Abstract
The production process, such as fermentation and purification etc., can significantly affect the relative ratio of matrix components in a multi-component antibiotic. The ratio of components can be varied in different products. This status causes a difficulty to assure the homogeneity and consistency between reference standards and test samples in potency determination, which hinders the results judgment and accuracy of a routine microbiological assay. In the current study, a multi-component antibiotic, teicoplanin, was selected as a model to explore the relationship between the ratio of matrix component and antibiotics potency. Single-component samples, TA3-1, TA2-1, and mixed-component samples, TA2-2.3, TA2-4.5, of teicoplanin were prepared and purified. Dose–response relationship of each sample has been determined by HPLC and microbiological assay, respectively. The accuracy of the potency result was guaranteed by choosing a test organism with the same sensitivity to each component of teicoplanin when there were differences existing in the ratio of components between the reference standard and the test sample. The experimental methods in current specifications can be replaced with the new potency determination method, which can provide a more realistic reflection of the biological activity of the product.
Similar content being viewed by others
Introduction
Teicoplanin, discovered in 1975, is a glycopeptide antibiotic produced by the actinomycete Actinoplanes teichomyceticus. Its bioactive mechanism is similar to other glycopeptide antibiotics, such as vancomycin. Teicoplanin will hinder the growth of bacteria by binding peptidoglycan synthesis precursor specifically to inhibit the biosynthesis of cell wall.1 It can also accumulate UDP-N-acetylmuramic acid pentapeptide to inhibit the growth of bacteria.2 Teicoplanin has significant antimicrobial activity against Gram-positive cocci, including Staphylococcus aureus, S. epidermidis, Streptococcus pyogenes, S. pneumoniae, S. faecalis, S. viridans, and Gram-positive anaerobes, as well as against methicillin-resistant S. aureus and methicillin-resistant S. epidermidis.3, 4, 5, 6 The matrix composition of Teicoplanin has five components with a similar structure (Teicoplanin A 2-1, TA2-1, Teicoplanin A 2-2, TA2-2, Teicoplanin A 2-3, TA2-3, Teicoplanin A 2-4, TA2-4, Teicoplanin A 2-5, TA2-5). The degradation products of TA2 and TA3-1 (deacyl glucosamine product), such as two more lipophilic analogs (RS-1, RS-2) and two less lipophilic analogs (RS-3 RS-4) are also considered to be the active components.7, 8, 9 Figure 1 shows main matrix components chemical structures; TA2-2 and TA2-3, TA2-4, and TA2-5 are isomers.
Teicoplanin is newly added into the 2010 edition of the Chinese Pharmacopoeia.10 It is included in both European Pharmacopoeia 7.011 and Japanese Pharmacopoeia XVI,12 but is excluded in United States Pharmacopoeia 36 (NF31).13 In addition to Sanofi-Aventis (Shanghai, China) has its specific import registration specification, JX20040258, to import teicoplanin for injection. HPLC purity and microbiological potency are required simultaneously in all above specifications for teicoplanin quality control. HPLC conditions and its purity limit are same across specifications, as well as potency limits assayed by same test organism, Bacillus subtilis (ATCC6633). Except for these, the media and buffers used in microbiological assay are varied in different specifications, and we have found that same teicoplanin materials can gain different potency results based on different specifications. Those made the potency results difficult to compare. Recently, compendial globalization, a new concept discussed, address to provide harmonized, globally applicable specifications for medicines within the existing framework of multiple national and regional pharmacopeias to the benefit of patients worldwide.14 We hoped to establish an ideal potency assay method instead of the methods described in current pharmacopeias to overcome the problem above.
According to some pilot examination, teicoplanin products produced by different manufacturers might be classified into three types depending on differences in ratio of main matrix components which constituted teicoplanin. Type 1 (manufactured in France) included a relative amount of main component TA2-2 was between 40 and 50% and other two components TA2-4 and TA2-5 were between 10 and 20%. Type 2 (manufactured in China and Korea) included a relative amount of main component TA2-2 was between 60 and 70% and other two components TA2-4 and TA2-5 were less than 10%;15 Type 3 was teicoplanin of our national reference standard, lot 130374-200701, used as a reference, with a relative amount of the main component TA2-2 being between 40 and 60% and other two components TA2-4 and TA2-5 being less than 10%, as well as TA2-1 being about 20%, which was significantly higher than the other two products. HPLC chromatograms of three types of teicoplanin are shown in Figure 2. Current study stressed on whether different ration of matrix components between reference standard and test samples was the reason of varied potency results using different microbiological assay methods.
Materials and methods
Instruments, samples and reagents
HPLC determination was performed on Waters 2690 Separations Module coupled with Waters 996 Photodiode Array Detector. Waters Millennium 32 Software was used for system control. Antibiotic potency measurement was achieved on CHB-1 antibiotic potency measuring instrument (Beijing Chaosheng Technique Development Company, Beijing, China) assisted by Laborota 4000 rotary evaporator (Heidolph, Schwabach, Germany) and GRP-9270 Water-jacket thermostatic incubator (Shanghai Sumsung Laboratory Instrument).
Teicoplanin national reference standard (lot no.: 130374-200701, 841 u mg−1) was obtained from National Institutes for Food and Drug Control (NIFDC). European Pharmacopoeia teicoplanin reference standard (Cat. no. Y0001102, 51550IU per ampoule) and European Pharmacopoeia teicoplanin reference substance for identification (Cat. no. Y0001047) were from European Directorate for Quality Medicines (EDQM).
Batch no. A7720, A8819 and A9924 teicoplanin for injection were produced by Sanofi-Aventis (Paris, France), as well as batch no. 100715, 100720 and 100722 by Zhejiang Medicine Co, Ltd Xinchang Pharmaceutical Factory (Zhejiang, China).
Except acetonitrile was HPLC grade from Thermo Fisher (Pittsburgh, PA, USA), other reagents used in this study, sodium phosphate monobasic dehydrate (NaH2PO4·2H2O), potassium phosphate monobasic (KH2PO4), potassium hydrogen phosphate (K2HPO4) and sodium hydroxide (NaOH) were all analytical grade purchased from Beijing Chemical Reagents Company, China. Antibiotic test medium I (pH 7.8–8.0) and antibiotic test medium II (pH 6.5–6.6) were provided by the National Institutes for Food and Drug Control. MH solid medium was purchased from Bio-rad Company, Hercules, CA, USA. Experimental strains, B. pumilus [ATCC6633], and S. aureus [ATCC29213] were provided by National Center for Surveillance of Antimicrobial Resistance, as well as strains for determination of MIC values were provided by the Center for Surveillance of Resistance of State Food and Drug Administration, China.
HPLC method of teicoplanin components
The HPLC method used to determine the content of teicoplanin components followed the instruction described in the 2010 edition of the Chinese Pharmacopoeia.10 Briefly, all separation was performed with Hypersil BDS C18 column, 5 μm, 4.6 × 250 mm2 under detecting wavelength 254 nm and a flow rate of 1.8 ml min−1. Gradient elution program is shown in Table 1, while mobile phase A was 0.4% sodium phosphate monobasic dehydrate solution in water and acetonitrile mixture (17:3), pH 6.0 adjusted by sodium hydroxide TS, as well as mobile phase B was 0.4% sodium phosphate monobasic dehydrate solution in water and acetonitrile mixture (6:14), pH 6.0 adjusted by sodium hydroxide TS. Injection volume for all samples was 20 μl.
Main teicoplanin matrix components preparation
Main matrix components of teicoplanin were separated and prepared by HPLC described above. Teicoplanin powder was dissolved in water to obtain a solution of 25 mg ml−1. With 100 μl injection volume, the peaks were collected based on retention time, shown in Figure 3. Organic solvent was removed by rotary evaporation at 60 °C. The final matrix components, single-component samples TA3-1, TA2-1, mixed-component samples TA2-2 and TA2-3, mixed-component samples TA2-4 and TA2-5 of teicoplanin, were obtained by freeze drying, respectively.
Microbiological assay
Four microbiological assay methods were used in current study based on different pH in culture medium or buffer solution. Method 1 used antibiotic test medium II (pH 6.5–6.6) and pH 6.0 phosphate buffer described in the 2010 edition of the Chinese Pharmacopoeia10 while the concentrations of the high and low dose solution were ∼40 and 20 u ml−1, respectively. Method 2 used antibiotic test medium I (pH 7.8–8.0) and pH 6.0 phosphate buffer, which were similar to European Pharmacopoeia 7.011 and Japanese Pharmacopoeia X VI12 while the concentrations of the high and low dose solution were ∼160 and 40 u ml−1, respectively. Method 3 used antibiotic test medium I (pH 7.8–8.0)+pH 7.8 phosphate buffer referenced from import registration specification (JX20040258) while the concentrations of the high and low dose solution were ∼20 and 10 u ml−1, respectively. As a new exploration of potency determination, Method 4 was developed which used antibiotic test medium I (pH 7.8–8.0) and pH 7.8 phosphate buffer, while the concentrations of the high- and low-dose solution were ∼200 and 100 u ml−1, respectively.
Determination method of MIC values
According to CLSI agar dilution method,16 one McF (McFarland) bacterial suspension was prepared with sterile normal saline. The suspensions were diluted with sterile normal saline in proportion of 1:100. The final solutions were inoculated onto the surface of MH agar, which contained teicoplanin components with different concentrations using multi-point inoculators. After culturing at 35±1 °C for 22–24 h, MIC values were recorded.
Results and discussion
Purity analysis of main matrix components collections of teicoplanin
Matrix components, single-component samples TA3-1, TA2-1, mixed-component samples TA2-2 and TA2-3, mixed-component samples TA2-4 and TA2-5 of teicoplanin, were analyzed for their purities with HPLC. The purities were TA3-1, 94.9%, TA2-1, 92.8%, TA2-2 and TA2-3, 98.5%, TA2-4 and TA2-5 95.4%, respectively, calculated by peak area normalization.
Dose–response relationships of main marix components of teicoplanin
B. subtilis ATCC6633 was used as the test organism to compare the dose–response relationships of matrix components in teicoplanin with methods 1 and 2, the dose–response curves of TA3-1, TA2-1, TA2-2.3 and TA2-4.5 were y=0.0049x−0.0012 (R2=0.9999), y=0.0015x−0.0005 (R2=1), y=0.001x+0.0006 (R2=1), and y=0.0009x+0.0021 (R2=0.9993) (Figure 4a), respectively, where y was content (mg mg−1) of the component, as well as x was potency (u mg−1) of the components. With methods 3, the dose–response curves of TA3-1, TA2-1, TA2-2.3 and TA2-4.5 were y=0.0068x−0.0009 (R2=1), y=0.0015x+0.0005 (R2=1), y=0.0009x−0.003 (R2=0.9998) and y=0.0007x+0.0014 (R2=0.9999) (Figure 4b), respectively. The slopes of each curves reflected significant differences between each matrix component across all three methods. Results also stated that each component had different activity on B. subtilis ATCC6633, while the activity of each component could be sorted as TA3-1<TA2-1<TA2-2.3<TA2-4.5.
According to the accuracy requirements of microbiological assay on antibiotics, reference standard and test sample should have homogeneity or consistency, while dose–response curve should be parallel between them.17, 18 For current specifications used in teicoplanin potency determination, B. subtilis ATCC6633 as the test organism had various sensitivities on different matrix components which constituted teicoplanin. The accuracy of measurement has been affected while a reference standard and a test sample from different type were used. In current study, teicoplanin national reference standard, lot 130374-200701, belonged to type 3 because of its components ratio, as well as three batches samples from type 1 and other three from type 2. All samples were determined using methods 1, 2 and 3, respectively (Table 2). The results indicated that same batch samples obtained different results for the reason of different components ratio between reference standard and test sample. The relative amount of two components, TA2-4 and TA2-5, of type 1 was higher, between 10 and 20%, although of type 3 was less than 10%. The difference in the amount of the components TA2-4.5 was about 2–4 times between these two type. The ratios of two components, TA2-4 and TA2-5, of type 2 were similar to those of type 3. B. subtilis ATCC6633 was more sensitive to components TA2-4 and TA2-5, while the results from type 1 were higher than other two type which TA2-4 and TA2-5 were lower in relative amounts.
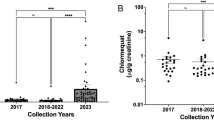
Comparison of antimicrobial activity of different components of teicoplanin
In order to demonstrate similarities and differences of the antimicrobial activity of teicoplanin components, multiple strains of clinically separated S. aureus and standard strains were used to determine MIC values of single-component samples TA3-1, TA2-1 and mixed-component samples TA2-2.3, TA2-4.5 (Table 3). MIC provided same values for different components, which shown similar biological and clinical activities of each component in teicoplanin. The results were similar with literature,19 in which the theoretical potencies of TA2-1, TA2-2, TA2-3, TA2-4 and TA2-5 were suggested as 841, 1086, 1131, 1066 and 954 u mg−1, respectively, and they displayed similar activities on antimicrobial property.
Establishment of a new method for determination of potency of teicoplanin
Test organism should provided consistent sensitivities on different matrix components in multi-components antibiotics involved in microbiological assay, which could eliminate measurement deviation and improve accuracy of results.17, 18 In Table 3, MIC values of main matrix components TA3 and TA2 showed same values, 1 μg ml−1, while using S. aureus ATCC29213 as the test organism, which was also recommended by Practical and Laboratory Standards Institute (CLSI).20 Therefore, S. aureus ATCC29213 replaced B. subtilis ATCC6633 as the test organism during the development of a new method for potency determination on teicoplanin to eliminate composition difference and promote accuracy of results. Medium and buffer solution in the new method were optimized: buffer solution was pH 7.8 phosphate buffer as well as medium was antibiotic test medium I (pH 7.8–8.0). Under these conditions, the dose–response curves (see also Figure 5) of TA3-1, TA2-1, TA2-2.3 and TA2-4.5 were y=0.0011x+0.0027, R2=0.9999, y=0.0011x+0.0055, R2=0.9991, y=0.001x−0.004, R2=0.9996, and y=0.001x+0.0076, R2=0.9987, respectively. There were no significant differences between different matrix components, which reflected better consistency and accuracy than current specifications in routine potency determination on teicoplanin.
Methodology validation
The new method, method 4, was validated in accordance with the guideline in the appendix of Volume II, the 2010 edition of the Chinese Pharmacopoeia.10
Linearity and range
In all, 30.2 mg of teicoplanin national reference standard (lot no. 130374-200701) was weighed and transferred into a 25-ml volumetric flask, dissolved with sterilized water. The solution was then diluted 1000 folds with water to be stock solution. Series standard solutions were prepared from used as stock solution diluted with pH 7.8 phosphate buffer to obtain the final concentration as 203.19, 152.39, 101.59, 50.80, 25.40 and 10.16 u ml−1. Antibiotic test medium I (pH 7.8–8.0) was used in the microbiological assay of antibiotics and the areas of antimicrobial circle were recorded. Linearity regression curve between concentration dose and the square of the radius of antimicrobial circle was y=0.2895x+2.0159, R2=0.9998, with linearity range being between 10.16–203.19 u ml−1.
Precision
The potency of same batch of sample was used to assess the precision of the method. The intra-day relative s.d. was 0.46% (numbers of repeat, n=6) and the inter-day relative s.d. was 0.91% (numbers of repeat, n=14).
Accuracy
Potencies of six batches of teicoplanin for injection, which belonged to different type (three for each), were determined with teicoplanin national reference standard lot no. 130374-200701 as reference (Table 2). The new method can effectively eliminate the difference in the components ratio between a reference standard and a test sample.
Conclusion
Because of the different sensitivities of different components of teicoplanin to test organism using potency determination methods described in published specifications, B. subtilis ATCC6633 as the test organism might induce varying results for same sample while using reference standard which belonged to different type from sample. In order to promote homogeneity and consistency between a multi-component antibiotic reference standard and test samples, MIC test was carried out on matrix components of teicoplanin by multiple standard strains. S. aureus ATCC29213, which had same sensitivities to matrix components, was selected as the test organism to establish a new method for teicoplanin potency determination. The method provided consistent results even reference and sample from different type. The result also reflected real biological activities across multi-source products.
References
Gholizadeh, Y. & Courvalin, P. Acquired and intrinsic glycopeptide resistance in enterococci. Int. J. Antimicrob. Agents 16, S11–S17 (2000).
Somma, S., Gastaldo, L. & Corti, A. Teicoplanin, a new antibiotic from Actinoplanes teichomyceticus nov. Sp. Antimicrob. Agents Chemother. 26, 917–923 (1984).
Parenti, F., Beretta, G., Berti, M. & Arioli, V. Teichomycins, new antibiotics from Actinoplanes teichomyceticus Nov. Sp. I. Description of the producer strain, fermentation studies and biological properties. J. Antibiotics 31, 276–283 (1978).
Bardone, M. R., Paternoster, M. & Coronelli, C. Teichomycins, new antibiotics from Actinoplanes teichomyceticus nov. Sp. II. Extraction and chemical characterization. J. Antibiotics 31, 170–177 (1978).
Pallanza, R. et al. Teichomycin: In vitro and in-vivo evaluation in comparison with other antibiotics. J. Antimicrob. Chemother. 11, 419–425 (1983).
Borghi, A. et al. Teichomycins, new antibiotics from Actinoplanes teichomyceticus nov. Sp. IV. Separation and characterization of the components of teichomycin (teicoplanin). J. Antibiotics 37, 615–620 (1984).
Brogden, R. N & Peters, D. H. Teicoplanin. A reappraisal of its antimicrobial activity, pharmacokinetic properties and therapeutic efficacy. Drugs 47, 823–854 (1994).
Malabarba, A. et al. Teicoplanin, antibiotics from Actinoplanes teichomyceticus nov. Sp. VI. Chemical degradation: physico-chemical and biological properties of acid hydrolysis products. J. Antibiotics 37, 988–999 (1984).
Cometti, A. et al. Isolation and structure determination of the main related substances of teicoplanin, a glycopeptide antibiotic. Farmaco. Sci. 43, 1005–1018 (1988).
The Chinese Pharmacopoeia Commission.. Pharmacopoeia of the People’s Republic of China. 2010 edn China Medical Science Press: Beijing, China, (2010).
The European Pharmacopoeia Commission. The European Pharmacopoeia 7th edn Council of Europe: Strasbourg, (2011).
The Ministry of Health, Labour and Welfare. The Japanese pharmacopoeia 16th edn Society of Japanese Pharmacopoeia: Tokyo, Japan, (2011).
The United States Pharmacopoeia Commission Inc. The United States Pharmacopeia, The United States Pharmacopeia Convention, Inc, 2013: NF31: Rockville, MD, USA, (2013).
Wiggins, J. M, Skutnik, J. A, Shimek-Cox, J. L & Schwarzwalder, N. A. The ideal pharmacopeia. Pharm. Technol 32, 122–125 (2008).
Xue, Jing, Chang, Yan, Zou, Wen-bo, Li, Ping & Hu, Chang-qin Component content analysis of teicoplanin for injection. Chinese J. Antibiotics 35, 848–851,872 (2010).
CLSI Methods for dilution antimicrobial susceptibility tests for bacteria that grow aerobically; approved standard-8th edn, January 2009. Report no.: M07-A7.
Zhang, Zhi-tan Antibiotics Drug Control, People’s Medical Publishing House, (1987).
Hu, Chang-qin & Liu, Wei Microbiological Assay of Antibiotics and Its Standard Operating, China Meteorological Press, (2004).
Borghi, A., Pallanza, R., Coronelli, C. & Cassani, G. Teicoplanin A2 pure single factors 1,2,3,4 and 5 method for their production. United States Patent: 4542018, 17 September (1985).
CLSI Performance Standards for Antimicrobial Susceptibility Testing; Nineteenth Informational Supplement, January 2009. Report no.: M02-A10 and M07-A8.
Acknowledgements
Project supported by the National Science and Technology Major Project of the Ministry of Science and Technology of China (Grant no. 2010ZX09401-403).
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Chang, Y., Wang, N., Yao, SC. et al. Exploring quality and its potential effects of multi-components antibiotic: consistency evaluation between matrix components ratio and microbiological potency of teicoplanin. J Antibiot 66, 641–646 (2013). https://doi.org/10.1038/ja.2013.66
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/ja.2013.66
Keywords
This article is cited by
-
Consistency evaluation between matrix components ratio and microbiological potency of tylosin major components
DARU Journal of Pharmaceutical Sciences (2018)