Abstract
Background
Biomarker studies on colorectal cancer (CRC) prognosis are limited to pre-diagnostic or pre-operative measures. Post-treatment biomarkers are not well understood for their associations with CRC survival.
Methods
We included 306 eligible incident stage II–III CRC cases from the population-based Seattle Colon Cancer Family Registry. Concentrations of C-reactive protein (CRP), interleukin-6 (IL-6), monocyte chemoattractant protein-1 (MCP-1), adiponectin, and leptin were measured using post-treatment plasma samples. Adjusted hazard ratios (HRs) and 95% confidence intervals (CIs) for all-cause and CRC-specific mortality were calculated using Cox proportional hazard models.
Results
Elevated levels of CRP, IL-6, MCP-1, and adiponectin were significantly associated with a higher risk of all-cause mortality within 10 years post blood draw with HRs (95% CI) of 1.32 (1.10–2.59), 2.72 (2.07–3.56), 1.97 (1.18–3.28) and 1.71 (1.14–2.58), respectively. IL-6 and adiponectin had a dose–response effect (Ptrend < 0.0001). For CRC-specific mortality, we observed positive associations for CRP (HR = 1.75, 95% CI: 1.2–2.56), IL-6 (HR = 5.02, 95% CI: 2.92–8.59), MCP-1 (HR = 3.78, 95% CI: 1.41–10.08), and adiponectin (HR = 3.16, 95% CI: 1.27–7.86), and inverse association for leptin (HR = 0.44, 95% CI: 0.29–0.68) within the first year of blood draw, whereas the association for IL-6 remained statistically significant over 10 years.
Conclusion
Our results support the role of chronic inflammation in CRC progression and suggested several post-treatment inflammatory biomarkers, particularly IL-6, are promising prognostic markers for stage II–III CRC patients.
Similar content being viewed by others
Introduction
Inflammation plays an important role in both the development and progression of colorectal cancer (CRC) [1]. Evidence linking chronic inflammation to colorectal carcinogenesis implicates several mediators [2, 3]. These inflammation-modulating factors include cytokines and chemokines released by tumour-infiltrating immune cells and tumour cells. They can activate inflammatory responses and stimulate tumour growth and progression [3]. Obesity-induced low-grade systemic inflammation may contribute to colorectal carcinogenesis and tumour growth through altered levels of adipokines [2]. Thus, the dysregulation of these inflammatory biomarkers derived from either the tumour microenvironment or adipose tissue may affect CRC outcomes and may be informative in identifying CRC patients who are at higher risk for disease progression and mortality.
Observational studies of circulating inflammatory biomarkers and CRC survival have been primarily focused on the key acute-phase protein, C-reactive protein (CRP), and the major pro-inflammatory cytokine, interleukin-6 (IL-6). Positive correlations between elevated levels of CRP and IL-6 with larger tumour sizes, metastasis, and mortality among CRC patients have been reported [4,5,6]. However, these observational studies were limited to measures of either pre-diagnostic or pre-operative inflammatory markers. They cannot directly inform prognosis after completed treatment, a critical period when CRC patients are at greatest risk for disease recurrence and metachronous cancers.
In addition to CRP and IL-6, other inflammatory markers with biological relevance merit further investigation. Monocyte chemoattractant protein-1 (MCP-1), an essential chemokine, is responsible for the recruitment of monocytes, macrophages and other immune cells to the tumour microenvironment [7]. Studies have demonstrated that MCP-1 expression is associated with tumour stage, venous invasion and metastasis for multiple cancers [8,9,10]. The association between circulating MCP-1 levels and CRC survival is not well studied [11]. Adipocyte-released hormones—adiponectin and leptin—are strongly associated with obesity, and have also been linked to CRC development [12]. However, there is limited data on their associations with CRC survival [13].
In this study, we aimed to evaluate post-treatment circulating concentrations of biomarkers of systemic inflammation, including CRP, IL-6, MCP-1, adiponectin, and leptin, in relation to overall and CRC-specific mortality among patients diagnosed with CRC, and to assess whether these associations differ according to patient and tumour characteristics. To accomplish this, we leveraged the existing data and biospecimens from the Seattle Colon Cancer Family Registry (CCFR).
Materials and methods
Study population
The Seattle CCFR is a population-based site of the multi-centre international consortium CCFR [14]. The details of this consortium have been described previously [14, 15]. Briefly, incident invasive CRC cases were ascertained through the Surveillance, Epidemiology, and End Results (SEER) cancer registry covering 13 counties in western Washington State. All cases were invited to participate in Seattle CCFR without an additional sampling scheme (i.e. family history). Participants provided informed consent and completed a standardised telephone interview at enrolment (a median of 9.5 months after diagnosis) to provide information on demographics, personal and family history of cancer, CRC screening, medical history, medication use and lifestyle factors (e.g. physical activity, alcohol and tobacco use). Blood samples were collected after the baseline interview using ethylenediaminetetraacetic acid-treated vacutainers, processed within 48 h and plasma was stored at −70 °C until analysis. Paraffin-embedded tumour tissue was obtained from cases according to established CCFR protocols. Information on first-line treatment of the primary tumour (i.e. surgery, radiation and chemotherapy) was abstracted from SEER and medical records. All study participants were followed up for vital status, date and cause of death through linkages to SEER.
Eligible individuals for this study included population-based incident CRC cases aged 18–74 years diagnosed with stage II–III diseases between 1998 and 2007 from whom a blood specimen was obtained after active treatment. A total of 306 eligible participants were identified. The study protocol was approved by the institutional review board of the Fred Hutchinson Cancer Research Centre (Seattle, WA).
Biomarker measurement
We measured the circulating concentrations of all five biomarkers (CRP, IL-6, MCP-1, adiponectin, and leptin) using Meso Scale Discovery immunoassays (V-PLEX custom human biomarkers assay for CRP, IL-6 and MCP-1; human adiponectin kit and human leptin kit). All assays were performed on never-thawed samples except for CRP, which is stable through freeze–thaw cycles [16], and was measured in samples that had undergone one freeze–thaw cycle. All samples from the same individual were analysed on the same batch in duplicates. Quality control (QC) samples were randomly plated among the study samples across all batches. Laboratory personnel was blinded to study QC samples and all patients’ information including vital status. Study samples were plated randomly regardless of study outcome to reduce bias due to laboratory variation. The inter-plate coefficients of variation (CVs) for CRP, IL-6, MCP-1, adiponectin and leptin were 7.4, 9.4, 8.3, 5.9 and 3.9%, respectively. Intra-plate CVs for each marker on average were 1.7, 4.7, 4.9, 1.9 and 3.9%. No samples in this study had biomarker concentrations below the lower limit of detection for any biomarkers. The concentration of leptin for one sample was above the upper limit of the detection range. One sample had an extremely high value for MCP-1, although within the detection range. These samples were included in the main analysis, but were excluded in the sensitivity analysis.
Tumour characteristics
Tumour stage according to the American Joint Committee on Cancer (AJCC, 7th edition) was available for most eligible cases. For a subset of CRC cases whose AJCC staging was missing (n = 67), we used a standard algorithm to impute based on SEER summary staging and clinical TNM staging: stage II (SEER 1 and T3; SEER 3/7 and N0, M0) and stage III (SEER 3/4/7 and N1/N2, M0). Information on tumour location was determined based on the International Classification of Disease for Oncology, Third Edition (ICD-O-3) codes [17] abstracted from SEER, pathology records, or medical records. Colon cancer was defined as cancers arising from the caecum to the sigmoid colon (C180, C182–187 and C189). Rectal cancers consisted of cancers of the rectosigmoid junction or rectum (C199 and C209).
Tumour DNA was extracted from paraffin-embedded, formalin-fixed tumour tissues for tumour marker testing. Microsatellite instability (MSI) status was determined based on a ten-marker panel for the majority of cases: tumours were classified as MSI-high if instability was observed in ≥30% of markers and as microsatellite stable (MSS) or MSI-low if otherwise [18]. For other cases, MSI status was assessed using immunohistochemistry testing of MLH1, MSH2, MSH6 and PMS2 expression: patients with positive staining for all markers were considered MSS/MSI-low and as MSI-high if otherwise [19]. Previous studies demonstrated a high concordance (97%) between these two methods [19, 20]. Our data showed a similar level of agreement (98.4%) among samples tested using both methods [21]. Extracted tumour DNA was also tested for p.V600E BRAF mutation by using a fluorescent allele-specific polymerase chain reaction assay [22] and for coding sequence in KRAS exon 2 using forward and reverse sequencing [23]. CpG island methylator phenotype (CIMP) was determined using a validated five-marker DNA methylation assay (CACNA1G, IGF2, NEUROG1, RUNX3 and SOCS1) [24]. We classified tumours as CIMP-positive if three or more of five markers had a percentage of methylated reference ratio ≥10 and as CIMP-negative if otherwise [25].
Statistical analysis
We first performed a natural logarithmic transformation of all markers to ensure the concentrations of each biomarker were normally distributed. We then categorised each measure using sex-specific quartiles. Pearson correlation coefficients were used to evaluate the correlations among biomarkers and between each biomarker and years of plasma storage. We also compared the distributions of each biomarker by patients and tumour characteristics.
We used Cox proportional hazards regression to calculate adjusted hazard ratios (HRs) and the 95% confidence intervals (CIs) evaluating the association of each post-treatment biomarker with mortality. Time to event was defined as days between the date of blood draw to the date of death, last date of contact, or the end of follow-up. We used the International Classification of Diseases-9 (ICD-9) or ICD-10 (depending on the year of linkage) to define CRC-specific deaths, CRC being the primary cause of death (ICD-9: 153.0–153.4, 153.6–153.9 or 154.0–154.1; ICD-10: C18.0–20.0 or C26.0) [26]. All regression models were adjusted for a priori confounders, including age at blood draw, sex, pre-diagnostic body mass index (BMI), smoking status at baseline, regular use of non-steroidal anti-inflammatory drugs (NSAIDs) at baseline, stage at diagnosis, plasma storage time and years between diagnosis and blood draw. Pre-diagnostic measures of BMI was calculated based on self-reported height and weight at the date of reference, defined as 2 years before baseline interview (~1 year before diagnosis). The proportional hazard (PH) assumption was examined by testing for a nonzero slope of the scaled Schoenfeld residuals as a function of survival time. When the PH assumption was violated for a confounder, we used the stratified PH model. When the PH assumption was violated for an exposure variable (i.e. a biomarker), we then used the extended Cox models with time-varying coefficient, which allowed us to calculate interval-specific HRs (95% CIs) for the associations between biomarker and mortality within 1, 1–3 and >3 years after the blood draw. The time intervals were determined based on the Schoenfeld residual plots. Tests for trend were conducted by including the categorical variable (i.e. quartiles) in the model as an ordinal variable and calculating the Wald statistic.
In addition, sensitivity analyses were conducted excluding (1) patients with extremely high values of MCP-1 (n = 1) and leptin (n = 1) and (2) patients with CRP > 10 mg/L (n = 58) to ensure our study results were not driven by extreme values of these biomarkers or by individuals with an acute inflammation that may have affected their circulating levels of biomarkers.
We performed stratified analyses according to sex, smoking status (never vs ever), BMI (<25, 25–29.9 and ≥30 kg/m2), stage at diagnosis (II and III), and tumour characteristics (MSI, somatic BRAF and KRAS mutation status, and CIMP) since circulating concentrations of pro-inflammatory biomarkers are generally higher among females, smokers and people who are obese, and CRC survival is likely different by tumour characteristics. Tests for interaction were performed by adding the cross-product term of the biomarker and each of these potential effect modifiers in the regression models and P for interaction was calculated using likelihood ratio tests. All statistical analyses were performed using R 3.6.0 with a two-sided P value < 0.05 considered statistically significant.
Results
Study participants in this analysis were on average 55 years old at diagnosis (standard deviation, SD: 12.1 years). They were mostly white (87%), with an equal number of males and females. Baseline characteristics of the 306 eligible CRC cases according to quartiles of CRP are listed in Table 1. Compared to patients in the lowest quartile of CRP levels, those with elevated concentrations of CRP were more likely to be older at diagnosis, obese, ever-smokers, regular users of NSAIDs and longer plasma storage time. The distribution of these patients and clinical characteristics by other inflammatory biomarkers follows similar patterns, with the exception that people with an elevated level of IL-6 were also more likely to have a positive family history of CRC; people with higher adiponectin were less likely to be obese; and the observed pattern was different for leptin—patients with higher leptin concentrations were more likely to be obese, had diabetes, higher cholesterol and more likely to be diagnosed with colon cancer (Supplementary Table 1A–D). Sex-specific median, interquartile range [IQR]), and quartiles of each biomarker are summarised in Supplementary Table 2. Pair-wise Pearson correlation coefficients among all markers and between biomarkers and years of plasma storage are summarised in Supplementary Table 3. CRP was positively correlated with IL-6 (r = 0.53) and moderately correlated with MCP-1 (r = 0.27) and leptin (r = 0.26). No/weak inverse correlations were observed for leptin with IL-6 (r = −0.004) and with adiponectin (r = −0.019). Plasma storage time was positively correlated with IL-6 (r = 0.18) and adiponectin (r = 0.16). On average, patients who underwent surgical resection had significantly lower levels of post-treatment IL-6, whereas patients who underwent radiation had lower levels of leptin (Supplementary Fig. 1).
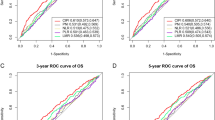
All-cause mortality
Over the 10-year follow-up, 94 out of 306 CRC patients (31%) died and 53 (18%) had CRC as their primary cause of death. Elevated concentrations of CRP, IL-6, MCP-1 and adiponectin were significantly associated with a higher risk of all-cause mortality (Table 2). The HRs (95% CIs) per unit increase in logarithmically transformed biomarkers were 1.32 (1.10–2.59), 2.72 (2.07–3.56), 1.97 (1.18–3.28) and 1.71(1.14–2.58) for CRP, IL-6, MCP-1, and adiponectin, respectively. In contrast, log-transformed concentrations of leptin were associated with a lower risk of overall mortality, although not reaching statistical significance (HR = 0.85, 95% CI: 0.70–1.03). We further evaluated the sex-specific quartiles of each marker in relation to all-cause mortality. Kaplan–Meier survival curves by sex-specific quartiles of all biomarkers are shown in Fig. 1. We observed a clear separation across the quartiles of IL-6 and moderate separation for adiponectin (Plog rank < 0.0001). For both markers, dose–response effects were observed in multivariable analyses (Table 2). Patients in the highest quartile of IL-6 had an almost 8-fold increase in overall mortality compared to those in the lowest quartile (HR = 7.87, 95% CI: 3.47–17.82, Ptrend < 0.0001). Patients in the highest quartile of adiponectin had a 3-fold increased risk of overall mortality compared to those in the lowest quartile (HR = 2.56, 95% CI: 1.34–4.90, Ptrend = 0.0011). We did not find evidence of dose–response effects for CRP, MCP-1 or leptin.
Comparing overall mortality in stage II–III colorectal cancer patients by sex-specific quartiles of circulating C-reactive protein (A), interleukin-6 (B), monocyte chemoattractant protein (MCP)-1 (C), adiponectin (D), and leptin (E), Seattle Colon Cancer Family Registry, 1998–2007 (n = 306). P values were based on log-rank tests.
After excluding cases with CRP > 10 mg/L (n = 58), logarithmic CRP, MCP-1, and leptin were no longer associated with overall mortality, whereas logarithmic IL-6 and adiponectin remained statistically significantly associated with a higher risk of overall mortality, with HRs (95% CIs) of 3.01 (2.1–4.32) and 1.87 (1.15–3.04) per unit increase in logarithmic biomarker (Table 2). Stronger dose–response effects were observed for IL-6: patients in the highest quartile had a >9-fold increased risk of overall mortality compared to those in the lowest quartile (HR = 9.50, 95% CI: 3.54–25.45, Ptrend < 0.0001, Table 2). Cases in the highest quartile of adiponectin had a 2.3 times higher risk of overall mortality compared to those in the lowest quartiles (HR = 2.32, 95% CI: 1.07–5.03, Ptrend = 0.0043, Table 2). Models with or without adjustment of prediagnosis BMI did not materially change the study results (Table 2).
CRC-specific mortality
Since the biomarkers violated the PH assumption for associations with CRC-specific mortality, we used the extended Cox models to calculate interval-specific HRs (95% CIs) for the associations between each logarithmic biomarker and CRC-specific mortality within 1, 1–3 and >3 years after the blood draw. Within the first year after the blood draw, we observed similar but stronger associations of logarithmic markers with CRC-specific mortality: CRP, IL-6, MCP-1 and adiponectin were associated with increased risks of CRC-specific mortality, with HRs (95% CI) of 1.75 (1.2–2.56), 5.01 (2.92–8.59), 3.78 (1.41–10.08) and 3.16 (1.27–7.86), respectively (Table 3); leptin was inversely associated with CRC-specific mortality (HR = 0.44, 95% CI: 0.29–0.68). However, these effects did not persist after year 1, except for IL-6. The positive associations between IL-6 and CRC-specific mortality remained statistically significant after 1 year, but the effect sizes attenuated over time (Table 3). In our sensitivity analysis excluding patients with CRP > 10 mg/L (n = 58), IL-6, adiponectin and leptin remained statistically significantly associated with CRC-specific mortality within the first year (Table 3).
Stratified analyses
In stratified analyses, we observed that CRP was associated with higher overall mortality among cases who were normal/underweight (HR = 1.76, 95% CI: 1.28–2.42, Pinteraction = 0.02, Table 4) but not among those who were overweight or obese, and among cases with MSI-high tumours (HR = 6.46, 95% CI: 2.04–20.49, Pinteraction = 0.007, Table 4), but not among those with MSS/MSI-low tumours. The observed association between IL-6 and higher risk of overall mortality was modified by BRAF mutation status, MSI and tumour location (Pinteraction = 0.02, 0.02 and 0.03, respectively, Table 4). MCP-1 was significantly associated with a 3-fold increased overall mortality among colon cancer patients (HR = 2.85, 95% CI: 1.66–4.87, Table 4), but not among patients with rectum cancers (Pinteraction = 0.0005). An inverse association between leptin and overall mortality was observed in patients with MSI-high tumours (HR = 0.29, 95% CI: 0.13–0.68, Pinteraction = 0.02) and those underwent radiation therapy (HR = 0.64, 95% CI: 0.44–0.92, Pinteraction = 0.03, Table 4), but not among those with MSS/MSI-low tumours or without radiation therapy. For adiponectin, we found no evidence of interactions with patient or tumour characteristics in relation to overall mortality.
Discussion
In this population-based study of stage II–III CRC patients, we observed dose–response effects of post-treatment circulating IL-6 and adiponectin on all-cause mortality over the 10-year follow-up period. Adiponectin was associated with higher CRC-specific mortality within the first year of blood draw, whereas IL-6 remained significantly associated with a higher risk of CRC-specific mortality over 10 years, although the effect sizes attenuated with time. CRP and MCP-1 were also associated with higher all-cause mortality over the 10-year follow-up as well as CRC-specific mortality within the first year of blood draw. However, no association was observed when restricting to patients with CRP < 10 mg/L. In contrast, post-treatment leptin was not associated with overall mortality but was inversely associated with CRC-specific mortality within the first year of blood draw. These results are all independent of pre-diagnostic BMI.
IL-6
Several lines of evidence support our findings that higher circulating levels of IL-6 were associated with a worse prognosis among CRC patients. Observational studies demonstrated that CRC patients with higher concentrations of serum IL-6 before treatment had a two to four times higher risk of overall mortality [27,28,29,30]. In vitro studies also demonstrated that IL-6 can stimulate tumour growth in both primary and metastatic colon cancer cell lines [31]. Consistently, IL-6-deficient mice, after injected with colon cancer cells, had significantly decreased tumour growth and increased tumour-infiltrating immune cells (i.e. mature dendritic cells, helper T cells and cytotoxic T cells) in the tumour microenvironment compared with wild-type mice [32].
The long-term effect of IL-6 observed in our study was, supported in part by Yeh et al., that CRC patients with IL-6 > 10 pg/mL had a 2.4 times higher risk of 10-year overall mortality [29]. Mechanisms underlying this observation is likely to be multifacet through both promotion of the tumour growth and the inhibitory effects on immune cells. This likely involves the trans-signalling pathway, where the IL-6/soluble IL-6 receptor complex can bind to gp130 and target a variety of cells including tumour cells and tumour-infiltrating immune cells. These can activate the downstream intracellular JAK/STAT3 signalling cascade, promoting tumour cell proliferation, survival, invasiveness and metastasis, and inhibiting the immune responses against the tumour through down-regulation of neutrophils, natural killer cells, effector T cells and dendritic cells [33].
Our study found that the association between circulating IL-6 and overall mortality was stronger in patients with BRAF-mutant tumours compared to those with BRAF wild-type CRCs. It is supported by Thomsen et al. [27], a study of 393 patients with metastatic CRC, where a more pronounced association between IL-6 and overall mortality was observed in patients with BRAF mutation. Although the underlying mechanism is unclear, it is likely that the somatic BRAF mutation and elevated IL-6 act in synergy in promoting tumour growth and progression through the BRAF kinase and JAK/STAT3 signalling pathways.
It is noteworthy that circulating IL-6 levels in our study (median = 1.0, IQR: 0.6–1.6 pg/mL) are lower than what has been generally reported in the literature among CRC patients [6, 34, 35]. This may be because our study population included only stage II–III CRC patients, and circulating IL-6 level increase with the tumour stage [30]. Also, post-treatment systemic inflammation is likely to be lower compared to that during the pre-operative period when the tumour is present. Tumour-associated inflammation could lead to an elevated level of circulating inflammatory markers.
Adiponectin
Several epidemiologic studies have reported that elevated concentrations of circulating adiponectin were associated with a lower risk of developing CRC [36,37,38]. However, studies that reported the impact of circulating adiponectin on CRC survival are few and had inconsistent results. One hospital-based study of 344 CRC patients found that adiponectin measured at the time of diagnosis was not associated with CRC survival [39]. Another small study of 60 patients with non-metastatic CRC reported low adiponectin levels measured before treatment was associated with disease recurrence [40]. Chong et al. conducted a prospective study of 621 incident CRC cases and found that pre-diagnostic plasma adiponectin was positively associated with increased risk of both overall and CRC-specific mortality over a median of 9-year follow-up [13]. Patients in the highest vs lowest quartile of adiponectin had a 66% higher risk of overall mortality and a nearly two-fold increased risk of CRC-specific mortality. We observed similar associations with a stronger effect for post-treatment adiponectin with overall and CRC-specific mortality in our study population.
The diverging associations of adiponectin with CRC risk and survival are worth noting. Although the underlying mechanism is unclear, it is likely that individuals with elevated adiponectin levels, who then develop CRC, may have tumours that originated through alternative pathways, and that elevated adiponectin levels can exert a pro-inflammatory effect that associated with adverse disease outcomes. Similarly, adiponetin is associated with a lower risk of developing cardiovascular disease (CVD), but for patients diagnosed with CVD, elevated circulating adiponectin was shown to be associated with higher CVD-specific mortality [41]. Further, studies demonstrated the pleiotropic effect of adiponectin [42]. Convincing evidence showed that circulating adiponectin is inversely associated with visceral obesity, type 2 diabetes, CVD and metabolic syndrome [43]. Other studies found pro-inflammatory effects of adiponectin in chronic inflammatory and autoimmune diseases, such as rheumatoid arthritis [44], inflammatory bowel disease [45] and type 1 diabetes [46]. In human colonic epithelial cells, adiponectin exerted pro-inflammatory effects by inducing chemokine production and it promotes colonic cell proliferation in a dose-dependent manner [47]. Together, these evidences suggest that adiponectin may exert pro-inflammatory properties in the tumour microenvironment that facilitate tumour proliferation and metastasis, leading to a worse prognosis.
Obesity, CRP and leptin
Since obesity-induced inflammation was shown to play an important role in carcinogenesis, we evaluated the effect of additional adjustment of prediagnosis BMI in our analysis and found that the associations were not materially changed for all markers. Our stratified analysis by BMI found that the association between elevated post-treatment CRP concentrations and overall mortality was only among normal/underweight individuals, but not among patients who were obese. This finding was further supported by Swede et al. who evaluated waist circumference (WC) in addition to BMI and observed similar patterns of effect modification by BMI and WC: the associations between pre-diagnostic circulating CRP and increased CRC-specific mortality were much stronger among those with a normal BMI compared to overweight/obese individuals and among those with a normal sex-specific WC compared to people with at-risk WC [48]. Together, these suggest that the impact of chronic inflammation on CRC survival may be independent of excess body fat.
Leptin, a biomarker strongly correlated with adiposity, was shown in our study to be associated with improved CRC-specific survival within the first year of blood draw. Although direct evidence on leptin in relation to CRC survival is lacking, our finding is in line with previous studies. Exiting evidence suggested a J-shaped association between body weight and CRC survival: patients who are overweight at and after the time of CRC diagnosis had the lowest risk of mortality [49, 50]. Further, our previous study of long-term CRC survivor showed that patients who maintained body weight ~5 years after diagnosis had better survival compared to those who experienced weight loss [51]. Although future studies are needed to validate the association between post-treatment leptin and CRC survival as well as the underlying mechanisms, these findings suggest that maintaining body weight in CRC patients who are overweight may be important and recommendations for weight loss among these patients may be unwarranted.
Limitations and strengths
Several limitations need to be considered when interpreting our study results. First, post-treatment inflammatory biomarkers were measured only once; repeated measurements in both pre- and post-treatment periods in future studies would better capture intra-individual variabilities and characterise systemic inflammation over time among CRC patients. Second, selection bias may be of concern because our study only included cases for whom blood was collected after active treatment (1–3 years after CRC diagnosis). However, the comparison between our study population and all stage II–III CRC patients from the parent study, the Seattle CCFR, showed similar distributions of baseline patients and tumour characteristics (Supplementary Table 4). We only included stage II and III CRC patients in this study because (1) stage I CRC patients have relatively high 5-year survival rates (~90%), which can limit the power for survival analysis, and (2) study participation for stage IV patients was relatively low due to high mortality in this group. This limited the generalisability of our findings. In addition, we included pre-diagnostic BMI to evaluate the potential impact of obesity-associated inflammation on the association between post-treatment biomarkers of inflammation and survival. However, post-treatment measures of obesity around the time of blood draw as well as other measures of adiposity (i.e. WC) are desired. Lastly, although this study is well powered for the main analysis, our subgroup analyses had limited power for subgroups with limited sample size and need to be interpreted with caution due to potential inflated type I error.
This study also has many strengths. Our study population is well characterised: standardised questionnaires provided detailed information on potential confounders associated with inflammation; tumour characterisations enhanced our ability to conduct stratified analyses to improve the specificity of our study findings. Circulating biomarkers were measured using standardised and validated assays with QC procedures. The assays performed extremely well with no values below the assay level of detection and low inter- and intra-plate CVs. The long follow-up time of the Seattle CCFR allowed us to study long-term survival, and to evaluate time-varying associations. In addition, the circulating inflammatory biomarkers in this study were measured after the completion of treatments. We incorporated a lag time between diagnosis and blood draw (1–3 years, median 1.4 years) to preclude acute treatment effects or acute diseases.
Conclusion
In this population-based study of stage II–III CRC patients, post-treatment circulating CRP, MCP-1 and adiponectin concentrations are associated with higher all-cause mortality over 10 years, but only within the first year for CRC-specific mortality. Elevated levels of IL-6 is associated with both overall and CRC-specific mortality over 10 years after blood draw. In contrast, post-treatment leptin levels were not associated with overall mortality, but were inversely associated with CRC-specific mortality within the first year of blood draw.
To the best of our knowledge, this is the first study that directly evaluated post-treatment markers of systemic inflammation in association with CRC survival and suggests that IL-6 is an informative prognostic biomarker for both all-cause and CRC-specific mortality. Although these results need further validation, they support the role of chronic inflammation in CRC progression and the potential of using inflammatory markers to identify subsets of patients at higher risk for targeted CRC surveillance and post-treatment care.
Data availability
The data that support the findings of this study will be made available upon reasonable request and contingent upon the requester obtaining the necessary human subjects approvals.
References
Terzic J, Grivennikov S, Karin E, Karin M. Inflammation and colon cancer. Gastroenterology. 2010;138:2101–14.e2105.
Aleman JO, Eusebi LH, Ricciardiello L, Patidar K, Sanyal AJ, Holt PR. Mechanisms of obesity-induced gastrointestinal neoplasia. Gastroenterology. 2014;146:357–73.
Lin WW, Karin M. A cytokine-mediated link between innate immunity, inflammation, and cancer. J Clin Invest. 2007;117:1175–83.
Nozoe T, Matsumata T, Kitamura M, Sugimachi K. Significance of preoperative elevation of serum C-reactive protein as an indicator for prognosis in colorectal cancer. Am J Surg. 1998;176:335–8.
Crozier JE, McKee RF, McArdle CS, Angerson WJ, Anderson JH, Horgan PG, et al. The presence of a systemic inflammatory response predicts poorer survival in patients receiving adjuvant 5-FU chemotherapy following potentially curative resection for colorectal cancer. Br. J. Cancer. 2006;94:1833–6.
Nikiteas NI, Tzanakis N, Gazouli M, Rallis G, Daniilidis K, Theodoropoulos G, et al. Serum IL-6, TNFalpha and CRP levels in Greek colorectal cancer patients: prognostic implications. World J Gastroenterol. 2005;11:1639–43.
Balkwill F. Cancer and the chemokine network. Nat Rev Cancer. 2004;4:540–50.
Monti P, Leone BE, Marchesi F, Balzano G, Zerbi A, Scaltrini F, et al. The CC chemokine MCP-1/CCL2 in pancreatic cancer progression: regulation of expression and potential mechanisms of antimalignant activity. Cancer Res. 2003;63:7451–61.
Qian BZ, Li J, Zhang H, Kitamura T, Zhang J, Campion LR, et al. CCL2 recruits inflammatory monocytes to facilitate breast-tumour metastasis. Nature. 2011;475:222–5.
Bailey C, Negus R, Morris A, Ziprin P, Goldin R, Allavena P, et al. Chemokine expression is associated with the accumulation of tumour associated macrophages (TAMs) and progression in human colorectal cancer. Clin Exp Metastasis. 2007;24:121–30.
Szczepanik AM, Siedlar M, Szura M, Kibil W, Brzuszkiewicz K, Brandt P. et al. Preoperative serum chemokine (C-C motif) ligand 2 levels and prognosis in colorectal cancer. Pol Arch Med Wewn. 2015;125:443–51.
Murphy, N, Jenab, M & Gunter, MJ Adiposity and gastrointestinal cancers: epidemiology, mechanisms and future directions. Nat Rev Gastroenterol Hepatol. 2018. https://doi.org/10.1038/s41575-018-0038-1.
Chong DQ, Mehta RS, Song M, Kedrin D, Meyerhardt JA, Ng K, et al. Prediagnostic plasma adiponectin and survival among patients with colorectal cancer. Cancer Prev Res. 2015;8:1138–45.
Newcomb PA, Baron J, Cotterchio M, Gallinger S, Grove J, Haile R, et al. Colon Cancer Family Registry: an international resource for studies of the genetic epidemiology of colon cancer. Cancer Epidemiol Biomark Prev. 2007;16:2331–43.
Jenkins MA, Win AK, Templeton AS, Angelakos MS, Buchanan DD, Cotterchio M, et al. Cohort Profile: The Colon Cancer Family Registry Cohort (CCFRC). Int J Epidemiol. 2018;47:387–8i.
Aziz N, Fahey JL, Detels R, Butch AW. Analytical performance of a highly sensitive c-reactive protein-based immunoassay and the effects of laboratory variables on levels of protein in blood. Clin Diagn Lab Immunol. 2003;10:652–7.
Fritz A,PC, Jack A, Shanmugaratnam K, Sobin L, Parkin DM, Whelan S. International classification of diseases for oncology, third edition. Geneva: World Health Organization; 2000.
Boland CR, Thibodeau SN, Hamilton SR, Sidransky D, Eshleman JR, Burt RW, et al. A National Cancer Institute Workshop on Microsatellite Instability for cancer detection and familial predisposition: development of international criteria for the determination of microsatellite instability in colorectal cancer. Cancer Res. 1998;58:5248–57.
Lindor NM, Burgart LJ, Leontovich O, Goldberg RM, Cunningham JM, Sargent DJ, et al. Immunohistochemistry versus microsatellite instability testing in phenotyping colorectal tumors. J Clin Oncol. 2002;20:1043–8.
Cicek MS, Lindor NM, Gallinger S, Bapat B, Hopper JL, Jenkins MA, et al. Quality assessment and correlation of microsatellite instability and immunohistochemical markers among population- and clinic-based colorectal tumors results from the Colon Cancer Family Registry. J Mol Diagn. 2011;13:271–81.
Hua X, Phipps AI, Burnett-Hartman AN, Adams SV, Hardikar S, Cohen SA, et al. Timing of aspirin and other nonsteroidal anti-inflammatory drug use among patients with colorectal cancer in relation to tumor markers and survival. J Clin Oncol. 2017;35:2806–13.
Buchanan DD, Sweet K, Drini M, Jenkins MA, Win AK, English DR, et al. Risk factors for colorectal cancer in patients with multiple serrated polyps: a cross-sectional case series from genetics clinics. PLoS ONE. 2010;5:e11636.
Oliner K, Juan T, Suggs S, Wolf M, Sarosi I, Freeman DJ, et al. A comparability study of 5 commercial KRAS tests. Diagn Pathol. 2010;5:23.
Weisenberger DJ, Siegmund KD, Campan M, Young J, Long TI, Faasse MA. et al. CpG island methylator phenotype underlies sporadic microsatellite instability and is tightly associated with BRAF mutation in colorectal cancer. Nat Genet. 2006;38:787–93.
Leggett B, Whitehall V. Role of the serrated pathway in colorectal cancer pathogenesis. Gastroenterology. 2010;138:2088–100.
Organization WH. International classification of diseases,tenth revision (ICD-10). Geneva: World Health Organization; 2004.
Thomsen M, Kersten C, Sorbye H, Skovlund E, Glimelius B, Pfeiffer P, et al. Interleukin-6 and C-reactive protein as prognostic biomarkers in metastatic colorectal cancer. Oncotarget. 2016;7:75013–22.
Shimazaki J, Goto Y, Nishida K, Tabuchi T, Motohashi G, Ubukata H, et al. In patients with colorectal cancer, preoperative serum interleukin-6 level and granulocyte/lymphocyte ratio are clinically relevant biomarkers of long-term cancer progression. Oncology. 2013;84:356–61.
Yeh KY, Li YY, Hsieh LL, Lu CH, Chou WC, Liaw CC, et al. Analysis of the effect of serum interleukin-6 (IL-6) and soluble IL-6 receptor levels on survival of patients with colorectal cancer. Jpn J Clin Oncol. 2010;40:580–7.
Belluco C, Nitti D, Frantz M, Toppan P, Basso D, Plebani M. et al. Interleukin-6 blood level is associated with circulating carcinoembryonic antigen and prognosis in patients with colorectal cancer. Ann Surg Oncol. 2000;7:133–8.
Schneider MR, Hoeflich A, Fischer JR, Wolf E, Sordat B, Lahm H. Interleukin-6 stimulates clonogenic growth of primary and metastatic human colon carcinoma cells. Cancer Lett. 2000;151:31–38.
Ohno Y, Toyoshima Y, Yurino H, Monma N, Xiang H, Sumida K, et al. Lack of interleukin-6 in the tumor microenvironment augments type-1 immunity and increases the efficacy of cancer immunotherapy. Cancer Sci. 2017;108:1959–66.
Johnson DE, O’Keefe RA, Grandis JR. Targeting the IL-6/JAK/STAT3 signalling axis in cancer. Nat Rev Clin Oncol. 2018;15:234–48.
Knupfer H, Preiss R. Serum interleukin-6 levels in colorectal cancer patients-a summary of published results. Int J Colorectal Dis. 2010;25:135–40.
Galizia G, Orditura M, Romano C, Lieto E, Castellano P, Pelosio L. et al. Prognostic significance of circulating IL-10 and IL-6 serum levels in colon cancer patients undergoing surgery. Clin Immunol. 2002;102:169–78.
Song M, Zhang X, Wu K, Ogino S, Fuchs CS, Giovannucci EL, et al. Plasma adiponectin and soluble leptin receptor and risk of colorectal cancer: a prospective study. Cancer Prev Res. 2013;6:875–85.
Wei EK, Giovannucci E, Fuchs CS, Willett WC, Mantzoros CS. Low plasma adiponectin levels and risk of colorectal cancer in men: a prospective study. J Natl Cancer Inst. 2005;97:1688–94.
Xu XT, Xu Q, Tong JL, Zhu MM, Huang ML, Ran ZH, et al. Meta-analysis: circulating adiponectin levels and risk of colorectal cancer and adenoma. J Dig Dis. 2011;12:234–44.
Volkova E, Willis JA, Wells JE, Robinson BA, Dachs GU, Currie MJ. Association of angiopoietin-2, C-reactive protein and markers of obesity and insulin resistance with survival outcome in colorectal cancer. Br. J. Cancer. 2011;104:51–59.
Ferroni P, Palmirotta R, Spila A, Martini F, Raparelli V, Fossile E, et al. Prognostic significance of adiponectin levels in non-metastatic colorectal cancer. Anticancer Res. 2007;27:483–9.
Dekker JM, Funahashi T, Nijpels G, Pilz S, Stehouwer CDA, Snijder MB, et al. Prognostic value of adiponectin for cardiovascular disease and mortality. J Clin Endocrinol Metab. 2008;93:1489–96.
Fantuzzi G. Adiponectin and inflammation: consensus and controversy. J Allergy Clin Immunol. 2008;121:326–30.
Chandran M, Phillips SA, Ciaraldi T, Henry RR. Adiponectin: more than just another fat cell hormone? Diabetes Care. 2003;26:2442–50.
Schäffler A, Ehling A, Neumann E, Herfarth H, Tarner I, Schölmerich J, et al. Adipocytokines in synovial fluid. JAMA. 2003;290:1709–10.
Yamamoto K, Kiyohara T, Murayama Y, Kihara S, Okamoto Y, Funahashi T, et al. Production of adiponectin, an anti-inflammatory protein, in mesenteric adipose tissue in Crohn’s disease. Gut. 2005;54:789–96.
Perseghin G, Lattuada G, Danna M, Sereni LP, Maffi P, De Cobelli F, et al. Insulin resistance, intramyocellular lipid content, and plasma adiponectin in patients with type 1 diabetes. Am J Physiol Endocrinol Metab. 2003;285:E1174–1181.
Ogunwobi OO, Beales ILP. Adiponectin stimulates proliferation and cytokine secretion in colonic epithelial cells. Regul Pept. 2006;134:105–13.
Swede H, Hajduk AM, Sharma J, Rawal S, Rasool H, Vella AT, et al. Baseline serum C-reactive protein and death from colorectal cancer in the NHANES III cohort. Int J Cancer. 2014;134:1862–70.
Wu S, Liu J, Wang X, Li M, Gan Y, Tang Y. Association of obesity and overweight with overall survival in colorectal cancer patients: a meta-analysis of 29 studies. Cancer Causes Control. 2014;25:1489–502.
Kroenke CH, Neugebauer R, Meyerhardt J, Prado CM, Weltzien E, Kwan ML, et al. Analysis of body mass index and mortality in patients with colorectal cancer using causal diagrams. JAMA Oncol. 2016;2:1137–45.
Kocarnik JM, Hua X, Hardikar S, Robinson J, Lindor NM, Win AK, et al. Long‐term weight loss after colorectal cancer diagnosis is associated with lower survival: the Colon Cancer Family Registry. Cancer. 2017;123:4701–8.
Acknowledgements
The SCCFR and the PMH study graciously thanks the generous contributions of their study participants, the dedication of study staff and the financial support from the National Cancer Institute, without which this important research was not possible. The content of this manuscript does not necessarily reflect the views or policies of the NIH or SCCFR, nor does it mention the trade names, commercial products, or organisations, implying endorsement by the US Government, the SEER Programme or the CCFR.
Funding
The Colon Cancer Family Registry (CCFR, www.coloncfr.org) is supported in part by funding from the National Cancer Institute (NCI), National Institutes of Health (NIH) through award U01 CA167551. Additional funding for the Seattle CCFR was through NCI grants U01 CA074794 (to JYD) and U24 CA074794 and R01 CA076366 (to PAN). Support for Seattle CCFR case ascertainment was provided in part from the Surveillance, Epidemiology, and End Results (SEER).
Author information
Authors and Affiliations
Contributions
XH: contributed to study concept and design, data and funding acquisition, analysis and interpretation of data, drafting the manuscript and revising the manuscript. MK and PAN: contributed to study concept and design, funding support, data and funding acquisition, interpretation of data and revising the manuscript. RCM, JYD, SL and YZ: contributed to study concept, interpretation of data and revising the manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The study protocol was approved by the institutional review board of the Fred Hutchinson Cancer Research Center (Seattle, WA).
Consent to publish
Yes.
COMPETING INTERESTS
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
About this article
Cite this article
Hua, X., Kratz, M., Malen, R.C. et al. Association between post-treatment circulating biomarkers of inflammation and survival among stage II–III colorectal cancer patients. Br J Cancer 125, 806–815 (2021). https://doi.org/10.1038/s41416-021-01458-y
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41416-021-01458-y
This article is cited by
-
Postoperative serum interleukin-6 levels correlate with survival in stage I-III colorectal cancer
BMC Gastroenterology (2023)
-
Bodywide ecological interventions on cancer
Nature Medicine (2023)