nine tagging SNPs, including rs17270181, rs1898413, rs17270216, rs8033552, rs8036966, rs7169364, rs340002, rs340023 and rs11630262, were screened in 279 COPD patients and 367 controls by the SNaPshot method. Association analysis of genotypes and haplotypes constructed from these loci with COPD was conducted under different genetic models. Alleles or genotypes of rs8033552 distributed significantly differently in COPD patients and controls (allele: P=0.0001, false discovery rate (FDR) Q=0.004, odds ratios (OR): 1.62 and 95% confidence interval (CI): 1.27–2.07; genotype: P=0.0005, FDR Q=0.008). The allele A at rs8033552 was potentially associated with an increased risk of COPD in additive model, displaying ORs of 1.62 (95% CI: 1.17–2.26, P=0.004, FDR Q=0.019) in subjects with genotypes AG vs GG and 2.69 (95% CI: 1.47–4.93, P=0.001, FDR Q=0.011) in subjects with genotypes AA vs GG, respectively. In haplotype analysis, we observed haplotypes GGAGATGTG and GGAGCTGTG had protective effects, whereas haplotypes GGAGATACA and GGAGATACG were significantly associated with the increased risk of COPD. These data suggest that RORα may be a potential risk gene for COPD.
Similar content being viewed by others
Introduction
Chronic obstructive pulmonary disease (COPD) is a major global disease that has been predicted to be the third leading cause of mortality worldwide by the year 2020,1 and it is estimated to affect nearly 8.2% of the Chinese adult population.2 Although cigarette smoke is a main risk factor for COPD, only ∼20% of smokers develop this pathology;3 thus, there are additional factors that are implicated in the pathogenesis of COPD. The variation in the susceptibility to cigarette smoke, in combination with the familial inheritance pattern of COPD, suggests that there may be a genetic component to the development of COPD.4, 5 The associations between COPD and polymorphisms in genes with potential importance in COPD pathogenesis have been investigated;6 however, only α1-antitrypsin has been unequivocally identified as relevant to the development of COPD. Recently, polymorphisms in the CHRNA3-CHRNA5-IREB2, HHIP and FAM13A loci have been found to influence susceptibility to COPD by genome-wide association studies,7, 8, 9, 10 but they explained little more than 3% of the variance in lung function.
There is increasing evidence of lipid/cholesterol metabolism in the pathophysiology of COPD,11, 12, 13, 14, 15 and the polymorphisms in genes for apolipoprotein M, a component of high-density lipoprotein, are associated with emphysema.12 Retinoic acid receptor-related orphan receptor-α (RORα) is a member of the nuclear hormone receptor superfamily.16 RORα is known to play a key role in the regulation of circadian rhythms and pathways including inflammation, lipid metabolism and cholesterol.17 Cholesterol and cholesterol derivatives have been identified as natural ligands of RORα.18 In addition to binding cholesterol, RORα has also been shown to regulate lipoproteins, such as high-density lipoprotein HDL, apolipoprotein A1 (the major constituent of high-density lipoprotein HDL), apolipoprotein A5 and apolipoprotein CIII.19, 20, 21 Further evidence for the role of RORα in cholesterol metabolism comes from phenotypic examination of the RORα-deficient staggerer mouse (RORαsg/sg). Staggerer mice have decreased expression of the reverse cholesterol transporters Abca1 and Abca8/g1 in their liver and intestine.22 On a normal diet, staggerer mice have lower levels of total plasma cholesterol, high-density lipoprotein, apolipoprotein A1, apolipoprotein CIII, apolipoprotein A2 and triglycerides compared with wild-type mice.22, 23
With these considerations in mind, we hypothesized that polymorphisms in the RORα gene might modulate susceptibility to COPD. To test this hypothesis, we investigated the association of common genetic variants in the RORα gene with the risk of COPD in a Chinese Han population.
Materials and methods
Subjects
As described previously,24, 25 279 patients with COPD and 367 age-matched non-COPD control subjects were recruited for this study. The subjects in both groups were unrelated ethnic Han Chinese individuals recruited from Chengdu city or surrounding regions in the Sichuan province of western China. All subjects underwent physical examinations including chest X-ray, anthropometric measurements including body mass index (BMI), assessment of lung function and blood sampling. The recruitment and the clinical analyses were conducted at the Department of Respiratory Medicine in West China Hospital of Sichuan University; clinical analyses were performed according to the Global Initiative for Chronic Obstructive Lung Disease (GOLD) criteria.26 COPD patients were enrolled when they suffered from cough, sputum production and dyspnea at least upon exertion and showed chronic irreversible airflow limitation defined by an FEV1 (forced expiratory volume in 1 s) to FVC (forced vital capacity) ratio <70%, and FEV1 predicted <80% after the inhalation of a β2 agonist. Patients were excluded from this study if they had other significant respiratory diseases, such as bronchial asthma, bronchiectasis, lung cancer or pulmonary tuberculosis based on their chest X-ray test. Atopic patients determined by the serum levels of the total and allergen-specific IgE were also excluded from this study. The age-matched non-COPD control subjects were volunteers who came to the West China Hospital of Sichuan University for physical examination only. The inclusion criteria for controls were as follows: (1) FEV1/FVC ratio >70%, FEV1% and FVC% predicted >80% and (2) without pulmonary disease. Individuals were excluded if they had a history of chronic lung disease, atopy, an acute pulmonary infection in the 4 weeks before assessment for this study or a family history of COPD.
This study was approved by the Ethical Committee of the West China Hospital, Sichuan University, and written informed consent was obtained from all subjects before their participation in the study. The investigator explained the nature, purpose and risks of the study and provided the subject with a copy of the information sheet.
Biochemical measurements
Blood samples were collected at baseline from patients and controls after an overnight fast. Plasma separated from cells by centrifugation at 500 g for 10 min at room temperature was used for lipid and glucose analyses. The plasma levels of total cholesterol, triglycerides and glucose were determined with an enzymatic kit (Boehringer Mannheim, Mannheim, Germany) and calibrated with a plasma calibrator. Serum total and allergen-specific IgE were assessed using the ImmunoCAP System (Thermo Fisher Scientific, Uppsala, Sweden). Serum-specific IgE was determined against common inhalant allergens of birch, timothy, mugwort, Dermatophagoides pteronyssinus and farinae, horse, dog and cat epithelium and Cladosporium herbarum. Atopic sensitization was indicated if the individual had at least one allergen-specific serum IgE level ⩾0.35 kU l−1.
SNP selection and genotyping
RORα is located on chromosome 15q and spans ∼730 kilobases (RORA: ENST00000069667) (http://www.ensembl.org/index.html). Genotype data of the Chinese population for the RORα region were obtained from the HapMap website (http://www.hapmap.org/), and nine tag single-nucleotide polymorphisms (SNPs) were selected using the Tagger software implemented in the Haploview software,27 with an r2 threshold of 0.8 and minor allele frequencies of 0.1 (Supplementary Table 1).
Genomic DNA was extracted from peripheral blood leukocytes using a commercial extraction kit (Bioteke Corporation, Beijing, China) according to the manufacturer’s instructions. SNPs were genotyped using the ABI SNaPshot method (Applied Biosystems, Foster City, CA, USA) as described previously.25 The genomic regions of interest were amplified by primers shown in Supplementary Table 1. The PCR products were then purified by incubating with shrimp alkaline phosphatase and exo-nuclease I. The purified PCR products were used as the templates for SNaPshot reaction using the specific SNaPshot primers (Supplementary Table 1). Next, 3 μl of pooled PCR products, 1 μl of pooled SNaPshot primers and 1 μl of deionized water were incubated in a GeneAmp 9600 thermal cycler (Applied Biosystems, Carlsbad, CA, USA) by 25 cycles at 96 °C for 10 s, 50 °C for 5 s and 60 °C for 30 s, and finally 60 °C for 30 s. Then, 1 U of shrimp alkaline phosphatase was added to SNaPshot product and incubated at 37 °C for 1 h to deactivate the enzyme. The SNaPshot reaction products were mixed with Hi-Di formamide and GeneScan-120 LIZ internal size standard (Applied Biosystems), and analyzed on an ABI 3130 Genetic Analyzer (Applied Biosystems). The data were analyzed by the software of GeneMapper 4.0 (SoftGenetics, LLC., State College, PA, USA). Genotype analysis was performed in a blinded manner so that the staff was unaware of the cases or control status. For quality control, a 10% masked random sample of cases and controls was tested repetitively by different investigators and all the results were completely concordant.
Statistical analyses
The demographic and clinical data between the COPD patients and the control subjects were compared using the χ2 test and Student’s t-test. A two-sided significance level of α<0.05 was used for all significant tests. Statistical analyses were performed in SPSS version 17.0 (SPSS Inc, Chicago, IL, USA) and Microsoft Excel (Microsoft Corporation, Redmond, WA, USA).
The Hardy–Weinberg equilibrium test using two-sided χ2 analysis was done for each SNP among cases and controls. Differences in the distribution of genotypes or alleles under different genetic models (including dominant, recessive and additive models) between the COPD patients and the controls were estimated by using the χ2 test, and the best genetic model for each SNP was determined using Akaike’s information criterion. Odds ratios (ORs) and 95% confidence intervals (CIs) were calculated by unconditional logistic regression analyses.28, 29 Multiple testing corrections were carried out using false discovery rate (FDR).30 Q-values (=corrected P-values) were adjusted with gender, age, BMI and cigarette smoking. The significance level was set at Q<0.05. FDR calculations were done using R language package fdrtool (http://strimmerlab.org/software/fdrtool/index.html). In addition to the overall association analysis, we performed a stratified analysis according to BMI and smoking status to explore the association between genotypes and the risk of COPD in each stratum.
Pairwise linkage disequilibrium (LD) estimation and haplotype reconstruction were performed using SHEsis (http://analysis.bio-x.cn).31 For haplotype analysis, only haplotypes with a frequency of >3% in at least one group were tested. We also used Haploview 4.2 to estimate LD.27
Results
General characteristics of the subjects
The baseline characteristics, biochemical features and the results of the pulmonary function tests for the 279 patients with COPD and 367 control subjects are presented in Table 1. All patients had FEV1 values <80% of predicted and thus were diagnosed with moderate-to-severe COPD according to the Global Initiative for Chronic Obstructive Lung Disease. The COPD cases and control subjects did not significantly differ in sex, age or smoking history. The FEV1, FEV1/predicted and FEV1/FVC were significantly lower in the COPD patients compared with the controls (P<0.01). Compared with control subjects, the COPD patients showed statistically higher glucose concentrations (5.86±0.16 vs 5.13±0.12 mmol l−1, P<0.01) and lower BMI (22.03±2.27 vs 23.91±2.48 kg m−2, P<0.01). The serum levels cholesterol, triglycerides and total IgE had no difference between COPD patients and control subjects.
Distribution of the SNPs in RORα between COPD patients and controls
Nine SNPs in RORα, including rs17270181, rs1898413, rs17270216, rs8033552, rs8036966, rs7169364, rs340002, rs340023 and rs11630262, were screened in all 279 patients with COPD and 367 controls using the SNaPshot method. The genotype and allele frequencies of each SNP in both COPD patients and controls are presented in Table 2. All of the tested SNPs did not significantly deviate from that expected for a Hardy–Weinberg equilibrium in the COPD patients and controls (Table 2, all P-values were >0.05), illustrating that our subjects presented the source population well.
We compared the differences in frequency distributions of genotypes or alleles of every SNP between COPD patients and controls by χ2 test. As shown in Table 2, significant differences in allele or genotype frequencies were observed between COPD patients and controls at rs8033552 (allele: P=0.0001, FDR Q=0.004, OR: 1.62 and 95% CI: 1.27–2.07; genotype: P=0.0005, FDR Q=0.008).
Association of genotypes with COPD under different genetic models
For each SNP, if one allele frequency is relatively lower compared with another one, it is recognized as the minor allele (Table 2). We assumed that the minor allele of each SNP was a risk allele compared with the wild-type allele. We compared the genotype frequencies of every polymorphism between groups under the dominant, recessive and additive genetic models, respectively. As shown in Table 3, the minor allele A at rs8033552 was observed to be associated with an increasing COPD risk using an additive model as determined by Akaike information criterion (AG vs GG: P=0.004, FDR Q=0.019, OR: 1.62, 95% CI: 1.17–2.26; AA vs GG: P=0.001, FDR Q=0.011, OR: 2.69, 95% CI: 1.47–4.93).
The association between the rs8033552 genotypes and the risk of COPD was further investigated after stratification according to BMI and smoking status (Table 4). Compared with the genotype GG at rs8033552, genotype AG or AA was associated with a significantly increased risk of COPD in lower-BMI subjects (AG vs GG, P=0.017, FDR Q=0.038, OR: 1.74, 95% CI: 1.10–2.73; AA vs GG: P=0.003, FDR Q=0.018, OR: 2.88, 95% CI: 1.30–6.36), whereas there was no association in heavier subjects with BMI more than 22 kg m−2. When stratified by the median pack-years of smoking, the minor allele A at rs8033552 significantly increased the risk of COPD in heavy smokers under additive model (AG vs GG, P=0.002, FDR Q=0.016, OR: 1.84, 95% CI: 1.26–2.70; AA vs GG: P=0.009, FDR Q=0.027, OR: 2.51, 95% CI: 1.25–5.08).
LD between SNPs and haplotype analysis
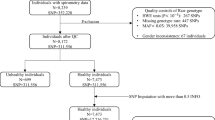
The extent of LD in pairwise combinations of alleles in different SNPs was estimated by means of maximum likelihood from the genotype frequency in the COPD and control groups. Pairwise LD between the nine SNPs is shown in Table 5 and Figure 1. Based on LD determinations, two blocks with moderate LD were detected: block 1 is composed of rs17270181 and rs1898413 and block 2 is composed of rs340002, rs340023 and rs11630262.
Linkage disequilibrium (LD) plots for retinoic acid receptor-related orphan receptor-α (RORα). The LD plots were generated by Haploview 4.2. Polymorphisms are identified by their single-nucleotide polymorphism database (dbSNP) rs numbers. The numbers within squares indicate the D′ value, expressed as a percentile. A full color version of this figure is available at the Journal of Human Genetics journal online.
We estimated the frequencies of haplotypes constructed from phased multilocus genotypes in RORα. The haplotypes with a frequency >3% in at least one group were involved in the haplotype analysis (Table 5). The global result for block 1 (rs17270181 and rs1898413) was: χ2=23.32 and d.f.=3, P=3.82 × 10−6. The global result for block 2 (rs340002, rs340023 and rs11630262) was: χ2=113.98 and d.f.=4, P=4.31 × 10−18. The overall frequency distribution of haplotype composed of all nine SNPs was significantly different between cases and controls (total global χ2=90.72 and d.f.=9, P=4.22 × 10−15).
The results of the association between the RORα haplotype and the risk of COPD are listed in Table 6. Haplotype AA in block 1 was found to be associated with an increased risk of COPD (OR: 1.39, 95% CI: 1.01–1.92, P=0.042), whereas haplotype GA was not observed in COPD patients (P=2.18 × 10−6). In block 2, two haplotypes were observed to be associated with the risk of COPD (ACA: OR: 1.52, 95% CI: 1.13–2.04, P=0.006; ACG: OR: 1.71, 95% CI: 1.26–2.32, P=0.001), whereas haplotypes ATG (OR: 0.02, 95% CI: 0.00–0.13, P=1.43 × 10−5) and GCG (P=2.47 × 10−11) were protective from COPD. Global haplotype association analyses showed that three haplotypes, including GGAGATACA, GGAGATACG and GGAAATACG, were significantly associated with the risk of COPD (all P<0.01). In addition, three protective haplotypes, GGAGATGTG (OR: 0.56, 95% CI: 0.41–0.75, P=0.0001), GGAGCTGTG (OR: 0.50, 95% CI: 0.28–0.89, P=0.017) and GGAGATATG (P=1.84 × 10−6), were associated with a decreased risk of COPD.
Discussion
In this case–control study in a Han Chinese population, we carried out the first investigation of the possible association between the SNPs in RORα and COPD risk. Our current findings suggested that rs8033552 is associated with the risk of COPD. In comparison with allele G at rs8033552, the allele A could increase the risk of COPD under all dominant, recessive and additive genetic models. In addition to the genotype analysis, our study also adopted a haplotype-based approach. Haplotype analysis, in which several SNPs within the same gene are evaluated simultaneously, can provide more information than a single SNP and thus elevates the statistical power of the analysis.32 Using this approach, we provided strong support that RORα variations contributed to the susceptibility to COPD. LD analysis showed that some SNPs in RORα gene were in moderate LD, and some haplotypes with low frequency were found to affect the risk of COPD dramatically. Haplotypes GGAGATGTG, GGAGCTGTG and GGAGATATG were associated with a reductive risk of COPD, whereas haplotypes GGAGATACA, GGAGATACG and GGAAATACG increased the risk of developing COPD, indicating the complexity of RORα gene in the development of COPD.
The significant RORα variants associated with COPD in this unrelated case–control cohort occur within the intron region of the RORα that is usually removed during the gene-splicing process. Although there is no apparent functional change, intronic SNPs may modify gene function by affecting the regulation of gene expression.33 In addition, the associated SNP with the statistical signal might just play a role as a surrogate marker for the causal functional SNP or SNPs. Therefore, rs8033552 in RORα gene could be in LD with another polymorphism of the gene that may impact the RORα expression level. However, it is also likely that the causal sequence change(s) in this region has yet to be identified as suggested by analysis of the significant haplotypes. For example, SNP rs340002 was significantly associated with COPD risk as part of a haplotype but not individually (Table 6). We selected SNPs with minor allele frequencies of >10% in the Han Chinese population using HapMap project data, but this is not suited for situations where genetic architecture is such that multiple rare disease-causing variants contribute significantly to disease risk. Recent studies demonstrate that identification of rare variants may lead to critically important insights about disease etiology through implication of new genes and/or pathways.34, 35 The rare variants in the RORα gene should be investigated to clarify their susceptibility to the development of COPD.
In addition to the regulation of cholesterol/lipid metabolism, data suggest the role of RORα in inflammation that has been implicated in the development and progression of COPD.36, 37, 38 Deficiency of RORα had been reported to lead paradoxically to increased lipopolysaccharide-induced lung inflammation and decreased allergic inflammation.39, 40 Compared with the wild-type counterparts, RORα-deficient staggerer (RORαsg/sg) mice show a significantly reduced expression of several macrophage markers, such as F4/80, Mac-2, Mpeg1 and Msr1. The reduced inflammation in RORαsg/sg mice is further indicated by the greatly reduced levels of the proinflammatory cytokines interleukin-1α, -1β and -6, and tumor necrosis factor-α.41 RORα has been shown to mediate transcriptional inhibition of the pro-inflammatory transcription factor nuclear factor-κB.42 In addition, RORα is identified as a participant in cell-fate decisions in response to DNA damage, and the absence of RORα can protect against airspace enlargement in animal models of emphysema.43 These observations suggest that genetic variants of RORα might affect COPD risk through a combination of multiple pathways.
We are aware that the significant results in this study could prove to be false positives because of the relatively small sample size. The 279 COPD patients and 367 control subjects were not relatively large among COPD association studies published to date, and further studies using larger populations are needed. But even with a larger sample, the functional and biological impacts of the described polymorphisms would require further study. Given the number of processes/pathways in which RORα functions and the significance of association between RORα and COPD, it is unlikely that RORα alone contributes to the sequelae of events in COPD but rather that genes regulated by RORα, or those that regulate RORα, may influence the disease. Therefore, although one gene may be modestly associated with COPD risk, it may be the combination of variants within sets of genes that can lead to small changes in the way the genes/proteins interact that, when combined with environmental effects, can have a huge impact on biological systems culminating in disease.44 As a result, the investigation of RORα-related pathways and gene networks may lead to a better understanding of the pathophysiology of COPD.
In conclusion, our comprehensive analysis of SNPs in the RORα gene suggests that RORα genotypes and haplotypes are associated with COPD risk. Because this is the first case–control study investigating the association of RORα with the risk of COPD, additional studies are required to confirm our findings.
References
Murray, C. J. & Lopez, A. D. Evidence-based health policy—lessons from the Global Burden of Disease Study. Science 274, 740–743 (1996).
Zhong, N., Wang, C., Yao, W., Chen, P., Kang, J., Huang, S. et al. Prevalence of chronic obstructive pulmonary disease in China: a large, population-based survey. Am. J. Respir. Crit. Care. Med. 176, 753–760 (2007).
Pauwels, R. A. & Rabe, K. F. Burden and clinical features of chronic obstructive pulmonary disease (COPD). Lancet 364, 613–620 (2004).
Khoury, M. J., Beaty, T. H., Tockman, M. S., Self, S. G. & Cohen, B. H. Familial aggregation in chronic obstructive pulmonary disease: use of the loglinear model to analyze intermediate environmental and genetic risk factors. Genet. Epidemiol. 2, 155–166 (1985).
Shi, W., Chen, F. & Cardoso, W. V. Mechanisms of lung development: contribution to adult lung disease and relevance to chronic obstructive pulmonary disease. Proc. Am. Thorac. Soc. 6, 558–563 (2009).
Castaldi, P. J., Cho, M. H., Cohn, M., Langerman, F., Moran, S., Tarragona, N. et al. The COPD genetic association compendium: a comprehensive online database of COPD genetic associations. Hum. Mol. Genet. 19, 526–534 (2010).
Cho, M. H., Boutaoui, N., Klanderman, B. J., Sylvia, J. S., Ziniti, J. P., Hersh, C. P. et al. Variants in FAM13A are associated with chronic obstructive pulmonary disease. Nat. Genet. 43, 200–202 (2010).
Pillai, S. G., Ge, D., Zhu, G., Kong, X., Shianna, K. V., Need, A. C. et al. A genome-wide association study in chronic obstructive pulmonary disease (COPD): identification of two major susceptibility loci. PLoS Genet. 5, e1000421 (2009).
Wilk, J. B., Chen, T. H., Gottlieb, D. J., Walter, R. E., Nagle, M. W., Brandler, B. J. et al. A genome-wide association study of pulmonary function measures in the Framingham Heart Study. PLoS Genet. 5, e1000429 (2009).
Soler Artigas, M., Wain, L. V., Repapi, E., Obeidat, M., Sayers, I., Burton, P. R. et al. Effect of five genetic variants associated with lung function on the risk of chronic obstructive lung disease, and their joint effects on lung function. Am. J. Respir. Crit. Care. Med. 184, 786–795 (2011).
Nillawar, A. N., Joshi, K. B., Patil, S. B., Bardapurkar, J. S. & Bardapurkar, S. J. Evaluation of HS-CRP and Lipid Profile in COPD. J. Clin. Diagn. Res. 7, 801–803 (2013).
Burkart, K. M., Manichaikul, A., Wilk, J. B., Ahmed, F. S., Burke, G. L., Enright, P. et al. APOM and high-density lipoprotein are associated with lung function and percent emphysema. Eur. Respir. J. 43, 1007–1017 (2013).
Reed, R. M., Iacono, A., DeFilippis, A., Eberlein, M., Girgis, R. E. & Jones, S. Advanced chronic obstructive pulmonary disease is associated with high levels of high-density lipoprotein cholesterol. J. Heart Lung Transplant. 30, 674–678 (2011).
Iribarren, C., Jacobs, D. R. Jr., Sidney, S., Claxton, A. J., Gross, M. D., Sadler, M. et al. Serum total cholesterol and risk of hospitalization, and death from respiratory disease. Int. J. Epidemiol. 26, 1191–1202 (1997).
Tisi, G. M., Conrique, A., Barrett-Connor, E. & Grundy, S. M. Increased high density lipoprotein cholesterol in obstructive pulmonary disease (predominant emphysematous type). Metabolism 30, 340–346 (1981).
Giguere, V., Tini, M., Flock, G., Ong, E., Evans, R. M. & Otulakowski, G. Isoform-specific amino-terminal domains dictate DNA-binding properties of ROR alpha, a novel family of orphan hormone nuclear receptors. Genes Dev. 8, 538–553 (1994).
Solt, L. A. & Burris, T. P. Action of RORs and their ligands in (patho)physiology. Trends Endocrinol. Metab. 23, 619–627 (2012).
Kallen, J. A., Schlaeppi, J. M., Bitsch, F., Geisse, S., Geiser, M., Delhon, I. et al. X-ray structure of the hRORalpha LBD at 1.63 A: structural and functional data that cholesterol or a cholesterol derivative is the natural ligand of RORalpha. Structure 10, 1697–1707 (2002).
Genoux, A., Dehondt, H., Helleboid-Chapman, A., Duhem, C., Hum, D. W., Martin, G. et al. Transcriptional regulation of apolipoprotein A5 gene expression by the nuclear receptor RORα. Arterioscler. Thromb. Vasc. Biol. 25, 1186–1192 (2005).
Raspé, E., Duez, H., Gervois, P., Fiévet, C., Fruchart, J.-C., Besnard, S. et al. Transcriptional regulation of apolipoprotein C-III gene expression by the orphan nuclear receptor RORα. J. Biol. Chem. 276, 2865–2871 (2001).
Vu-Dac, N., Gervois, P., Grötzinger, T., De Vos, P., Schoonjans, K., Fruchart, J.-C. et al. Transcriptional regulation of apolipoprotein AI gene expression by the nuclear receptor RORα. J. Biol. Chem. 272, 22401–22404 (1997).
Lau, P., Fitzsimmons, R. L., Raichur, S., Wang, S. C., Lechtken, A. & Muscat, G. E. The orphan nuclear receptor, RORalpha, regulates gene expression that controls lipid metabolism: staggerer (SG/SG) mice are resistant to diet-induced obesity. J. Biol. Chem. 283, 18411–18421 (2008).
Mamontova, A., Seguret-Mace, S., Esposito, B., Chaniale, C., Bouly, M., Delhaye-Bouchaud, N. et al. Severe atherosclerosis and hypoalphalipoproteinemia in the staggerer mouse, a mutant of the nuclear receptor RORalpha. Circulation 98, 2738–2743 (1998).
Xu, S. C., Kuang, J. Y., Liu, J., Ma, C. L., Feng, Y. L. & Su, Z. G. Association between fibroblast growth factor 7 and the risk of chronic obstructive pulmonary disease. Acta. Pharmacol. Sin. 33, 998–1003 (2012).
Yuan, Y., Jiang, H., Kuang, J., Hou, X., Feng, Y. & Su, Z. Genetic variations in ADIPOQ gene are associated with chronic obstructive pulmonary disease. PLoS ONE 7, e50848 (2012).
GOLD, E., Committee. (Updated 2011). Global Strategy for the Diagnosis, Management and Prevention of chronic obstructive pulmonary disease, Global Initiative for Chronic Obstructive Lung Disease (GOLD). https://www.goldcopd.org.
Barrett, J. C., Fry, B., Maller, J. & Daly, M. J. Haploview: analysis and visualization of LD and haplotype maps. Bioinformatics 21, 263–265 (2005).
Bland, J. M. & Altman, D. G. Statistics notes. The odds ratio. BMJ 320, 1468 (2000).
Altman, D. G. & Bland, J. M. How to obtain the confidence interval from a P value. BMJ 343, d2090 (2011).
Benjamini, Y. & Hochberg, Y. Controlling the false discovery rate: a practical and powerful approach to multiple testing. J. R. Stat. Soc. Series B. Stat. Methodol. 57, 289–300 (1995).
Shi, Y. Y. & He, L. SHEsis, a powerful software platform for analyses of linkage disequilibrium, haplotype construction, and genetic association at polymorphism loci. Cell. Res. 15, 97–98 (2005).
Morris, R. W. & Kaplan, N. L. On the advantage of haplotype analysis in the presence of multiple disease susceptibility alleles. Genet. Epidemiol. 23, 221–233 (2002).
Korb, M., Ke, Y. B. & Johnson, L. F. Stimulation of gene expression by introns: conversion of an inhibitory intron to a stimulatory intron by alteration of the splice donor sequence. Nucl. Acids Res. 21, 5901–5908 (1993).
Cole, J. W., Stine, O. C., Liu, X., Pratap, A., Cheng, Y., Tallon, L. J. et al. Rare variants in ischemic stroke: an exome pilot study. PLoS ONE 7, e35591 (2012).
Nelson, M. R., Wegmann, D., Ehm, M. G., Kessner, D. St, Jean, P., Verzilli, C. et al. An abundance of rare functional variants in 202 drug target genes sequenced in 14002 people. Science 337, 100–104 (2012).
Barnes, P. J. New anti-inflammatory targets for chronic obstructive pulmonary disease. Nat. Rev. Drug Discov. 12, 543–559 (2013).
Garcia-Rio, F., Miravitlles, M., Soriano, J. B., Munoz, L., Duran-Tauleria, E., Sanchez, G. et al. Systemic inflammation in chronic obstructive pulmonary disease: a population-based study. Respir. Res. 11, 63 (2010).
Kolsum, U., Roy, K., Starkey, C., Borrill, Z., Truman, N., Vestbo, J. et al. The repeatability of interleukin-6, tumor necrosis factor-alpha, and C-reactive protein in COPD patients over one year. Int. J. Chron. Obstruct. Pulmon. Dis. 4, 149–156 (2009).
Stapleton, C. M., Jaradat, M., Dixon, D., Kang, H. S., Kim, S. C., Liao, G. et al. Enhanced susceptibility of staggerer (RORalphasg/sg) mice to lipopolysaccharide-induced lung inflammation. Am. J. Physiol. Lung. Cell. Mol. Physiol. 289, L144–L152 (2005).
Jaradat, M., Stapleton, C., Tilley, S. L., Dixon, D., Erikson, C. J., McCaskill, J. G. et al. Modulatory role for retinoid-related orphan receptor alpha in allergen-induced lung inflammation. Am. J. Respir. Crit. Care. Med. 174, 1299–1309 (2006).
Kang, H. S., Okamoto, K., Takeda, Y., Beak, J. Y., Gerrish, K., Bortner, C. D. et al. Transcriptional profiling reveals a role for RORalpha in regulating gene expression in obesity-associated inflammation and hepatic steatosis. Physiol. Genomics 43, 818–828 (2011).
Delerive, P., Monte, D., Dubois, G., Trottein, F., Fruchart-Najib, J., Mariani, J. et al. The orphan nuclear receptor ROR alpha is a negative regulator of the inflammatory response. EMBO Rep. 2, 42–48 (2001).
Shi, Y., Cao, J., Gao, J., Zheng, L., Goodwin, A., An, C. H. et al. Retinoic acid-related orphan receptor-alpha is induced in the setting of DNA damage and promotes pulmonary emphysema. Am. J. Respir. Crit. Care. Med. 186, 412–419 (2012).
Chen, Y., Zhu, J., Lum, P. Y., Yang, X., Pinto, S., MacNeil, D. J. et al. Variations in DNA elucidate molecular networks that cause disease. Nature 452, 429–435 (2008).
Acknowledgements
This study was supported by the National High-tech R&D Program of China (863 Program 2014AA021604), National Natural Science Foundation of China (Grant 31071108) and the Program for New Century Excellent Talents in University, Education Ministry of China (Grant NCET-10-0600).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Additional information
Supplementary Information accompanies the paper on Journal of Human Genetics website
Supplementary information
Rights and permissions
About this article
Cite this article
Yuan, Y., Hou, X., Zhang, J. et al. Genetic variations in RORα are associated with chronic obstructive pulmonary disease. J Hum Genet 59, 430–436 (2014). https://doi.org/10.1038/jhg.2014.48
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/jhg.2014.48
This article is cited by
-
Genetic variants of CDH13 determine the susceptibility to chronic obstructive pulmonary disease in a Chinese population
Acta Pharmacologica Sinica (2016)