Abstract
Background:
It is postulated that obstructive sleep apnea (OSA) is a risk factor for the development of depression. However, obesity and excessive daytime sleepiness (EDS) are associated with both OSA and depression. The goal of this study was to examine the relative contribution of OSA, obesity and EDS to incident depression.
Methods:
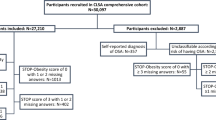
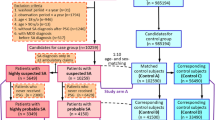
A representative random sample of 1137 adults without depression from the Penn State Adult Cohort was followed up after 7.5 years. All subjects underwent a full medical examination and polysomnography at baseline. OSA was defined as an apnea/hypopnea index (AHI) ⩾5, overweight as a body mass index (BMI) of 25–29.9 kg m−2, obesity as a BMI⩾30 kg m−2 and EDS as moderate-to-severe drowsiness/sleepiness and/or irresistible sleep attacks.
Results:
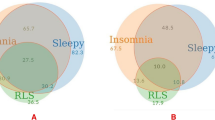
Overweight, obesity and EDS were associated with incident depression, whereas OSA alone was not. Overweight was associated with incident depression in women, while obesity and EDS were associated with incident depression in both genders. The association of overweight and obesity with incident depression was independent of premorbid emotional distress, while that of EDS was not. The association between BMI and EDS with incident depression was stronger in women 20–40 years old. The severity of EDS predicted incident depression in those with OSA, while AHI or oxygen desaturation did not.
Conclusions:
Overweight, obesity and EDS are the main predictors of incident depression. Obesity may be linked to depression through psychobiological mechanisms, while EDS may be an early sign of depression. Obesity should be a target of our preventative strategies for depression.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout


Similar content being viewed by others
References
American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders, 5th edn. American Psychiatric Association: Arlington: VA, USA, 2013.
Simon GE . Social and economic burden of mood disorders. Biol Psychiatry 2003; 54: 208–215.
Schulz R, Drayer RA, Rollman BL . Depression as a risk factor for non-suicide mortality in the elderly. Biol Psychiatry 2002; 52: 205–225.
Benca RM, Peterson MJ . Insomnia and depression. Sleep Med 2008; 9: S3–S9.
Harris M, Glozier N, Ratnavadivel R, Grunstein RR . Obstructive sleep apnea and depression. Sleep Med Rev 2009; 13: 437–444.
Baglioni C, Battagliese G, Feige B, Spiegelhalder K, Nissen C, Voderholzer U et al. Insomnia as a predictor of depression: a meta-analytic evaluation of longitudinal epidemiological studies. J Affect Disord 2011; 135: 10–19.
Peppard PE, Szklo-Coxe M, Hla KM, Young T . Longitudinal association of sleep-related breathing disorder and depression. Arch Intern Med 2006; 166: 1709–1715.
Vgontzas AN, Bixler EO, Chrousos GP . Sleep apnea is a manifestation of the metabolic syndrome. Sleep Med Rev 2005; 9: 211–224.
Kritikou I, Basta M, Vgontzas AN, Pejovik S, Liao D, Tsaoussoglou M et al. Sleep apnoea, sleepiness, inflammation and insulin resistance in middle-aged males and females. Eur Respir J 2014; 43: 145–155.
Luppino FS, de Wit LM, Bouvy PF, Stijnen T, Cuijpers P, Penninx BW et al. Overweight, obesity, and depression: a systematic review and meta-analysis of longitudinal studies. Arch Gen Psychiatry 2010; 67: 220–229.
Bixler EO, Vgontzas AN, Lin HM, Calhoun SL, Vela-Bueno A, Kales A . Excessive daytime sleepiness in a general population sample: the role of sleep apnea, age, obesity, diabetes, and depression. J Clin Endocrinol Metab 2005; 90: 4510–4515.
Vgontzas AN, Papanicolaou DA, Bixler EO, Kales A, Tyson K, Chrousos GP . Elevation of plasma cytokines in disorders of excessive daytime sleepiness: role of sleep disturbance and obesity. J Clin Endocrinol Metab 1997; 82: 1313–1316.
Vgontzas AN, Bixler EO, Chrousos GP . Obesity-related sleepiness and fatigue: the role of the stress system and cytokines. Ann NY Acad Sci 2006; 1083: 329–344.
Panossian LA, Veasey SC . Daytime sleepiness in obesity: mechanisms beyond obstructive sleep apnea—a review. Sleep 2012; 35: 605–615.
Fernandez-Mendoza J, Vgontzas AN, Kritikou I, Calhoun SL, Liao D, Bixler EO . Natural history of excessive daytime sleepiness: role of obesity, weight loss, depression, and sleep propensity. Sleep 2015; 38: 351–360.
Bixler EO, Vgontzas AN, Lin HM, Vela-Bueno A, Kales A . Insomnia in central Pennsylvania. J Psychosom Res 2002; 53: 589–592.
Bixler EO, Vgontzas AN, Ten Have T, Tyson K, Kales A . Effects of age on sleep apnea in men: I. Prevalence and severity. Am J Respir Crit Care Med 1998; 157: 144–148.
Bixler EO, Vgontzas AN, Lin HM, Ten Have T, Rein J, Vela-Bueno A et al. Prevalence of sleep-disordered breathing in women: effects of gender. Am J Respir Crit Care Med 2001; 163: 608–613.
Fernandez-Mendoza J, Vgontzas AN, Liao D, Shaffer ML, Vela-Bueno A, Basta M et al. Insomnia with objective short sleep duration and incident hypertension: the Penn State Cohort. Hypertension 2012; 60: 929–935.
Singareddy R, Vgontzas AN, Fernandez-Mendoza J, Liao D, Calhoun S, Shaffer ML et al. Risk factors for incident chronic insomnia: a general population prospective study. Sleep Med 2012; 13: 346–353.
Vgontzas AN, Fernandez-Mendoza J, Bixler EO, Singareddy R, Shaffer ML, Calhoun SL et al. Persistent insomnia: the role of objective short sleep duration and mental health. Sleep 2012; 35: 61–68.
Fernandez-Mendoza J, Vgontzas AN, Bixler EO, Singareddy R, Shaffer ML, Calhoun SL et al. Clinical and polysomnographic predictors of the natural history of poor sleep in the general population. Sleep 2012; 35: 689–697.
Fernandez-Mendoza J, Shea S, Vgontzas AN, Calhoun SL, Liao D, Bixler EO . Insomnia and incident depression: role of objective sleep duration and natural history. J Sleep Res 2015; 24: 390–398.
Rechtschaffen A, Kales A . A Manual of Standardized Terminology, Techniques and Scoring System for Sleep Stages of Human Subjects. National Institutes of Health: Bethesda, MD, USA, 1968.
Ogden CL, Carroll MD, Kit BK, Flegal KM . Prevalence of childhood and adult obesity in the United State, 2011-2012. JAMA 2014; 311: 806–814.
Vgontzas AN, Liao D, Bixler EO, Chrousos GP, Vela-Bueno A . Insomnia with objective short sleep duration is associated with a high risk for hypertension. Sleep 2009; 32: 491–497.
Vgontzas AN, Liao D, Pejovic S, Calhoun S, Karataraki M, Bixler EO . Insomnia with objective short sleep duration is associated with type 2 diabetes: a population-based study. Diabetes Care 2009; 32: 1980–1985.
Fernandez-Mendoza J, Calhoun S, Bixler EO, Pejovic S, Karataraki M, Liao D et al. Insomnia with objective short sleep duration is associated with deficits in neuropsychological performance: a general population study. Sleep 2010; 33: 459–465.
Vgontzas AN, Liao D, Pejovic S, Calhoun S, Karataraki M, Basta M et al. Insomnia with short sleep duration and mortality: the Penn State cohort. Sleep 2010; 33: 1159–1164.
Fernandez-Mendoza J, Calhoun SL, Bixler EO, Karataraki M, Liao D, Vela-Bueno A et al. Sleep misperception and chronic insomnia in the general population: role of objective sleep duration and psychological profiles. Psychosom Med 2011; 73: 88–97.
Butcher JN, Graham JR, Ben-Porah YS, Tellegen A, Dahkstrom WG . Manual for Administration, Scoring and Interpretation, revised edn. University of Minnesota Press: Minneapolis, MN, USA, 2001.
Peppard PE, Young T, Palta M, Dempsey J, Skatrud J . Longitudinal study of moderate weight change and sleep-disordered breathing. JAMA 2000; 284: 3015–3021.
Stunkard AJ, Faith MS, Allison KC . Depression and obesity. Biol Psychiatry 2003; 54: 330–337.
Basta M, Lin HM, Pejovic S, Sarriginnidis A, Bixler EO, Vgontzas AN . Lack of regular exercise, depression, and degree of apnea are predictors of excessive daytime sleepiness in patients with sleep apnea: sex differences. J Clin Sleep Med 2008; 4: 19–25.
Gold PW, Chrousos GP . Organization of the stress system and its dysregulation in melancholic and atypical depression: high vs low CRH/NE states. Mol Psychiatry 2002; 7: 254–275.
Stetler C, Miller GE . Depression and hypothalamic-pituitary-adrenal activation: a quantitative summary of four decades of research. Psychosom Med 2011; 73: 114–126.
Miller AH, Maletic V, Raison CL . Inflammation and its discontents: the role of cytokines in the pathophysiology of major depression. Biol Psychiatry 2009; 65: 732–741.
Valkanova V, Ebmeier KP, Allan CL . CRP, IL-6 and depression: a systematic review and meta-analysis of longitudinal studies. J Affect Disord 2013; 150: 736–744.
Petersen L, Schnohr P, Sørensen TI . Longitudinal study of long-term relation between physical activity and obesity in adults. Int J Obes Relat Metab Disord 2004; 28: 105–112.
Breslau N, Roth T, Rosenthal L, Andreski P . Daytime sleepiness: an epidemiological study of young adults. Am J Public Health 1997; 87: 1649–1653.
Hasler G, Buysse DJ, Gamma A, Ajdacic V, Eich D, Rössler W et al. Excessive daytime sleepiness in young adults: a 20-year prospective community study. J Clin Psychiatry 2005; 66: 521–529.
Jaussent I, Bouyer J, Ancelin ML, Akbaraly T, Pérès K, Ritchie K et al. Insomnia and daytime sleepiness are risk factors for depressive symptoms in the elderly. Sleep 2011; 34: 1103–1110.
Quan SF, Katz R, Olson J, Bonekat W, Enright PL, Young T et al. Factors associated with incidence and persistence of symptoms of disturbed sleep in an elderly cohort: the Cardiovascular Health Study. Am J Med Sci 2005; 329: 163–172.
Vgontzas AN, Bixler EO, Chrousos GP, Pejovic S . Obesity and sleep disturbances: meaningful sub-typing of obesity. Arch Physiol Biochem 2008; 114: 224–236.
Vgontzas AN . Does obesity play a major role in the pathogenesis of sleep apnoea and its associated manifestations via inflammation, visceral adiposity, and insulin resistance? Arch Physiol Biochem 2008; 114: 211–223.
Capuron L, Su S, Miller AH, Bremner JD, Goldberg J, Vogt GJ et al. Depressive symptoms and metabolic syndrome: is inflammation the underlying link? Biol Psychiatry 2008; 64: 896–900.
Daly M . The relationship of C-reactive protein to obesity-related depressive symptoms: a longitudinal study. Obesity (Silver Spring) 2013; 21: 248–250.
Murphy JM, Nierenberg AA, Laird NM, Monson RR, Sobol AM, Leighton AH . Incidence of major depression: prediction from subthreshold categories in the Stirling County Study. J Affect Disord 2002; 68: 251–259.
Eaton WW, Anthony JC, Gallo J . Natural history of Diagnostic Interview Schedule/DSM-IV major depression. The Baltimore Epidemiologic Catchment Area follow-up. Arch Gen Psychiatry 1997; 54: 993–999.
Kessler RC, Berglund P, Demier O . The epidemiology of major depressive disorder: results from the National Comorbidity Survey Replication (NCS-R). JAMA 2003; 289: 3095–3105.
Ford DE, Kamerow DB . Epidemiologic study of sleep disturbances and psychiatric disorders. An opportunity for prevention? JAMA 1989; 262: 1479–1484.
Breslau N, Roth T, Rosenthal L, Andreski P . Sleep disturbance and psychiatric disorders: a longitudinal epidemiological study of young adults. Biol Psychiatry 1996; 39: 411–418.
Ohayon MM . From wakefulness to excessive sleepiness: what we know and still need to know. Sleep Med Rev 2008; 12: 129–141.
Ohayon MM . Determining the level of sleepiness in the American population and its correlates. J Psychiatr Res 2012; 46: 422–427.
Acknowledgements
This work was performed at the Sleep Research and Treatment Center at the Penn State University Milton Hershey Medical Center, and the staff is especially commended for their efforts. This research was funded in part by the American Heart Association (14SDG19830018) and the National Institutes of Health (R01 51931, R01 40916 and R01 64415).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Rights and permissions
About this article
Cite this article
LaGrotte, C., Fernandez-Mendoza, J., Calhoun, S. et al. The relative association of obstructive sleep apnea, obesity and excessive daytime sleepiness with incident depression: a longitudinal, population-based study. Int J Obes 40, 1397–1404 (2016). https://doi.org/10.1038/ijo.2016.87
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/ijo.2016.87
This article is cited by
-
Positive airway pressure therapy for obstructive sleep apnea in patients with Osteogenesis imperfecta: a prospective pilot study
BMC Musculoskeletal Disorders (2021)
-
Current Management of Residual Excessive Daytime Sleepiness Due to Obstructive Sleep Apnea: Insights for Optimizing Patient Outcomes
Neurology and Therapy (2021)
-
The distinct roles of OSA and depression severity in day- and night-time symptomatology in OSA patients: a pilot study
Sleep and Breathing (2020)
-
Excessive daytime sleepiness, metabolic syndrome, and obstructive sleep apnea: two independent large cross-sectional studies and one interventional study
Respiratory Research (2019)
-
Cluster Analysis of Obesity Disease Based on Comorbidities Extracted from Clinical Notes
Journal of Medical Systems (2019)