Abstract
Background and aims:
The small intestinal free fatty acid (FFA) sensors, FFA receptor 1 (FFAR1), FFAR4, G-protein receptor 119 (GPR119) and cluster of differentiation-36 (CD36), mediate the fat-induced release of gastrointestinal (GI) hormones. We investigated whether expression of duodenal FFA sensors in humans was (i) altered by intraduodenal (ID) lipid infusion, (ii) disordered in overweight or obese individuals, (iii) related to lipid-induced GI hormone secretion or (iv) affected by habitual dietary patterns.
Methods:
Endoscopic duodenal biopsies were collected from 20 lean (body mass index (BMI): 22±1 kg m−2), 18 overweight (BMI: 27±1 kg m−2) and 19 obese (BMI: 35±1 kg m−2) participants at baseline, and following a 30 min ID Intralipid infusion (2 kcal min−1); FFA sensor expression was quantified by reverse transcription-PCR. On a separate day, participants underwent ID Intralipid infusion (2 kcal min−1) for 120 min, to assess GI hormone responses. Habitual diet was evaluated using food frequency questionnaires.
Results:
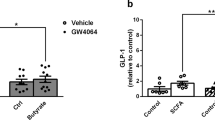
Baseline FFAR1 and FFAR4 expression were lower, and CD36 was higher, in obese participants compared with lean participants. ID lipid increased GPR119 and FFAR1 expression equally across study groups, but did not alter FFAR4 or CD36 expression. Increased FFAR1 expression correlated positively with glucose-dependent insulinotropic polypeptide (GIP) secretion (r=0.3, P<0.05), whereas there was no relationship between habitual diet with the expression of FFA sensors.
Conclusions:
Obesity is associated with altered duodenal expression of FFAR1, FFAR4 and CD36, suggesting altered capacity for the sensing, absorption and metabolism, of dietary lipids. GPR119 and FFAR1 are early transcriptional responders to the presence of ID lipid, whereas FFAR1 may be an important trigger for lipid-induced GIP release in humans.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout




Similar content being viewed by others
References
Feinle C, O'Donovan D, Doran S, Andrews JM, Wishart J, Chapman I et al. Effects of fat digestion on appetite, APD motility, and gut hormones in response to duodenal fat infusion in humans. Am J Gastrointestin Liver Physiol 2003; 284: G798–G807.
Lissner L, Levitsky DA, Strupp BJ, Kalkwarf HJ, Roe DA . Dietary fat and the regulation of energy intake in human subjects. Am J Clin Nutr 1987; 46: 886–892.
Little TJ, Feinle-Bisset C . Oral and gastrointestinal sensing of dietary fat and appetite regulation in humans: modification by diet and obesity. Front Neurosci, 2010; 4: 1782010.
Covasa M . Deficits in gastrointestinal responses controlling food intake and body weight. Am J Physiol Regul Integr Comp Physiol 2010; 299: R1423–R1439.
Stewart JE, Seimon RV, Otto B, Keast RS, Clifton PM, Feinle-Bisset C . Marked differences in gustatory and gastrointestinal sensitivity to oleic acid between lean and obese men. Am J Clin Nutr 2011; 93: 703–711.
Itoh Y, Kawamata Y, Harada M, Kobayashi M, Fujii R, Fukusumi S et al. Free fatty acids regulate insulin secretion from pancreatic beta cells through GPR40. Nature 2003; 422: 173–176.
Hirasawa A, Tsumaya K, Awaji T, Katsuma S, Adachi T, Yamada M et al. Free fatty acids regulate gut incretin glucagon-like peptide-1 secretion through GPR120. Nat Med 2005; 11: 90–94.
Edfalk S, Steneberg P, Edlund H . GPR40 is expressed in enteroendocrine cells and mediates free fatty acid stimulation of incretin secretion. Diabetes 2008; 57: 2280–2287.
Lauffer LM, Iakoubov R, Brubaker PL . GPR119 is essential for oleoylethanolamide-induced glucagon-like peptide-1 secretion from the intestinal enteroendocrine L-cell. Diabetes 2009; 58: 1058–1066.
Cox HM, Tough IR, Woolston AM, Zhang L, Nguyen AD, Sainsbury A et al. Peptide YY is critical for acylethanolamine receptor GPR119-induced activation of gastrointestinal mucosal responses. Cell Metab 2010; 11: 532–542.
Liou AP, Lu X, Sei Y, Zhao X, Pechhold S, Carrero RJ et al. The G-protein-coupled receptor GPR40 directly mediates long-chain fatty acid-induced secretion of cholecystokinin. Gastroenterology 2011; 140: 903–912.
Duca FA, Swartz TD, Sakar Y, Covasa M . Decreased intestinal nutrient response in diet-induced obese rats: role of gut peptides and nutrient receptors. Int J Obes 2013; 37: 375–381.
Little TJ, Isaacs NJ, Young RL, Ott R, Nguyen NQ, Rayner CK et al. Characterization of duodenal expression and localization of fatty acid-sensing receptors in humans: relationships with body mass index. Am J Physiol Gastrointest Liver Physiol 2014; 307: G958–G967.
Cvijanovic N, Isaacs NJ, Rayner CK, Feinle-Bisset C, Young RL, Little TJ . Duodenal fatty acid sensor and transporter expression following acute fat exposure in healthy lean humans. Clin Nutr 2016. e-pub ahead of print 13 February 2016 doi:10.1016/j.clnu.2016.02.005.
Stunkard AJ, Messick S . The three-factor eating questionnaire to measure dietary restraint, disinhibition and hunger. J Psychosom Res 1985; 29: 71–83.
Young RL, Chia B, Isaacs NJ, Ma J, Khoo J, Wu T et al. Disordered control of intestinal sweet taste receptor expression and glucose absorption in type 2 diabetes. Diabetes 2013; 62: 3532–3541.
Nair NS, Brennan IM, Little TJ, Gentilcore D, Hausken T, Jones KL et al. Reproducibility of energy intake, gastric emptying, blood glucose, plasma insulin and cholecystokinin responses in healthy young males. Br J Nutr 2009; 101: 1094–1102.
Santangelo A, Peracchi M, Conte D, Fraquelli M, Porrini M . Physical state of meal affects gastric emptying, cholecystokinin release and satiety. Br J Nutr 1998; 80: 521–527.
Parker BA, Sturm K, MacIntosh CG, Feinle C, Horowitz M, Chapman IM . Relation between food intake and visual analogue scale ratings of appetite and other sensations in healthy older and young subjects. Eur J Clin Nutr 2004; 58: 212–218.
Giles GG, Ireland PD . Dietary Questionnaire for Epidemiological Studies (Version 2). Cancer Council Victoria: Melbourne, VIC, Australia, 1996.
Hodge A, Patterson AJ, Brown WJ, Ireland PD, Giles GG . The Anti Cancer Council of Victoria FFQ: relative validity of nutrient intakes compared with weighed food records in young to middle-aged women in a study of iron supplementation. Aust N Z J Public Health 2000; 24: 576–583.
Schmittgen TD, Livak KJ . Analyzing real-time PCR data by the comparative C(T) method. Nat Protoc 2008; 3: 1101–1108.
Brennan IM, Feltrin KL, Nair NS, Hausken T, Little TJ, Gentilcore D et al. Effects of the phases of the menstrual cycle on gastric emptying, glycemia, plasma GLP-1 and insulin, and energy intake in healthy lean women. Am J Physiol Gastrointest Liver Physiol 2009; 297: G602–G610.
Tanaka T, Katsuma S, Adachi T, Koshimizu TA, Hirasawa A, Tsujimoto G . Free fatty acids induce cholecystokinin secretion through GPR120. Naunyn Schmiedebergs Arch Pharmacol 2008; 377: 523–527.
Ichimura A, Hirasawa A, Poulain-Godefroy O, Bonnefond A, Hara T, Yengo L et al. Dysfunction of lipid sensor GPR120 leads to obesity in both mouse and human. Nature 2012; 483: 350–354.
Zraika S, Dunlop M, Proietto J, Andrikopoulos S . Effects of free fatty acids on insulin secretion in obesity. Obes Rev 2002; 3: 103–112.
Chaput JP, Doucet E, Tremblay A . Obesity: a disease or a biological adaptation? An update. Obesity Rev 2012; 13: 681–691.
Lan H, Hoos LM, Liu L, Tetzloff G, Hu W, Abbondanzo SJ et al. Lack of FFAR1/GPR40 does not protect mice from high-fat diet-induced metabolic disease. Diabetes 2008; 57: 2999–3006.
Kebede M, Alquier T, Latour MG, Semache M, Tremblay C, Poitout V . The fatty acid receptor GPR40 plays a role in insulin secretion in vivo after high-fat feeding. Diabetes 2008; 57: 2432–2437.
Chu ZL, Carroll C, Alfonso J, Gutierrez V, He H, Lucman A et al. A role for intestinal endocrine cell-expressed G protein-coupled receptor 119 in glycemic control by enhancing glucagon-like peptide-1 and glucose-dependent insulinotropic peptide release. Endocrinology 2008; 149: 2038–2047.
Hansen KB, Rosenkilde MM, Knop FK, Wellner N, Diep TA, Rehfeld JF et al. 2-Oleoyl glycerol is a GPR119 agonist and signals GLP-1 release in humans. J Clin Endocrinol Metab 2011; 96: E1409–E1417.
Tran TT, Poirier H, Clement L, Nassir F, Pelsers MM, Petit V et al. Luminal lipid regulates CD36 levels and downstream signaling to stimulate chylomicron synthesis. J Biol Chem 2011; 286: 25201–25210.
Nassir F, Wilson B, Han X, Gross RW, Abumrad NA . CD36 is important for fatty acid and cholesterol uptake by the proximal but not distal intestine. J Biol Chem 2007; 282: 19493–19501.
Raybould HE, Meyer JH, Tabrizi Y, Liddle RA, Tso P . Inhibition of gastric emptying in response to intestinal lipid is dependent on chylomicron formation. Am J Physiol 1998; 274 (Part 2): R1834–R1838.
Buttet M, Poirier H, Traynard V, Gaire K, Tran TT, Sundaresan S et al. Deregulated lipid sensing by intestinal CD36 in diet-induced hyperinsulinemic obese mouse model. PLoS One 2016; 11: e0145626.
Masuda D, Hirano K, Oku H, Sandoval JC, Kawase R, Yuasa-Kawase M et al. Chylomicron remnants are increased in the postprandial state in CD36 deficiency. J Lipid Res 2009; 50: 999–1011.
Young RL, Sutherland K, Pezos N, Brierley SM, Horowitz M, Rayner CK et al. Expression of taste molecules in the upper gastrointestinal tract in humans with and without type 2 diabetes. Gut 2009; 58: 337–346.
Braam LA, Ocke MC, Bueno-de-Mesquita HB, Seidell JC . Determinants of obesity-related underreporting of energy intake. Am J Epidemiol 1998; 147: 1081–1086.
Acknowledgements
We thank the participants who volunteered their time for this study. We also thank the nursing staff of the Gastrointestinal Investigation Unit at the Royal Adelaide Hospital for assisting with endoscopy studies. We would like to acknowledge biostatistician Kylie Lange for statistical support, Scott Standfield for his work analysing CCK samples and Penelope Fitzgerald for her assistance with participant recruitment and infusion studies. TL was supported by a Career Development Fellowship from the National Health and Medical Research Council of Australia (NHMRC; Grant 1022706, 2012–2018), and CF-B by NHMRC Senior Research Fellowships (Grants 627002, 2010-2015, and 1103020, 2016–2020). This study was supported by funding from the Diabetes Australia Research Trust (Grant Y14G-LITT) and the Royal Adelaide Hospital Research Foundation (Grant 1665). CKR, CF-B, RY and TL acknowledge support from the NHMRC Centre of Research Excellence in Translating Nutritional Science to Good Health (Grant 1041687, 2013–17).
Clinical trial registry: This study was prospectively registered with the Australia and New Zealand Clinical Trial Registry (www.anzctr.org.au trial number: ACTRN12612000376842).
Author contributions
TJL conception and design of research; NC, NJI and CKR performed experiments; NC analysed data; NC, TJL, RY and CF-B interpreted results of experiments; NC drafted manuscript and prepared figures; NC, RY, TJL and CF-B edited and revised manuscript. All authors had access to the study data and reviewed and approved the final manuscript.
Disclaimer
A small subset of data from the lean group has been published previously in Clinical Nutrition (doi:10.1016/j.clnu.2016.02.005; Epub ahead of print).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Additional information
Supplementary Information accompanies this paper on International Journal of Obesity website
Supplementary information
Rights and permissions
About this article
Cite this article
Cvijanovic, N., Isaacs, N., Rayner, C. et al. Lipid stimulation of fatty acid sensors in the human duodenum: relationship with gastrointestinal hormones, BMI and diet. Int J Obes 41, 233–239 (2017). https://doi.org/10.1038/ijo.2016.199
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/ijo.2016.199
This article is cited by
-
The effect of bariatric surgery on the expression of gastrointestinal taste receptors: A systematic review
Reviews in Endocrine and Metabolic Disorders (2024)
-
Free fatty acids and peripheral blood mononuclear cells (PBMC) are correlated with chronic inflammation in obesity
Lipids in Health and Disease (2023)
-
Targeting the GPR119/incretin axis: a promising new therapy for metabolic-associated fatty liver disease
Cellular & Molecular Biology Letters (2021)
-
Obesity alters fatty acid sensing
Nature Reviews Endocrinology (2017)