Abstract
This study described the clinical and molecular genetic features of classical galactosemia in Korean population to contribute to the insight in the spectrum of galactosemia in the world, as little is known about the spectrum and incidence of galactosemia in Asia. During the 11-year study period, only three Korean children were identified as having classical galactosemia on the basis of the enzymatic and molecular genetic analysis. Asians have been reported to have mutations distinct from those of Caucasians and African Americans, indicating that galactose-1-phosphate uridyltransferase mutations are ethnically diverse. Our three patients had a total of three mutations (c.252+1G>A, p.Q169H and p.E363K), two of which were novel (p.E363K and c.252+1G>A) mutations. Interestingly, c.252+1G>A, which leads to skipping of exon 2, was observed in all three patients (three of six alleles), indicating that this mutation may be common in Koreans with classical galactosemia. Screening for classical galactosemia in 158 126 Korean newborns identified no patient with classical galactosemia. In conclusion, our findings provide further evidence for the ethnic diversity of classical galactosemia, which may be as rare in Koreans as in other Asian populations.
Similar content being viewed by others
Main
Classical galactosemia (OMIM 230400) is caused by a deficiency in galactose-1-phosphate uridyltransferase (GALT; EC2.7.712). Classical galactosemia is characterized by more severe clinical manifestations than the other two types, galactosemia II or III, with newborns usually manifesting symptoms within a few days of birth after milk feeding.1, 2, 3
The incidence of classical galactosemia in western Europe has been estimated to be between 1:23 000 and 1:89 000.1, 4, 5 In Korean newborns, the overall incidence of the three types of galactosemia have been reported to be approximately 1:40 000,6 but the exact incidence of classical galactosemia is not yet known. Since the first report of a mutation in the GALT gene,7 more than 200 different mutations have been identified with missense mutations being observed most commonly (http://www.hgmd.org).1, 8 The most common mutations in Caucasian and African American populations are p.Q188R and p.S135L, respectively,9, 10, 11 but neither of these mutations have been detected to date in Asian populations. Similarly, Japanese patients have distinct mutations, such as p.V85_N97delinsRfsX8, p.W249X and p.R231H, which have not been observed in Caucasians and African Americans, providing further evidence for genetic heterogeneities among ethnic groups.1, 12, 13
Between March 1999 and May 2010, only three unrelated Korean patients were diagnosed with classical galactosemia at the Asan Medical Center, Seoul, Korea, with the diagnosis of each confirmed by enzyme assays and molecular genetic analysis (Table 1). All patients were identified by neonatal screening program performed at 3–5 days of life. Patients 1 and 2 had neonatal jaundice with slightly increased serum hepatic enzyme concentrations, which was not progressive, whereas patient 3 had clinically deteriorated and showed progressive jaundice and a bleeding tendency, while awaiting the results of screening tests that were reported on the eleventh day after birth (Table 1). Median total plasma galactose concentration was 50 mg per 100 ml (range, 13.5–68.9 mg per 100 ml; normal range <13 mg per 100 ml) and median erythrocyte galactose-1-phosphate concentration was 10.4 mg per 100 ml (range 1.60–62.8 mg per 100 ml; normal range <0.3 mg per 100 ml). The GALT activity was decreased in all patients, ranging from 0.1 to 0.8 umol hr–1 per gram hemoglobin (median, 0.3umol hr–1 per gram hemoglobin; normal range, 25.7±3.6 umol hr–1 per gram hemoglobin) (Table 1). A galactose-restricted diet was effective in decreasing galactose and galactose-1-phosphate concentrations in all patients. The hepatic dysfunction, jaundice and coagulopathy observed in patient 3 were resolved by supportive care by 2 months of age. Although neonatal screening has reduced early morbidity and mortality in classical galactosemia, by allowing these infants to be fed a galactose-eliminated diet, as in our patients (patient 1–2), some patients (for example, patient 3) manifest the full spectrum of disease while awaiting the results of screening tests, indicating the existence of phenotypic diversity in classical galactosemia.
Patients were followed until the age of 1.5–10.8 years (median, 3.4 years), and all three patients showed normal neurocognitive development and normal growth profiles in height (range, –0.87 to 0.54 s.d. score; median, −0.53 s.d. score) and weight (range, −0.50 to 0.07 s.d. score; median, −0.45 s.d. score). Patient 1, at the age of 10.8 years showed normal cognitive function without speech or language delay and early pubertal stage of sexual maturity rating II (Table 1). It is necessary to assess our patients over the long term, because long-term evaluation has shown that patients with classical galactosemia might experience learning disabilities, dyspraxia, mental retardation and/or ovarian failure despite early detection and intervention.1, 14
In total, 11 exons of the GALT gene and their flanking intronic sequences except promoter region were amplified by PCR, and the products were sequenced using BigDye v.3.1 (Applied Biosystems, CA, USA). Two missense mutations, p.Q169H and p.E363K, and one splicing mutation, c.252+1G>A, were identified in our three patients (Table 1). The p.E363K and c.252+1G>A mutations have not been previously described. p.E363K was not detected in 100 normal Korean subjects. Although in vitro expression was not assessed, p.E363K mutation resulted in decreased in vivo GALT activity as a member of compound heterozygotes. Aberrant splicing caused by the c.252+1G>A mutation, led to the skipping of exon 2, as confirmed by sequencing of complementary DNA isolated from blood leukocytes of patient 1 (Figure 1). Interestingly, c.252+1G>A mutation, was observed in all the three patients (three of six alleles), indicating that this mutation may be common in Koreans with classical galactosemia.
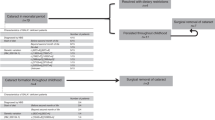
With the assumption that classical galactosemia might be rarer in Koreans than in other populations, we screened for classical galactosemia in a total of 158 126 Korean newborns, aged 3–5 days, at the Green Cross Reference Laboratory, Seoul, Korea from January 2008 to September 2009. Total galactose, free galactose and galactose-1-phosphate concentrations, in dried blood spots were measured using an Enzyme Colorimetric Assay as described.15 A total of 1299 (0.82%) subjects with total galactose concentrations greater than 13 mg per 100 ml were selected. Total galactose concentrations were re-measured in 1207 of these 1299 newborns (92.9%), with 99 (0.06%) again showing abnormal total galactose concentrations. Analysis of the GALT gene in the genomic DNA of peripheral leukocytes drawn from all 99 newborns showed that only one subject has D/G galactosemia (p.N314D and R200X) with moderately decreased GALT activity (4.3 umol hr–1 per gram hemoglobin) but without any clinical manifestations. Another subject carried a heterozygous Duarte variant (p.N314D). Patients 1–3 were not included in this cohort. Duarte variant is a polymorphic variant of the GALT gene with reduced enzyme activity. It is relatively common with the estimated prevalence of 2–6% (2% in Korean population) in various populations.16, 17 It might have a clinical significance in combination with other GALT mutations, so-called D/G galactosemia, whereas no clinical manifestation was noted on the subject with p.N314D and R200X.
Nationwide newborn screening for galactosemia, first introduced in Korea in 1991,6 is now performed in more than 90% of Korean newborns. The institute that participated in the current study is one of the largest centers in Korea screening newborns, accounting for approximately 25% of Korean newborns annually.6 Although the accurate prevalence of classical galactosemia in Korean population cannot be estimated from the results of our study that failed to identify a patient in 158 126 Korean newborns, the results imply that classical galactosemia is much rarer in Korean population than in western countries.1, 4, 5 The results of studies in other east Asian countries, including China, Japan and Taiwan, where the prevalence of classical galactosemia has been estimated to be between 1:400 000 and 1:1 000 000.18, 19, 20 Taken together, these data strongly indicate genetic diversity according to ethnicity.1, 10, 21
In conclusion, we have shown here that the classical galactosemia caused by GALT deficiency is very rare in the Korean population and that a splicing mutation (c.252+1G>A) may be common in Korean patients with classical galactosemia. Identification and evaluation of a larger number of Korean patients with classical galactosemia are required to verify these genetic characteristics.
References
Bosch, A. M. Classical galactosaemia revisited. J. Inherit. Metab. Dis. 29, 516–525 (2006).
Bosch, A. M., Bakker, H. D., van Gennip, A. H., van Kempen, J. V., Wanders, R. J. & Wijburg, F. A. Clinical features of galactokinase deficiency: a review of the literature. J. Inherit. Metab. Dis. 25, 629–634 (2002).
Timson, D. J. The structural and molecular biology of type III galactosemia. IUBMB Life 58, 83–89 (2006).
Shih, V. E., Levy, H. I., Karolkewicz, V., Houghton, S., Efron, M. L., Isselbacher, K. J. et al. Galactosemia screening of newborns in Massachusetts. N. Engl. J. Med. 284, 753–757 (1971).
Schweitzer, S. Newborn mass screening for galactosemia. Eur. J. Pediatr. 154, S37–S39 (1995).
Lee, D. H. Newborn screening of inherited metabolic disease in Korea. J. Koera. Pediatr. Soc. 49, 1125–1139 (2006) Korean.
Leslie, N. D., Immerman, E. B., Flach, J. E., Florez, M., Fridovich-Keil, J. L. & Elsas, L. J. The human galactose-1-phosphate uridyltransferase gene. Genomics 14, 474–480 (1992).
Calderon, F. R., Phansalkar, A. R., Crockett, D. K., Miller, M. & Mao, R. Mutation database for the galactose-1-phosphate uridyltransferase (GALT) gene. Hum. Mutat. 28, 939–943 (2007).
Gort, L., Boleda, M. D., Tyfield, L., Vilarinho, L., Rivera, I., Cardoso, M. L. et al. Mutational spectrum of classical galactosaemia in Spain and Portugal. J. Inherit. Metab. Dis. 29, 739–742 (2006).
Tyfield, L., Reichardt, J., Fridovich-Keil, J., Croke, D. T., Elsas, L. J. II., Strobl, W. et al. Classical galactosemia and mutations at the galactose-1-phosphate uridyl transferase (GALT) gene. Hum. Mutat. 13, 417–430 (1999).
Lai, K., Langley, S. D., Singh, R. H., Dembure, P. P., Hjelm, L. N. & Elsas, L. J. II. A prevalent mutation for galactosemia among black Americans. J. Pediatr. 128, 89–95 (1996).
Hirokawa, H., Okano, Y., Asada, M., Fujimoto, A., Suyama, I. & Isshiki, G. Molecular basis for phenotypic heterogeneity in galactosaemia: prediction of clinical phenotype from genotype in Japanese patients. Eur. J. Hum. Genet. 7, 757–764 (1999).
Ashino, J., Okano, Y., Suyama, I., Yamazaki, T., Yoshino, M., Furuyama, J. et al. Molecular characterization of galactosemia (type 1) mutations in Japanese. Hum. Mutat. 6, 36–43 (1995).
Schweitzer-Krantz, S. Early diagnosis of inherited metabolic disorders towards improving outcome: the controversial issue of galactosaemia. Eur. J. Pediatr. 162, S50–S53 (2003).
Diepenbrock, F., Heckler, R., Schickling, H., Engelhard, T., Bock, D. & Sander, J. Colorimetric determination of galactose and galactose-1-phosphate from dried blood. Clin. Biochem. 25, 37–39 (1992).
Suzuki, M., West, C. & Beutler, E. Large-scale molecular screening for galactosemia alleles in a pan-ethnic population. Hum. Genet. 109, 210–215 (2001).
Ko, D. H., Chang, H. E., Song, S. H., Park, K. U., Kim, J. Q., Kim, M. C. et al. Molecular and biochemical characterization of the GALT gene in Korean patients with galactose-1-phosphate uridyltransferase deficiency. Clin. Chim. Acta. 411, 1506–1510 (2010).
Cheung, K. L., Tang, N. L., Hsiao, K. J., Law, L. K., Wong, W., Ng, P. C. et al. Classical galactosaemia in Chinese: A case report and review of disease incidence. J. Paediatr. Child Health 35, 399–400 (1999).
Tada, K., Tateda, H., Arashima, S., Sakai, K., Kitagawa, T., Aoki, K. et al. Follow-up study of a nation-wide neonatal metabolic screening program in Japan. A collaborative study group of neonatal screening for inborn errors of metabolism in Japan. Eur. J. Pediatr. 142, 204–207 (1984).
Chen, R. G., Sun, M., Ni, Y. Y., Pan, X. S., Chen, J. Z., Zhang, Y. F. et al. Neonatal hypothyroidism, phenylketonuria and galactosemia screening in metropolitan Shanghai. Chin. Med. J. (Engl.) 97, 61–65 (1984).
Novelli, G. & Reichardt, J. K. Molecular basis of disorders of human galactose metabolism: past, present, and future. Mol. Genet. Metab. 71, 62–65 (2000).
Acknowledgements
We thank our patients and their family members for their participation in this study. This study was supported in part by Grant A080588 from the Korean Ministry of Health, Welfare and Family Affairs.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Rights and permissions
About this article
Cite this article
Lee, B., Cheon, C., Kim, JM. et al. Low prevalence of classical galactosemia in Korean population. J Hum Genet 56, 94–96 (2011). https://doi.org/10.1038/jhg.2010.152
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/jhg.2010.152
Keywords
This article is cited by
-
Novel GALTvariations and mutation spectrum in the Korean population with decreased galactose-1-phosphate uridyltransferase activity
BMC Medical Genetics (2014)
-
Diversity of approaches to classic galactosemia around the world: a comparison of diagnosis, intervention, and outcomes
Journal of Inherited Metabolic Disease (2012)