Abstract
Colorectal cancer (CRC) is a common malignancy worldwide, and chronic inflammation is a risk factor for CRC. In this study, we carried out a cohort study among the Japanese atomic bomb (A-bomb) survivor population to investigate any association between immune- and inflammation-related gene polymorphisms and CRC. We examined the effects of six single-nucleotide polymorphisms of CD14 and IL18 on relative risks (RRs) of CRC. Results showed that RRs of CRC, overall and by anatomic subsite, significantly increased with increasing radiation dose. The CD14–911A/A genotype showed statistically significant higher risks for all CRC and distal CRC compared with the other two genotypes. In addition, the IL18–137 G/G genotype showed statistically significant higher risks for proximal colon cancer compared with the other two genotypes. In phenotype–genotype analyses, the CD14–911A/A genotype presented significantly higher levels of membrane and soluble CD14 compared with the other two genotypes, and the IL18–137 G/G genotype tended to be lower levels of plasma interleukin (IL)-18 compared with the other two genotypes. These results suggest the potential involvement of a CD14-mediated inflammatory response in the development of distal CRC and an IL18-mediated inflammatory response in the development of proximal colon cancer among A-bomb survivors.
Similar content being viewed by others
Introduction
It has been reported that colorectal cancer (CRC) at particular anatomic subsites may be associated with distinct risk factors.1–3 The molecular mechanisms of CRC development also differ among anatomic sites: proximal colon cancer is usually related to the nucleotide instability pathway, such as microsatellite instability;4,5 distal colon and rectal cancer are usually associated with specific chromosomal instability6–9 and it is possible that CRC may also have different levels of association with radiation by subsite. Therefore, we studied separately the two CRC subsites for proximal colon cancer and distal CRC: cancers located in the cecum, ascending colon and transverse colon were categorized as proximal colon cancer, whereas cancers located in the descending colon, sigmoid colon, rectosigmoid junction and rectum were categorized as distal CRC. Previous epidemiological studies conducted by the Radiation Effects Research Foundation (RERF) indicated an increase in incidence and mortality of CRC among atomic bomb (A-bomb) survivors,10,11 but the mechanisms underlying susceptibility to radiation effects at different anatomic subsites of CRC have remained unclear.
Chronic inflammation is a critical risk factor for the development of CRC.12 RERF immunological studies have found an accelerated persistent dose-dependent inflammation among A-bomb survivors,13,14 which may provide a key to understanding anatomic subsite differences in susceptibility. Owing to its known biological role in the innate immune response to pathogens, CD14 was an obvious candidate. Lipopolysaccharide or endotoxin, the main component of the outer membrane of Gram-negative bacteria, has been related to accelerated growth of human colorectal carcinoma cells.15 The cellular response to lipopolysaccharide is mainly regulated by expression of CD14, and the binding between lipopolysaccharide and CD14 activates macrophages and colorectal epithelial cells to produce cytokines such as tumor necrosis factor- α (TNF-α) and interleukin (IL)-1, IL-6 and IL-18.16–19 It has been reported that these cytokines may be related to the enhancement of inflammatory response in the colorectum.15,20 The CD14 gene is located on chromosome 5q31.1 and single-nucleotide polymorphisms (SNPs) were recently identified in the 5′-untranslated region of CD14, which regulates CD14 gene expression levels, thereby affecting susceptibility to inflammatory diseases such as atopic dermatitis, Crohn’s disease, asthma and CRC.21–26 CD14 exists in two forms, membrane CD14 (mCD14) and soluble CD14 (sCD14). The mCD14 found mainly on the surface of monocytes and macrophages is the principal membranous receptor for lipopolysaccharide bindings16 and sCD14 is present in the plasma, being released owing to shedding from monocytes.27
IL-18 is a pro-inflammatory cytokine that has a crucial role in immune and inflammatory reactions. The human IL-18 gene, IL18, is located on chromosome 11q22.2–22,328 and SNPs located in the promoter position of the IL18 gene that regulates IL18 gene expression levels are associated with various inflammatory diseases20,29–32 and CRC.33
CRC is considered a multifactorial disease, the onset of which is attributed to complex interactions between environmental and genetic factors. It was difficult to obtain cancer and normal tissues from all cohort subjects; thus, we could not precisely determine microsatellite instability or chromosomal instability status. Considering the points mentioned above, the aim of the present study was to examine a possible association between immune- and inflammation-related gene polymorphisms and CRC development, as well as the effects in relation to radiation. We identified six SNPs in the 5′-untranslated regions of two genes, CD14 and IL18, and here we report the risks of proximal colon cancer and distal CRC for immune/inflammation-related CD14 and IL18 gene polymorphisms, as well as the effects of those polymorphisms on the radiation dose response for the two CRC anatomic subsites.
Materials and Methods
Study population
The RERF and its predecessor, the Atomic Bomb Casualty Commission, have conducted and continue to conduct a cohort study, the Adult Health Study, of ~20,000 A-bomb survivors, to determine the late health effects of A-bomb radiation exposure. The Immunology Study began in the Adult Health Study cohort in December 1981 with the aim of investigating radiation effects on the immune systems of A-bomb survivors. During the period 1981–2005, we obtained blood samples from 7,131 Adult Health Study participants who visited the clinic for examinations. After excluding subjects who had a history of first primary cancer at the time of blood collection, whose radiation dose could not be estimated, who were exposed in utero (organ doses not estimable), who were older than 80 years of age at the time of blood collection, or who chose not to provide informed consent (84 subjects), a total of 4,690 subjects (3,175 who provided informed consent and 1,515 who died after blood collection but were approved for this study by the RERF Ethical Committee) remained. They constitute the Immunogenome (IMG) cohort to assess association between cancer development and gene polymorphisms among A-bomb survivors, focusing on immune/inflammation-related genes. In addition, for the present study, 13 cases, whose CRC occurred more than 1 year after another primary cancer, and 4 cases, whose cancer was found in both sites (proximal colon and distal colorectal sites) at the same time, were excluded, leaving 4,673 subjects for the final analysis.
Incident cancer cases were identified through the Hiroshima Tumor and Tissue Registries and the Nagasaki Cancer Registry. Baseline for follow-up was defined as the date of the first blood sample for the IMG study (collection began in December 1981 and continued through August 2001). The end of follow-up was 31 December 2005, the latest date of complete cancer ascertainment at the time the data analysis was initiated. This study was approved by the Human Investigation Committee and by the Ethics Committee for Genome Research at RERF.
Genotyping
SNP genotyping was performed as previously described in detail.34 Briefly, genomic DNA was extracted from peripheral blood cells using proteinase K digestion and a QIAmp DNA Mini Kit (Qiagen, Hilden, Germany), and subsequently subjected to whole genome amplification (GenomiPhi DNA Amplification Kit, GE Healthcare, Little Chalfont, Buckinghamshire, UK). The Celera Genomic and NCBI databases including Asian populations35,36 were used to screen 6 CD14 SNPs and 10 IL18 SNPs in the CD14 and IL18 gene regions, respectively. After determining allele frequency, we selected three CD14 SNPs CD14–1247 C/T (CD14-1, rs2569191), −911A/C (CD14-2, rs5744454) and −260A/G (CD14-3, rs2569190), and three IL18 SNPs IL18–656A/C (IL18-1, rs1946519), −607T/G (IL18-2, rs1946518) and −137 G/C (IL18-3, rs187238). All of these were localized in the 5′-untranlated region and showed variant allele frequencies >5% in our study population. We found 100% linkage disequilibrium (LD) between CD14-1 and CD14-3 SNPs and between IL18-1 and IL18-2 SNPs. Frequency distributions of CD14 and IL18 genotypes according to CRC and each subsite are shown in Table 1. Primers and probes for these SNPs were designed using Primer Express software, version 2.1 (Applied Biosystems, Foster City, CA). The TaqMan-Allelic Discrimination method was used for the detection of SNPs and all of the assays were conducted in 384-well PCR plates. The principle of TaqMan Real-Time PCR assay system using fluorogenic probes and the 5′-nuclease is explained by Livak.37 Amplification reactions (5 μl) were carried out in duplicate with 10 ng of template DNA, 1×TaqMan Universal Master Mix buffer (Applied Biosystems), 300 nM of each primer and 200 nM of each fluorogenic probe. Thermal cycling was initiated with 2 min incubation at 50 °C, followed by a first denaturation step of 10 min at 95 °C and then by 40 cycles of 15 s at 95 °C and 1 min at 60 °C. After PCR was completed, plates were brought to room temperature and read in an ABI PRISM 7900 Sequence Detection System (Applied Biosystems). Results were analyzed using Allelic Discrimination software (SNPAlyze, Dynacom, Yokohama, Japan).
Measurement of monocyte cell surface mCD14 levels
Blood samples were lysed with EasyLyse (DakoCytomation, code-Nr.S2364, Glostrup, Denmark) and subsequently stained with fluorescein isothiocyanate-labeled CD14 monoclonal antibody (Invitrogen, MHCD1401, Carlsbad, CA, USA) in the wells of a flexible 96-well U-bottom plate (BD Biosciences, San Jose, CA, USA) at 37 °C for 20 min. The cells were washed with phosphate-buffered saline containing 1% fetal calf serum and then analyzed using a CyAn ADP analyzer (Beckman Coulter, Indianapolis, IN, USA). Results were expressed as the mean of fluorescence intensity. Four hundred and one subjects who did not have cancer and who were non-exposed (radiation dose <0.005 Gy) were randomly selected from the IMG cohort members with the aim of excluding the effects of cancer and radiation on the relationship between CD14 genotype and mCD14 levels. The mCD14 levels were considered as the dependent variables to be analyzed after taking the logarithm at the base 10. This logarithmic transformation was applied to ensure the normality of the error distribution.
Measurement of plasma sCD14 and IL-18 levels
Plasma sCD14 levels were measured by the enzyme-linked immunosorbent assay method using a Quatikine Human sCD14 Immunoassay Kit (R&D Systems, Minneapolis, MN) according to the manufacturers’ instructions. The concentration of plasma sCD14 was calibrated from a dose–response curve based on the reference standards. The minimum detectable concentration of sCD14 was 125 pg/ml. Four hundred and one cancer-free, non-exposed subjects (same subjects as those used for mCD14 levels measurement) were selected from the IMG cohort to assess the relationship between CD14 genotype and plasma sCD14 levels, excluding the effects of cancer and radiation.
Plasma IL-18 levels were measured using a Human IL-18 ELISA Kit (Medical & Biological Laboratories, Nagoya, Japan) as per the manufacturers’ instructions. The concentration of human IL-18 was calibrated from a dose–response curve based on the reference standards. The minimum detectable concentration of IL-18 was 12.5 pg/ml. Four hundred and one cancer-free, non-exposed subjects (same subjects as those used for mCD14 levels measurement) were selected from the IMG cohort to assess the relationship between IL-18 genotype and plasma IL-18 levels, excluding the effects of cancer and radiation. Plasma sCD14 and IL-18 levels were also considered as the dependent variables to be analyzed after taking the logarithm at the base 10.
Risk analysis
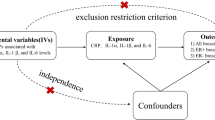
Rate ratios or excess rate ratios for CRC incidence were estimated using standard event-time analysis, with attained age as the primary baseline time scale. All statistical models included adjustment for city (Hiroshima or Nagasaki), gender, calendar year and smoking intensity (in units of 20 cigarettes per day) in a log-linear model analogous to the Cox proportional hazards regression model (apart from the effect of radiation; see below). Information on smoking was obtained by interview at the time of blood collection. A-bomb radiation dose in weighted Gray was estimated using the DS02 dosimetry system,38 based on weighted colon dose computed as the γ-dose plus 10 times the neutron dose. The model used for estimating the effects of risk factors without genomic factors on the CRC incidence was , where λ represents rate (cancer incidence), a is attained age, c is city indicator (0 for Hiroshima, 1 for Nagasaki), g is gender indicator (0 for males, 1 for females), cg is the interaction between city and gender, t is calendar time (beginning in 1981), t>7.5 is a linear spline with value (t–7.5) after 1 July 1987 and 0 before 1 July 1987, sc is current smoking intensity (in units of 20 cigarettes per day), sp is past smoking intensity among persons who had quit smoking (also in units of 20 cigarettes per day) and d is radiation dose to the colon in weighted Gray. The join point 7.5 in the calendar year spline was selected as providing the best fit over a grid of 6 month calendar-time values, between 1985 and 1989, to show the effect of screening introduced in the mid-1980s.
Genetic effects were estimated and tested as log relative risk (RR) in the log-linear part of the above model (with adjustment for city, gender, calendar year, smoking and radiation dose). For each SNP, a two-degree-of-freedom model was fit based on indicators h1 and h2 for two of the three possible genotypes (major homozygotes, heterozygotes and minor homozygotes) at each locus. The reference group was the homozygous group with lower RR; usually the minor variant homozygous genotype had the lower RR. For IL18-3 SNPs where there was only one or no cancer case with minor homozygous genotype, major homozygote was used as a reference group. We also considered one degree of freedom recessive or dominant models; the primary model of interest was the recessive model for the homozygotes of the allele, demonstrating positive risk, and an alternative model was the dominant model (heterozygotes and homozygotes) for the positive-risk allele. However, for IL18 SNPs few numbers of cases sometimes required that a different reference group be used; see Tables 2A, 2B, 2C for definitions of the models fit. We estimated both genomic main effect and interaction between genotype and radiation for each SNP. Statistical interaction between radiation and genotypes was tested by including in the model a log-linear effect modifier of the excess RR: where h1 and h2 are the heterozygote and non-reference homozygote genotype, respectively, eőj (j=1,2) is the main effect (RR) of genotype and eγ is the multiplicative interaction between genotype and radiation.
Analyses of protein levels were based on analysis of variance applied to log transformed (base 10) values using IBM SPSS Statistics (Version 21, Chicago, IL, USA). Risk analyses based on the excess RR model were performed using Epicure software (HiroSoft International Corp., Seattle, WA). Unless specified otherwise, confidence bounds are 95% based on statistical likelihood. Although 95% confidence corresponds to a statistical significance at the 5% level, because of multiple testing with correlated outcomes (due to LD), it is not possible to specify a clear cutoff level for traditional statistical significance with the multiple SNP tests. We tested the following three outcomes: all colorectal, proximal colon and distal colon/rectal. We tested five marker sets (CD14-1, CD14-2, CD14-3, IL18-1/2 and IL18-3), but the first three and the latter two sets were not in compete equilibrium. A strict Bonferroni correction would be based on assuming that 15 independent statistical tests were performed, leading to a significance level of 0.05/15=0.0033; this is a conservative level, leading to possible false negative results. As there are two independent sites and two strictly independent marker sets, we considered P⩽0.05/4=0.0125 to be statistically significant and P⩽0.1/4=0.025 (but>0.0125) to be suggestive or marginally significant for the SNP tests and for interactions between SNPs and radiation dose. The usual 0.05 level was considered statistically significant for radiation dose.
Results
Characteristics of subjects
Characteristics of cases only and all cohort subjects are shown in Table 3. Compared with the full cohort (i.e., population-based baseline characteristics, including subsequent cases of CRC), the cases included higher proportions of males, smokers and persons with radiation doses above the median.
Effects of covariates on CRC risk without genomic factors
Women showed significantly lower incidence of all CRC combined, proximal colon cancer and distal CRC compared with men (RR: 0.43 (95% confidence interval (CI): (0.31, 0.61), 0.49 (0.28, 0.89) and 0.36 (0.23, 0.56), respectively). There were no significant differences in incidence of all CRC combined or subsite according to city or smoking.
Excess relative risk (ERR) for radiation at 1 Gy (with adjustment for city, gender, calendar year and smoking, but not for CD14 or IL-18 genotypes) was: 0.55 (95% CI (0.21, 1.02)) for all CRC combined, 0.53 (95% CI (0.02, 1.38)) for proximal colon cancer and 0.53 (95% CI (0.12, 1.15)) for distal CRC. After adjustment for each individual genotype, the ERRs for radiation at 1 Gy were essentially unchanged (Tables 2A, 2B, 2C).
Effects of CD14 genotype and radiation dose on the risks of CRC and each subsite
CD14-1 was in almost complete LD (r2=0.997) with CD14-3. CD14-2 was not in LD with CD14-1 and CD14-2 (r2=0.386 and 0.385), respectively. Despite the high LD between CD14-1 and CD14-3, results were slightly different numerically; hence, we show results for these two SNPs separately. Association between risks of all combined CRC and each subsite, genotypes and radiation dose were examined using three CD14 SNPs. For all three SNPs, subjects with major homozygous genotype, compared with heterozygotes and minor homozygotes combined, showed significantly higher RRs for all CRC combined and distal CRC, but not for proximal colon cancer (Tables 2A, 2B, 2C). There were no statistically significant interactions between CD14 genotypes and radiation dose (Tables 2A, 2B, 2C).
Effects of IL18 genotype and radiation dose on the risk of CRC and each subsite
IL18-1 was strongly linked (r2=0.999) with IL18-2. IL18-3 was not in high LD (r2=0.101) with IL18-1/2. Results for IL18-1 an IL18-2 were virtually identical numerically, so we present them as a single result. We focused on IL18-3 SNP to examine the association between the RRs of CRC and each subsite, IL18 genotypes and radiation dose(IL18-1/2 SNPs were not significantly related to risks of CRC; Table 2A). Subjects with minor homozygous genotype, compared with heterozygotes and major homozygotes combined, showed significantly lower RRs for all CRC combined (Table 2A, alternative model); in addition, those with major homozygous genotype, compared with heterozygotes and minor homozygotes combined, showed significantly higher RRs for proximal colon cancer (Table 2B, primary model), but not for distal CRC (Table 2C). There were no statistically significant interactions between IL18 genotypes and radiation dose (Tables 2A, 2B, 2C).
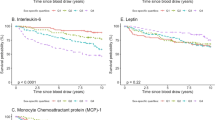
Alteration of mCD14, sCD14 and plasma IL-18 levels by genotypes in non-exposed cancer-free subjects
Levels of mCD14 were compared between the two genotype groups (major homozygotes versus minor homozygotes and heterozygotes combined) for each CD14 SNP, as shown in Figure 1a. There was a significant difference between the two groups with CD14-2 SNP (P<0.001).
Plasma levels of sCD14 were higher with major CD14 homozygotes, compared with the other two genotypes together (Figure 1b).
Levels of plasma IL-18 were compared between the two genotype groups for each IL18 SNP. Comparison of minor homozygotes with major homozygotes and heterozygotes combined for IL18-1 and IL18-2 revealed no significant difference, whereas comparison of major homozygotes with minor homozygotes and heterozygotes combined for IL18-3, although not statistically significant, suggested that minor homozygotes and heterozygotes combined expressed higher levels of plasma IL-18 than major homozygotes did (Figure 1c).
Discussion
We studied the association between gene polymorphisms in the immune/inflammation-related CD14 and IL18 gene region and risk of all CRC, as well as CRC at anatomic subsites, among A-bomb survivors, in a cohort study. Differences were found depending on anatomic subsite of CRC: the CD14-911A/C polymorphism was significantly related to risk of distal CRC, whereas the IL18–137 G/C polymorphism was significantly related to risk of proximal colon cancer.
As these SNPs are located in 5′-untranslated regions, including the promoter regions, we investigated the functional significance of gene polymorphisms in relation to levels of monocyte mCD14 and plasma sCD14, as well as IL-18, among non-exposed cancer-free subjects. In the main genotype effects analysis, the CD14–911A/C polymorphism major homozygotes appeared to be sensitive to all CRC combined and distal CRC. Moreover, in the phenotype–genotype analysis, major homozygotes expressed higher CD14 protein levels with the three targeted CD14 SNPs. Our results are consistent with a previous report in which CD14 gene expression was found in the colon, especially in the distal colon.39 On the other hand, the IL18–137 G/C polymorphism minor variant appeared to be resistant to proximal colon cancer, whether as heterozygote or minor homozygote, although there was only one minor homozygous case; and major homozygotes expressed lower IL-18 protein levels with three targeted IL18 SNPs. Moreover, the targeted IL18 SNPs showed no evidence of any association with distal CRC. It has been reported that production of IL-18 in the colon may have a part in host anti-tumor immune response,40,41 which is consistent with our results. IL-18 is known to be an inducing factor of interferon-γ that activates natural killer cells, T lymphocytes and macrophages, and it results in better prognosis for patients with CRC.40,42,43 Microsatellite instability CRCs are associated with lymphocytes and could also contribute to good prognosis.44–46
As noted above, development of proximal colon cancer and distal CRC have different mechanisms. In this study of A-bomb survivors, we found a potential involvement of CD14-mediated inflammatory response in the development of distal CRC and IL18-mediated inflammatory response in the development of proximal colon cancer. However, the mechanism that mediates these remains to be elucidated.
We previously observed that IL10 gene polymorphisms were involved in individual differences in radiation-related diffuse-type gastric cancer risk among A-bomb survivors.34 Although we also examined the association between CRC risk and radiation dose by genotype of IL10 among A-bomb survivors in this study, no significant relationship between radiation exposure, IL10 polymorphisms and CRC was observed.
Our data do not suggest a major difference in radiation risk according to anatomic subsite, contrary to previous findings in the RERF Life Span Study (LSS) of a radiation effect for colon cancer but not for rectal cancer (ERR for colon cancer 0.54 with 90% CI (0.30, 0.81), ERR for rectal cancer 0.19 with 90% CI (−0.04, 0.47)).10 To assess whether this variation was due to inability to detect a radiation effect on rectal cancer in previous LSS analyses, the analogous two ERRs were calculated for the IMG cohort as well. ERR for all colon (proximal and distal combined, as well as unspecified) was 0.47 (95% CI (0.10, 1.02), P=0.008) based on 160 cases of proximal or distal colon cancer and that for rectal cancer was 0.61 (95% CI (0.02, 1.69), P=0.041; based on 53 cases). As the ratio of numbers of colon to rectal cases in the IMG cohort (3.21) is larger than that in the LSS analysis (1.81), the significant radiation effect with rectal cancer in the IMG cohort is not due to an overabundance of rectal cancer cases, nor is the lack of significant radiation effect with rectal cancer in the LSS due to a paucity of cases. The relatively smaller number of rectal cancers in the IMG cohort is consistent with a result of the LSS cancer incidence analysis (temporal trends), which shows that the incidence of colon cancer increased more rapidly than that of rectal cancer in the more recent period of LSS follow-up, when the IMG cohort follow-up was conducted. Fifteen (out of a total of 53) rectal cancer cases in the IMG cohort were diagnosed after the end of the LSS analysis (between 1 January 1999 and 31 December 2005). With only three of these added cases having radiation doses over 2,000 mGy, the numbers are too small to reach any firm conclusion about new evidence of radiation risk for rectal cancer; this area requires further scrutiny in future analyses within the LSS cohort. None of the targeted CD14 and IL18 SNPs showed any evidence of interaction with radiation.
The advantages of our study are as follows: long-term follow-up, detailed dosimetry reconstruction and a well-defined radiation-exposed population. One limitation is the small number of subjects, in particular cases of CRC, owing to the size of the original cohort and exclusion criteria. However, lack of statistical significance does not necessarily imply lack of meaningful biological interaction.47 In the future, it will be possible to increase the statistical power by addition of cases, although LSS analyses suggest that radiation risk declines with age; thus,the magnitude of radiation effect on CRC—in particular any possible interaction between genes and radiation—may be diminished in future cases. As described above, onset of CRC is attributed to complex interactions between environmental and genetic factors. Factors that are found to be important in the development of CRC include the following: diet, alcohol consumption, body mass index and physical activity. Future studies will consider the effects of these lifestyle factors on radiation-related CRC.
In conclusion, we found strong associations between CRC and immune/inflammation-related gene polymorphisms in the CD14 and IL18 genes. Genetic factors related to immune/inflammation are involved in individual susceptibility to CRC. Further investigation into CRC and radiation exposure is planned based on consideration of microsatellite (chromosome) instability status. CD14 and IL18 genes may contribute to a predisposition to CRC; thus, screening for CD14–911A/C and IL18–137 G/C genotypes is likely to be a useful tool for RR assessment with CRC among A-bomb survivors.
References
Inoue M, Tajima K, Hirose K, Hamajima N, Takezaki T, Hirai T et al. Subsite-specific risk factors for colorectal cancer: a hospital-based case-control study in Japan. Cancer Causes Control 1995; 6: 14–22.
Peters U, Sinha R, Chatterjee N, Subar AF, Ziegler RG, Kulldorff M et al. Dietary fibre and colorectal adenoma in a colorectal cancer early detection programme. Lancet 2003; 361: 1491–1495.
Hjartaker A, Aagnes B, Robsahm TE, Langseth H, Bray F, Larsen IK . Subsite-specific dietary risk factors for colorectal cancer: a review of cohort studies. J Oncol 2013; 2013: 703854.
Miyakura Y, Sugano K, Konishi F, Ichikawa A, Maekawa M, Shitoh K et al. Extensive methylation of hMLH1 promoter region predominates in proximal colon cancer with microsatellite instability. Gastroenterology 2001; 121: 1300–1309.
Thibodeau SN, Bren G, Schaid D . Microsatellite instability in cancer of the proximal colon. Science 1993; 260: 816–819.
Fernebro E, Halvarsson B, Baldetorp B, Nilbert M . Predominance of CIN versus MSI in the development of rectal cancer at young age. BMC Cancer 2002; 2: 25.
Frattini M, Balestra D, Suardi S, Oggionni M, Alberici P, Radice P et al. Different genetic features associated with colon and rectal carcinogenesis. Clin Cancer Res 2004; 10: 4015–4021.
Nilbert M, Planck M, Fernebro E, Borg A, Johnson A . Microsatellite instability is rare in rectal carcinomas and signifies hereditary cancer. Eur J Cancer 1999; 35: 942–945.
Delattre O, Olschwang S, Law DJ, Melot T, Remvikos Y, Salmon RJ et al. Multiple genetic alterations in distal and proximal colorectal cancer. Lancet 1989; 2: 353–356.
Preston DL, Ron E, Tokuoka S, Funamoto S, Nishi N, Soda M et al. Solid cancer incidence in atomic bomb survivors: 1958-1998. Radiat Res 2007; 168: 1–64.
Ozasa K, Shimizu Y, Suyama A, Kasagi F, Soda M, Grant EJ et al. Studies of the mortality of atomic bomb survivors, Report 14, 1950-2003: an overview of cancer and noncancer diseases. Radiat Res 2012; 177: 229–243.
Itzkowitz SH, Yio X . Inflammation and cancer IV. Colorectal cancer in inflammatory bowel disease: the role of inflammation. Am J Physiol Gastrointest Liver Physiol 2004; 287: G7–G17.
Kusunoki Y, Hayashi T . Long-lasting alterations of the immune system by ionizing radiation exposure: implications for disease development among atomic bomb survivors. Int J Radiat Biol 2008; 84: 1–14.
Hayashi T, Morishita Y, Khattree R, Misumi M, Sasaki K, Hayashi I et al. Evaluation of systemic markers of inflammation in atomic-bomb survivors with special reference to radiation and age effects. FASEB J 2012; 26: 4765–4773.
Kojima M, Morisaki T, Izuhara K, Uchiyama A, Matsunari Y, Katano M et al. Lipopolysaccharide increases cyclo-oxygenase-2 expression in a colon carcinoma cell line through nuclear factor-kappa B activation. Oncogene 2000; 19: 1225–1231.
Wright SD, Ramos RA, Tobias PS, Ulevitch RJ, Mathison JC . CD14, a receptor for complexes of lipopolysaccharide (LPS) and LPS binding protein. Science 1990; 249: 1431–1433.
Ulevitch RJ, Tobias PS . Recognition of gram-negative bacteria and endotoxin by the innate immune system. Curr Opin Immunol 1999; 11: 19–22.
Dinarello CA . Interleukin-18. Methods 1999; 19: 121–132.
Manigold T, Bocker U, Traber P, Dong-Si T, Kurimoto M, Hanck C et al. Lipopolysaccharide/endotoxin induces IL-18 via CD14 in human peripheral blood mononuclear cells in vitro. Cytokine 2000; 12: 1788–1792.
Tamura K, Fukuda Y, Sashio H, Takeda N, Bamba H, Kosaka T et al. IL18 polymorphism is associated with an increased risk of Crohn's disease. J Gastroenterol 2002; 37: 111–116.
Munthe-Kaas MC, Torjussen TM, Gervin K, Lodrup Carlsen KC, Carlsen KH, Granum B et al. CD14 polymorphisms and serum CD14 levels through childhood: a role for gene methylation? J Allergy Clin Immunol 2010; 125: 1361–1368.
Litonjua AA, Belanger K, Celedon JC, Milton DK, Bracken MB, Kraft P et al. Polymorphisms in the 5' region of the CD14 gene are associated with eczema in young children. J Allergy Clin Immunol 2005; 115: 1056–1062.
Klein W, Tromm A, Griga T, Fricke H, Folwaczny C, Hocke M et al. A polymorphism in the CD14 gene is associated with Crohn disease. Scand J Gastroenterol 2002; 37: 189–191.
Yazdani N, Amoli MM, Naraghi M, Mersaghian A, Firouzi F, Sayyahpour F et al. Association between the functional polymorphism C-159T in the CD14 promoter gene and nasal polyposis: potential role in asthma. J Investig Allergol Clin Immunol 2012; 22: 406–411.
Guo Q, Zhu J, Xia B . Polymorphism of CD14 gene but not the mutation of TLR4 gene is associated with colorectal cancer in Chinese patients. J Gastroenterol Hepatol 2006; 21: 92–97.
Chen R, Luo FK, Wang YL, Tang JL, Liu YS . LBP and CD14 polymorphisms correlate with increased colorectal carcinoma risk in Han Chinese. World J Gastroenterol 2011; 17: 2326–2331.
Schutt C . Cd14. Int J Biochem Cell Biol 1999; 31: 545–549.
Nolan KF, Greaves DR, Waldmann H . The human interleukin 18 gene IL18 maps to 11q22.2-q22.3, closely linked to the DRD2 gene locus and distinct from mapped IDDM loci. Genomics 1998; 51: 161–163.
Tavares NA, Santos MM, Moura R, Araujo J, Guimaraes R, Crovella S et al. Interleukin 18 (IL18) gene promoter polymorphisms are associated with type 1 diabetes mellitus in Brazilian patients. Cytokine 2013; 62: 286–289.
Imboden M, Nicod L, Nieters A, Glaus E, Matyas G, Bircher AJ et al. The common G-allele of interleukin-18 single-nucleotide polymorphism is a genetic risk factor for atopic asthma. The SAPALDIA Cohort Study. Clin Exp Allergy 2006; 36: 211–218.
Tiret L, Godefroy T, Lubos E, Nicaud V, Tregouet DA, Barbaux S et al. Genetic analysis of the interleukin-18 system highlights the role of the interleukin-18 gene in cardiovascular disease. Circulation 2005; 112: 643–650.
Giedraitis V, He B, Huang WX, Hillert J . Cloning and mutation analysis of the human IL-18 promoter: a possible role of polymorphisms in expression regulation. J Neuroimmunol 2001; 112: 146–152.
Nikiteas N, Yannopoulos A, Chatzitheofylaktou A, Tsigris C . Heterozygosity for interleukin-18 −607A/C polymorphism is associated with risk for colorectal cancer. Anticancer Res 2007; 27: 3849–3853.
Hayashi T, Ito R, Cologne J, Maki M, Morishita Y, Nagamura H et al. Effects of IL-10 haplotype and atomic bomb radiation exposure on gastric cancer risk. Radiat Res 2013; 180: 60–69.
De La Vega FM, Dailey D, Ziegle J, Williams J, Madden D, Gilbert DA . New generation pharmacogenomic tools: a SNP linkage disequilibrium Map, validated SNP assay resource, and high-throughput instrumentation system for large-scale genetic studies. Biotechniques 2002; 52(Suppl: 48-50): 54.
Venter JC, Adams MD, Myers EW, Li PW, Mural RJ, Sutton GG et al. The sequence of the human genome. Science 2001; 291: 1304–1351.
Livak KJ . Allelic discrimination using fluorogenic probes and the 5' nuclease assay. Genet Anal 1999; 14: 143–149.
Cullings HM, Fujita S, Funamoto S, Grant EJ, Kerr GD, Preston DL . Dose estimation for atomic bomb survivor studies: its evolution and present status. Radiat Res 2006; 166: 219–254.
Ortega-Cava CF, Ishihara S, Rumi MA, Kawashima K, Ishimura N, Kazumori H et al. Strategic compartmentalization of Toll-like receptor 4 in the mouse gut. J Immunol 2003; 170: 3977–3985.
Pages F, Berger A, Henglein B, Piqueras B, Danel C, Zinzindohoue F et al. Modulation of interleukin-18 expression in human colon carcinoma: consequences for tumor immune surveillance. Int J Cancer 1999; 84: 326–330.
Zaki MH, Vogel P, Body-Malapel M, Lamkanfi M, Kanneganti TD . IL-18 production downstream of the Nlrp3 inflammasome confers protection against colorectal tumor formation. J Immunol 2010; 185: 4912–4920.
Matsushita K, Takenouchi T, Kobayashi S, Hayashi H, Okuyama K, Ochiai T et al. HLA-DR antigen expression in colorectal carcinomas: influence of expression by IFN-gamma in situ and its association with tumour progression. Br J Cancer 1996; 73: 644–648.
Billiau A . Interferon-gamma: biology and role in pathogenesis. Adv Immunol 1996; 62: 61–130.
Dolcetti R, Viel A, Doglioni C, Russo A, Guidoboni M, Capozzi E et al. High prevalence of activated intraepithelial cytotoxic T lymphocytes and increased neoplastic cell apoptosis in colorectal carcinomas with microsatellite instability. Am J Pathol 1999; 154: 1805–1813.
Phillips SM, Banerjea A, Feakins R, Li SR, Bustin SA, Dorudi S . Tumour-infiltrating lymphocytes in colorectal cancer with microsatellite instability are activated and cytotoxic. Br J Surg 2004; 91: 469–475.
Boissiere-Michot F, Lazennec G, Frugier H, Jarlier M, Roca L, Duffour J et al. Characterization of an adaptive immune response in microsatellite-instable colorectal cancer. Oncoimmunology 2014; 3: e29256.
Hutter CM, Mechanic LE, Chatterjee N, Kraft P, Gillanders EM . Gene-environment interactions in cancer epidemiology: a National Cancer Institute Think Tank report. Genet Epidemiol 2013; 37: 643–657.
Acknowledgements
The RERF, Hiroshima and Nagasaki, Japan is a public interest foundation funded by the Japanese Ministry of Health, Labour and Welfare (MHLW), and the US Department of Energy (DOE). This publication is supported by RERF Research Protocols RPs 4-04 and 5-04, and supported in part by the Grant-in-Aid for Scientific Research (B) from the Ministry of Education, Culture, Sports, Science and Technology of Japan (24390162 and 15H04791). The views of the authors do not necessarily reflect those of the two governments.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Rights and permissions
This work is licensed under a Creative Commons Attribution-NonCommercial-ShareAlike 4.0 International License. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in the credit line; if the material is not included under the Creative Commons license, users will need to obtain permission from the license holder to reproduce the material. To view a copy of this license, visit http://creativecommons.org/licenses/by-nc-sa/4.0/
About this article
Cite this article
Hu, Y., Yoshida, K., Cologne, J. et al. CD14 and IL18 gene polymorphisms associated with colorectal cancer subsite risks among atomic bomb survivors. Hum Genome Var 2, 15035 (2015). https://doi.org/10.1038/hgv.2015.35
Received:
Revised:
Accepted:
Published:
DOI: https://doi.org/10.1038/hgv.2015.35