Abstract
In the age-related macular degeneration (AMD) ‘inflammation model’, local inflammation plus complement activation contributes to the pathogenesis and progression of the disease. Multiple genetic associations have now been established correlating the risk of development or progression of AMD. Stratifying patients by their AMD genetic profile may facilitate future AMD therapeutic trials resulting in meaningful clinical trial end points with smaller sample sizes and study duration.
Similar content being viewed by others
Introduction
Based on the pioneering work of Dr Judah Folkman, novel research into ‘angiogenesis’ generated the commercial development of drugs to inhibit the growth of new blood vessels. This approach was developed as a strategy to ‘treat’ cancer as well as eye diseases that lead to progressive, irreversible visual loss. Pegaptanib was designed and approved by the FDA in 2004 as a valid treatment for age-related macular degeneration (AMD),1 followed by the publication of the landmark phase 3 ranibizumab data in 2006,2 and the published results of the short-term safety and efficacy of intravitreal bevacizumab, the ‘parent’ compound of ranibizumab, in patients with neovascular AMD (nAMD), by Rich et al.3
Since then, anti-vascular endothelial growth factor (VEGF) therapy has monopolized the treatment of nAMD.
However, AMD is a multifactorial, complex disease. Thus it seems unlikely that a single therapy that targets only the final result of a highly complicated pathogenetic process, will remain as the only viable treatment option in the future. Moreover, geographic atrophy (GA), the advanced non-neovascular form of AMD that accounts for 35% of all cases of late AMD and 20% of legal blindness attributable to AMD,4, 5 cannot be treated or prevented at the moment and indeed may be increased by anti-VEGF therapy.6, 7
In this review, we present and comment on the response to both complement and non-complement-based treatments, in relation to complement pathway mechanisms and complement gene regulation of these mechanisms. We discuss current and potential treatments for both wet and dry AMD in relation to complement pathway pathogenetic mechanisms.
The complement system
The innate immune system is composed of immunological effectors that provide robust, immediate, and nonspecific immune responses. These include evolutionarily primitive humoral, cellular, and mechanical processes that have a vital role in the protection of the host from pathogenic challenge. The complement system is a vital component of innate immunity and represents one of the major effector mechanisms of the innate immune system. It was so named for its ability to ‘complement’ the antibacterial properties of antibody in the heat-stable fraction of serum.8
The complement is a complex network of plasma and membrane-associated serum proteins, which are organized into a hierarchy of proteolytic cascades that start with the identification of pathogenic surfaces and lead to the generation of potent proinflammatory mediators (anaphylatoxins), opsonization (‘coating’) of the pathogenic surface through various complement opsonins (eg, C3b), and targeted lysis of the pathogenic surface through the assembly of membrane-penetrating pores known as the membrane attack complex (MAC).9, 10
The alternative pathway is in a continuous low-level state of activation characterized by the spontaneous hydrolysis of C3 into C3a and C3b fragments. C3b binds complement factor B (CFB) and, once bound, factor B is cleaved by complement factor D (CFD) into Ba and Bb, thereby forming the active C3 convertase (C3bBb). The convertase cleaves additional C3 molecules, generating more C3a and C3b, thereby promoting further amplification of the cascade.11
Activation of all complement pathways results in a proinflammatory response including generation of MACs, which mediate cell lysis, release of chemokines to attract inflammatory cells to the site of damage, and enhancement of capillary permeability.12, 13 Complement regulation occurs predominantly at two steps within the cascades, at the level of the convertases, both in their assembly and in their enzymatic activity, and during assembly of the MAC.14
There is an ‘interplay’ between adaptive and innate immunity. The adaptive immune system is organized around two classes of specialized lymphocytes, T and B cells, which display an extremely diverse repertoire of antigen-specific recognition receptors that enable specific identification and elimination of pathogens, as well as adaptive immune measures that ensure tailored immune responses, as well as long-lived immunological memory against re-infection.8 The ability of complement not only to affect robust innate immune responses but also to interface with, and influence T- and B-cell biology and adaptive responses, has become increasingly appreciated. However, the exact mechanism(s) by which complement mediates T-cell immunity has yet to be determined.15
AMD heritability
To accelerate progress in the discovery of macular degeneration genetics, 18 research groups from across the world formed the AMD Gene Consortium in the early 2010 and organized a meta-analysis of genome-wide association studies (GWAS). The meta-analysis evaluated the evidence for association at 2.442.884 single-nucleotide polymorphisms (SNPs) coming from >17 100 cases with advanced disease (GA, neovascularization, or both) and >60 000 controls.16 Joint analysis of discovery and follow-up studies17 resulted in the identification/confirmation of 19 AMD susceptibility loci reaching P<5 × 10−8. This included all susceptibility loci previously reaching P<5 × 10−8 and an additional seven new loci reaching P<5 × 10−8 for the first time. Two genes showed differential expression between post-mortem retina of young (ages 17–35) and elderly (ages 75 and 77 years) individuals: CFH (P=0.009) and VEGFA (P=0.003), both with increased expression in older individuals. Increased C3 expression was revealed in adult retinal pigment epithelium (RPE) compared with fetal RPE (P=0.0008). CFH, VEGFA, and C3 are thus upregulated with aging, and their role in AMD may indicate an accelerated aging process. In addition to C3 and CFH, all the complement genes with detectable expression in the retina or RPE experiments showed higher expression levels in older tissue. CFH risk alleles were preferentially associated with risk of GA. Variants near CFH exhibited a stronger evidence for association among Europeans (P=0.0000001).
CFH gene variants associated with AMD
A number of complement system proteins, complement activators, and complement regulatory proteins were identified as molecular constituents of drusen, the hallmark extracellular deposits associated with early AMD.18, 19 In this ‘inflammation’ model, local inflammation accompanied by complement activation, bystander cell lysis, and immune responsiveness are important facets of AMD pathogenesis and progression.20, 21, 22
Macrophages and the related giant cells have been demonstrated in histologic specimens from patients with AMD, especially in regions of RPE atrophy, breakdown of Bruch's membrane, and choroidal neovascularisation.23, 24, 25, 26 Moreover, as with uveitis, chemokines that mediate macrophage recruitment to the retina have also been associated with AMD.
Patel and Chan’s study, as well as prior studies showing increased oxidized lipoprotein levels with age in normal eyes and AMD eyes, suggests that the macrophages seen in AMD and in choroidal neovascularization (CNV) lesions might serve to ingest oxidized low-density lipoprotein that accumulates with age.15, 27, 28 The study did not clarify whether these macrophages serve maladaptive functions leading to CNV development or adaptive responses to the accumulation of oxidized protein and/or other pathological processes.15 In other words, before AMD develops, macrophages function as housekeepers in removing waste products from the retina and RPE. After AMD develops, especially wet AMD, macrophages function as inflammatory stimulators, thereby exacerbating the lesion.
Any genetic polymorphism or environmental stressor, which activates complement or impairs complement regulation leads to overactivity of the complement system. This results in inflammatory damage to the retina.29, 30, 31, 32, 33, 34, 35, 36 Complement activation also leads to VEGF upregulation, promoting CNV.37, 38 Influx of tissue-destructive M1 macrophages also potentiates ocular inflammation, leading to further tissue damage. At this point, M2 macrophages involved in tissue remodeling might also serve pro-angiogenic functions.15 M1 macrophages have considerable proinflammatory activities that promotes tissue damage; the release of proinflammatory cytokines and production of reactive oxygen and nitrogen species. M2 macrophages are less inflammatory and they promote scavenging, immunoregulation, and tissue remodeling.39
Therefore, new therapeutic approaches can be envisioned, designed to restore the complement-modulating activity that is deficient in genetically susceptible individuals.
The CFH Y402H risk variant
A SNP (T1277C) in one of the short consensus repeat domains (SCR7) of the CFH gene results in an amino acid substitution of histidine for tyrosine at position 402 in a CFH domain that contains binding sites for C-reactive protein (CRP), heparin, and streptococcal M6 protein.40
Clark et al demonstrated that the AMD-associated 402H variant binds less well to heparan sulfate and dermatan sulfate glycosaminoglycans within Bruch's membrane when compared with the 402Y form, although there was a similar level of binding of the two variants within the RPE. They proposed that the impaired binding of the 402H variant to Bruch's membrane results in an overactivation of the complement pathway leading to local chronic inflammation and thus contributes directly to the development and/or progression of AMD.41
Despite differences in binding properties, there are no detectable differences in either CFH or CRP immunolabeling in drusen between CFH402HH and CFH402YY homozygotes. However, CFH402HH homozygotes do show elevated levels of CRP in the choroid that is apparently systemic in origin, as there is no evidence for CRP transcription in either the RPE, neural retina, or choroid in vivo.42
This is supported by a case-control study of Seddon et al’ of 1026 participants at two centers in the Age-Related Eye Disease Study (AREDS), which showed that CRP levels were significantly higher among patients with advanced AMD than among those without AMD and suggested that elevated CRP level is an independent risk factor for AMD and may implicate the role of inflammation in its pathogenesis.43
These results suggest that CRP is most likely extravasated from the choroidal capillaries, in response to local signals generated by the RPE–choroid. The recruitment of circulating CRP to the choroid is most likely an indication of cellular injury that may be exacerbated by the reduced binding of CRP to CFH402HH, diminished complement regulatory activity, and heightened complement activation in predisposed ‘risk’ individuals. Presence of the CFH Y402H polymorphism increases the risk of AMD significantly, with an odds ratio (OR) of 2.5 and 6.3 for the heterozygous CT (YH) and homozygous CC (HH) genotypes, respectively.44
Other complement regulatory components linked to AMD
Vitronectin and clusterin are two negative regulators of the complement cascade that are present in drusen, including drusen in patients with AMD.19, 22 RPE cells near drusen show increased levels of cytoplasmic vitronectin, perhaps a compensatory response to complement attack.22 Another complement inhibitor, cluster of differentiation 46 (CD46; also known as membrane cofactor protein), is similarly present in drusen and expressed at high levels in RPE cells adjacent to drusen.22, 33
Gold et al screened CFB and complement component 2 (C2) genes in two independent cohorts of patients with or without AMD and found that two haplotypes—L9H BF/E318D C2 and R32Q BF/a variant in intron 10 of C2—were protective for AMD.45, 46 Combined analyses of the CFH and CFB/C2 variants indicated that they can account for nearly 75% of all AMD cases in the European and North American populations.45
Two non-synonymous polymorphisms in the C3 gene were also reported to be associated with AMD.47, 48, 49, 50 C3 is an acute phase reactant and is among the most highly expressed complement-related genes in the choroid, relative to adult liver.
Amyloid-beta, an aggregate found in drusen, is also found in the brains of patients with Alzheimer's disease, where it has been demonstrated in vitro to activate complement.51 Co-localization of amyloid-beta with C3 activation products in human AMD eyes suggests that amyloid-beta in AMD lesions might similarly activate complement.52
Accumulation of lipofuscin and A2E, the bis-retinoid component of lipofuscin, are early pathologic features of AMD, and in vitro photooxidation of A2E in RPE cells leads to complement activation.36
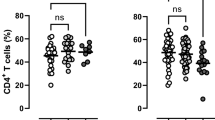
Activation products C3a, C5a, and C5b-9 are systemically elevated in patients suffering from AMD.53, 54, 55, 56 Locally, C5a and C3a accumulate in drusen and are shown to promote CNV.37 Liu et al showed that C5a protected human CD4+ T cells from undergoing apoptosis and C5a promoted IL-22 and IL-17 expression from CD4+ T cells of AMD patients and normal subjects as well.57 Consistent with the previous observation of elevated C5a expression in the serum of AMD patients, they found significantly increased levels of IL-22 and IL-17 in the sera of AMD patients, suggesting possible roles of IL-22 and IL-17 in the inflammation that contributes to AMD. Targeting the adaptive immune system, more specifically the Th17 family of cytokines, may have a beneficial effect on the course of AMD.
AMD-associated variations in a region in close proximity to another alternative pathway gene (CFI) on chromosome 4 have also been reported. The rs10033900 variant of the CFI gene has been shown to be independently associated with AMD.58, 59 CFI is a serine protease that has a role in the complement pathway as it cleaves and inactivates C4b and C3b.
Genetic evidence from GWAS as well as from common and rare variant analyses show the engagement of mainly the alternative complement pathway in AMD pathogenesis.60 However, there is a suggestion that the classical pathway may be important as well: an inverse relationship between AMD and a non-coding variant in intron 6 of the classical pathway gene SERPING1 (C1 inhibitor) was reported in two cohorts.61 This protective effect was not replicated in another two independent studies62, 63 but SERPING1 was again shown to have a modest effect on the risk of nAMD in a study by Lee et al.64 A recent study and meta-analysis suggested that the SERPING1 is not a major genetic component of AMD in East Asians but is a genetic risk factor for AMD in Caucasians, providing evidence for ethnic diversity in the genetic etiology of AMD.65
Table 1 displays the most common complement pathway biomarkers that have been investigated for an association with the pathogenesis of AMD. Evidence for and against the association are also displayed.
Intraocular vs systemic complement activity
Most complement components and many circulating complement regulatory proteins are synthesized primarily by liver hepatocytes and then released into the bloodstream.11 However, in some tissues with limited access to circulating plasma proteins such as the brain, an extrahepatic system of complement biosynthesis also exists.84, 85, 86
According to Anderson et al, for the alternative pathway-related genes, differential expression in adult liver relative to the other cells and tissues was not as striking as it was for the classical pathway-related genes.11 Expression of the alternative pathway inhibitors was also widespread in the various tissues/cells examined, but somewhat less prevalent in adult liver. Analysis of neural retina, RPE, and choroid isolates indicated that choroidal cells are the predominant local source of most alternative pathway components and regulators. For those complement-related genes that showed relatively high transcription levels in the neural retina, RPE, and/or choroid, they localized some of the corresponding proteins to specific cells and extracellular compartments within these tissues. A number of tissues including lung, RPE–choroid, and vein showed significant expression of the shared complement component C3. C3 levels in RPE–choroid were ~5% of those measured in adult liver. These findings were consistent with previous reports, most notably in the kidney,87 showing that at least 10% of the circulating pool of C3 cannot be attributed to hepatic synthesis. C3 expression in the neural retina was 16-fold lower than in the RPE–choroid.
Khandahdia et al showed that in liver transplant patients, AMD was associated with recipient rather than donor CFH Y402H genotype.88 Results by Khandhadia et al suggest that local intraocular complement activity in the eye may be more important in AMD pathogenesis and that any therapeutic intervention will thus need to be given intraocularly. This hypothesis was supported by results of the study by Bomback et al. They reported that intravenous administration of eculizumab (a monoclonal antibody that binds complement C5) over 12 months had no effect on retinal drusen in two patients with C3 glomerulopathy.89
On the contrary, Scholl et al performed a comprehensive investigation of the alternative pathway of complement protein plasma concentrations in a cohort of AMD patients and controls and correlated their findings with polymorphisms in the CFH, BF-C2, and C3 genes. They showed that several parameters that reflect systemic complement activation were significantly elevated in the circulation of AMD patients as compared with controls. Moreover, the discriminatory ability of complement proteins appeared superior or at least similar to the discriminatory ability of genetic markers of complement genes for the prediction of AMD.90
It is not yet clear whether AMD is a systemic disease with local disease manifestation at the aging macula or an intraocular disease where local complement activity is more important in its pathogenesis. This is worth investigating further.
Further comparisons between isolated preparations of RPE, choroid, and neural retina reveal that the predominant cellular source(s) for most classical and alternative pathway gene expression, including the shared C3 component, resides in the choroid rather than in the RPE or neural retina. In short, the results indicate that cells in the choroid have the capacity to synthesize an extensive array of classical and alternative activation pathway components and regulatory molecules, most of which are apparently not produced by cells in the RPE or neural retina.11
Such studies suggest that the choroid may be the target of choice for the development of new therapeutic agents to treat AMD, uveitis, and other posterior segment diseases with an inflammatory component.
Drug response related to complement pathway mechanisms
Genetic variation and anti-VEGF treatment
Approximately 1800 patients were treated for nAMD with anti-VEGF drugs in the CATT and the IVAN trials. Phenotypic data were collected in a rigorous manner in these study populations. This made these patients ideal for evaluating the effects of a number of genetic polymorphisms on treatment response to anti-VEGF therapy in nAMD.
In the CATT study, a pharmacogenetic relationship was tested between response to treatment and SNPs rs1061170 (CFH Y402H), rs10490924 (ARMS2 A69S), rs11200638 (HTRA1 promoter), and rs2230199 (C3 R80G) as these four SNPs had consistently been shown to have the strongest associations with the development and progression of AMD and have been postulated to influence the response to therapy.91 CFH and C3 encode genes involved in the complement cascade. Clinical measures of the response to treatment were based on visual acuity, anatomical features of AMD assessed by OCT and FA, and the total number of injections given in 1 year. For each of the three visual measures and for each of the five anatomic outcomes evaluated there was no association between genotype and either mean change in VA or mean change in total foveal thickness from baseline. Among the participants in the two PRN groups, no statistically significant difference was found in the number of injections among the different genotypes for any of the four SNPs, or for the total number of risk alleles. There were two instances where borderline significance was present. First, better visual acuity was seen in patients who were homozygous for the risk allele at C3 (P=0.03), which is the opposite of what would be expected. Second, the lowest mean change in total foveal thickness (less clinical response) was seen in patients who were homozygous for the CFH risk allele (P=0.03). However, patients who were heterozygous for the CFH risk allele had the highest mean change in total foveal thickness (best clinical response), which would again not be expected if the presence of the risk allele truly influences clinical response. Overall, according to the CATT trial, there is little biological evidence to support that the complement pathway, or at least these SNPs in the complement pathway, strongly influence the response to therapy.
In the IVAN trial,92 Lotery et al tested for replication of the three previously reported pharmacogenetic associations of response to VEGF inhibition in nAMD at the CFH, FZD4, and HTRA1/ARMS2 loci93, 94 as well as an additional 482 SNPs for pharmacogenetic associations using a candidate gene approach. They defined responder status based on the OCT metric of total retinal thickness (TRT) and they computed the change in TRT from baseline to the latest time point for which OCT data were available (3, 6, 9, or 12 months). None of the three SNPs previously associated with the CFH, FZD4, and HTRA1/ARMS2 genes were found to be significantly associated with responder status in this cohort. None of the associations between SNP and responder status for the remaining 482 SNPs was statistically significant.
CFH polymorphisms and anti-VEGF treatment
Chen et al performed a literature-based meta-analysis including 10 published association studies involving 1510 patients to investigate the association between polymorphism rs1061170 (T1277C, Y402H) of the CFH gene and treatment response of nAMD.95 They identified 10 eligible studies for their systematic review. Their results showed that polymorphism rs1061170 was a predictor of treatment response of nAMD, especially for anti-VEGF agents. Individuals homozygous for the variant risk C-allele showed a decreased response to treatment by ~1.6-fold when compared with patients homozygous for the ancestral T allele. When they divided the patients according to ethnicity (Caucasians or not), they found that CC genotype was associated with a reduced response to treatment of nAMD with an OR of 1.73 (95% CI, 1.05–2.86) in Caucasians. As only one study performed in Asians was reported and included in the meta-analysis, they could not conduct a sub-meta-analysis in Asians. Further validation in larger studies is needed of course, but this was, to the best of our knowledge, the first meta-analysis confirming a genetic marker predictive for AMD treatment response.
Lee et al collected mouthwash samples for genotyping from 178 patients with a diagnosis of exudative AMD who were undergoing treatment for an active neovascular lesion with intravitreal ranibizumab.96 Genomic DNA was prepared from buccal cells and genotyping for a SNP in the CFH gene (Y402H, rs1061170 T/C) was performed. The association between genotype and post-treatment visual acuities were assessed using two generalized linear modeling techniques at 6 and 9 months separately. For the CFH Y402H polymorphism, 37 patients (24%) were TT, 71 (45%) were TC, and 48 (31%) were CC. The prevalence of the C risk allele was 54%. The CFH genotypes were not found to significantly affect the post-treatment VA at 6 months (P=0.38) or 9 months (P=0.70). However, when the mean number of injections over a 9-month period was examined, they did observe a trend in the number of injections required over a 9-month period among the three genotypes, with the TT group receiving the fewest injections (P=0.09), and that patients homozygous for the variant genotype for CFH (CC) were more likely to require reinjection. They found a stepwise increase in risk of additional injections, as patients with the TC genotype had a 25% increased risk (P=0.12), and patients with the CC genotype had a 37% statistically significant higher risk (P=0.04), suggesting a possible genotype dose-dependent pharamacogenetic effect.
McKibbin et al identified preliminary evidence of associations between visual acuity outcome after 6 months of intravitreal ranibizumab and polymorphisms in the CFH, VEGF, and HTRA1 genes. In their study, they did not find an association between CFH genotype and the number of injections in the first 6 months, but they did find a trend toward a better visual acuity response with the higher risk TC or CC genotypes. A gain of >5 ETDRS letters was seen in 34.6, 56.6, and 56% of eyes with the TT, TC, and CC genotypes (P=0.04, 0.4, and 0.06 for TC, CC, or combined TC or CC genotypes compared with TT).97
Findings by Smailhodzic et al suggest an additive effect of high-risk alleles in CFH, ARMS2, and VEGFA, leading to a younger age of nAMD onset in combination with poor response to intravitreal ranibizumab treatment. After ranibizumab treatment, patients with 6 high-risk alleles demonstrated a mean VA loss of 10 ETDRS letters (P<0.0001).98
Brantley et al collected mouthwash samples for genotyping from 86 Caucasian patients diagnosed with exudative AMD who were undergoing treatment with intravitreal bevacizumab.99 Genomic DNA was prepared from buccal cells and genotyping for CFH Y402H and LOC387715 A69S was performed. They identified a significant association between the CFH Y402H genotype and response to the treatment with bevacizumab: post-bevacizumab VA was significantly worse in patients with the CFH CC genotype compared with VA for the CFH TT and CFH TC genotype (P=0.016). Conversely, presence of the LOC387715 TT genotype had no significant effect on the response to treatment with bevacizumab.
Nischler et al included 197 patients with exudative AMD in a prospective study in which patients were treated with 1.25 mg intravitreal bevacizumab at 6-week intervals until CNV was no longer active.100 SNP genotyping was performed using restriction fragment length polymorphism analysis of PCR products. Their results showed that the CFH402HH genotype correlates with lower visual acuity outcome after treatment with bevacizumab. They observed a significant worse outcome for distance and reading visual acuity in the CFH402HH genotype group (P=0.042; statistical power=88% and P=0.0039; statistical power=78%)
Despite the number of studies that did detect a statistically significant association between certain genetic variants and response to anti-VEGF treatment, the CATT trial in the US and the IVAN trial in the UK were the ones with the most rigorous follow-up and phenotyping and their outcomes did not identify any clear pharmacogenetic associations. If a pharmacogenetic association does exist, it may require much larger sample sizes to detect.
CFH polymorphisms and nutritional supplements
Klein et al were the first ones that showed a potential pharmacogenetic interaction between variations in the Complement Factor H gene (CFH) and zinc therapy on the progression of AMD.101 A significant interaction was found between the high-risk genotype (CC) for CFH Y402H and supplementation with a combination of zinc and antioxidants vs placebo (P=0.03), but not with the zinc only or the antioxidants only groups. When the genotypes of CFH Y402H were examined for zinc (zinc only combined with the zinc and antioxidants group) vs no zinc (antioxidants only combined with the placebo group), a significant interaction was found with the homozygous high-risk genotype (CC) compared with the homozygous low-risk (TT) variant (P=0.004). Specifically, when receiving zinc therapy, a 5% reduction in AMD progression was seen in the CC group, compared with a 22% reduction in AMD progression in the TT group.
The AREDS showed that antioxidants and zinc reduce progression rates of moderate to advanced AMD.102 Awh et al, in their pharmacogenetic analysis of the AREDS patients,103 performed genotyping of all AREDS white patients with category 3 disease in at least one eye (intermediate AMD, at least one drusen >125 μm, extensive intermediate drusen or GA not involving the center of the macula). Among the genetic risk predictors for AMD that they selected, there was a set of five common CFH polymorphisms: rs1048663, rs3766405, rs412852, rs11582939, and rs1066420, as well as the 372_815de1443ins54 ARMS2 marker. Their data supported a deleterious interaction between CFH risk alleles and high-dose zinc supplementation, suggesting that individuals with one or two CFH risk alleles and <2 ARMS2 alleles would benefit maximally from supplementation with antioxidants only, because they also found that the beneficial effect of antioxidants completely disappears in the presence of two ARMS2 alleles. This allowed the identification of subgroups, who would benefit more than the average AMD patient from nutritional treatment. These findings were consistent with current understanding of how CFH interacts with zinc. Zinc binds CFH, inducing multimeric large forms that lose complement component 3b inhibitory activity as a function of zinc concentration.104 Decreased targeting of CFH protein to sites of active complement activation as a functional consequence of CFH risk genotypes, may thus be exacerbated through zinc supplementation.105, 106
However recently, Chew et al used statistical models, adjusted for age, gender, smoking status, and baseline AMD severity, to examine the influence of genotypes on the response to therapy with four randomly assigned arms of AREDS supplement components: placebo, antioxidants (vitamin C, vitamin E, β-carotene), zinc, or a combination. They analyzed the influence of CFH RS1061170 and rs1410996 combined with ARMS2 rs10490924 and the combination of CFH rs412852 and rs3766405 with ARMS2 c.372_815del443ins54 on progression to late AMD and they found no statistically significant difference for the benefits of AREDS supplements among different genotype groups.107
As demonstrated above, associations between anti-VEGF therapy or nutritional supplements and genotypes vary markedly between different studies. This may be because study designs are flawed, phenotypes are imprecise or the associations are actually false. Therefore replication of such results in independent cohorts is essential in order to confirm the validity of such correlations.
Dry AMD potential treatments
Dry AMD emerging treatments, in addition to stem cell–based treatment, lasers (micropulse), implantable miniature telescopes and low vision rehabilitation, have basically focused on two strategies: prevention of photoreceptor and RPE cell loss, and suppression of inflammation. The former may be achieved by neuroprotection induction, oxidative damage prevention, and visual cycle modification.108
Potential therapies that decrease inflammation and oxidative stress include the AREDS vitamins, complement inhibitors, steroids (fluocinolone acetate), OT-551, prostaglandins, and hydroxychloroquine.109
A randomized, placebo controlled, clinical trial of high dose supplementation of vitamins C, E, beta-carotene, zinc, and copper was the first effective treatment to slow the progression of the disease for patients at high risk for developing advanced AMD as oxidative stress and depletion of essential micronutrients are important factors for AMD progression.101 In 2006, the same research group began a second study called AREDS2 to determine whether they could improve the AREDS formulation.
In this study, which was completed in 2013, they tried adding omega-3 fatty acids, as well as the antioxidants lutein and zeaxanthin, which are in the same family of nutrients as beta-carotene. The researchers also tried substituting lutein and zeaxanthin for beta-carotene, which prior studies had associated with an increased risk of lung cancer in smokers. The study found that while omega-3 fatty acids had no effect on the formulation, lutein, and zeaxanthin together appeared to be a safe and effective alternative to beta-carotene.110
Neuroprotective drugs aim to preserve macular function by preventing apoptosis of viable RPE cells and photoreceptors. The main drugs under investigation have been: Ciliary neurotrophic factor (NT-501, Neurotech Pharmaceuticals, Cumberland, RI, USA),111 brimonidine tartrate (Allergan, Inc., Irvine, CA, USA),112 tandospirone (Alcon Laboratories, Inc., Fort Worth, TX, USA),113 anti-amyloid β antibodies (Glatiramer acetate, Copaxone; Teva Pharmaceutical, Petah Tikva, Israel and RN6G, Pfizer Inc., New York, NY, USA)114, 115 and doxycycline.116
Visual cycle modifiers include ACU-4429,117 fenretidine, and anti-amyloid b antibodies. 118, 119
Therapies that increase oxygenation and affect blood flow include rheopheresis,120, 121, 122 ozonated autohemotherapy,123 and vasodilators.124, 125
Therapies that are currently in clinical trials include brimonidine, doxycycline, anti-amyloid antibodies (GSK933776 and RN6G), RPE65 inhibitor (ACU-4429, Acucela Inc., Seattle, WA, USA), complement inhibitors (ARC1905, FCFD4514S), hydroxychloroquine, intravitreal fluocinolone acetate, and vasodilators like sildenafil, moxaverine, and MC-1101.106 Therapies that have not been shown to be effective include POT-4, eculizumab, tandospirone, anecortave acetate, the antioxidant OT-551, sirolimus, and vitamin E.109
Complement-based treatments
Complement-based treatments are optimized to specific components of the pathway and differ in their mechanism of action, facilitating inhibition, replacement, or modulation of their target. They must also regulate complement activity without adversely affecting defence and immunomodulatory function of the cell. In contrast to the anti-VEGF agents that form the mainstay of conventional treatment, as complement-based therapeutics have the potential to intervene earlier in the disease process, perhaps even before an AMD phenotype is distinguishable.126
POT-4 (Potentia Pharmaceuticals, Crestwood, KY, USA) is a synthetic peptide that reversibly binds complement factor C3 and inhibits activation of the complement cascade. Inhibition of C3 shuts down all downstream complement activation that could otherwise lead to local inflammation, tissue damage, and upregulation of angiogenic factors. As with VEGF inhibitors, POT-4 may be administered intravitreally, limiting possible unwanted systemic effects. At higher dosages, an intravitreal gel forms creating a drug depot, with the potential to sustain therapeutic levels of the compound within the eye for several months following a single injection. (ClinicalTrials.gov number, NCT00473928).
ARC1905 is an aptamer-based C5 inhibitor, blocking the cleavage of C5 into C5a and C5b fragments. Nucleic acid aptamers are synthetically derived and demonstrate desirable therapeutic properties largely owing to their three-dimensional structure; namely high target specificity and binding affinity. It has been tested for both dry and nAMD (being tested in combination with ranibizumab for the latter; ClinicalTrials.gov number,NCT 00950638).
Eculizumab (Soliris), like ARC1905, is another antibody-based complement inhibitor. Eculizumab binds complement component C5, preventing cleavage, downstream activation, and the formation of MAC. The drug is administered intravenously over 6 months; weekly dosing during the initial induction period followed by two weekly maintenance doses. (ClinicalTrials.gov number, NCT00935883).
C5a, a product of proteolytic cleavage of C5 in the complement pathway, has been observed to have potent proinflammatory properties in its own right. Compared with complement component inhibitors that prevent C5a formation, receptor antagonists competitively bind to the C5a receptor neutralizing interaction. JSM-7717 and JPE-137539 are two peptidomimetic C5a receptor antagonists currently in preclinical assessment for AMD.127
Lampalizumab or anti-factor D is an antigen-binding fragment (Fab) of a humanized, monoclonal antibody directed against CFD. CFD is a rate-limiting enzyme involved in the activation of the alternative complement pathway. In the phase 2 MAHALO study, a reduction in disease progression was observed in patients with GA treated with lampalizumab.128 The MAHALO results also suggest that a CFI biomarker is prognostic for GA progression and predictive of lampalizumab treatment response; 57% of the samples selected in this study were positive for the CFI biomarker. In patients with AMD with GA, the complement inhibitor lampalizumab reduced disease progression by 20% and by 44% in the CFI biomarker-defined subset. This biomarker was identified by the International AMD Gene Consortium. Arguable it is the most effective example to date of a useful biomarker in an AMD treatment trial.129
Comments/conclusions
There is strong evidence that genetic variations in genes that regulate the alternative complement pathway are associated with an increased risk of developing AMD. However, the role of complement in the manifestation of the more advanced forms of the disease, particularly GA and CNV, is still unclear.
Clinical presentation of neovascular membranes in advanced wet AMD represents only the final stage of a complex cascade of events and therefore monotherapies, which are increasingly utilized to manage neovascular membranes, offer limited treatment options to patients.130 Recent clinical trials support this view. Combination therapy with anti-VEGF and anti-PDGF antibodies demonstrated improved visual acuity outcomes cf. monotherapy.131
Differences in individual patients’ responses to anti-VEGF treatment and possible correlations between this and SNPs of several genes, as well as the impact of pro-angiogenic mechanisms implicated in the pathogenesis of the disease, suggest that the complex cascade of events, which lead to the development of advanced AMD, can be modulated at different steps of the pathogenetic process. Perhaps, clinical drug resistance could be reasonably determined by upregulation of pro-angiogenic factors other than VEGFA.
As the authors of the results of the IVAN trial noted, there is no consensus of what constitutes response to treatment vs non-response. Correlations between vision and retinal morphologic features are modest at best, even when using OCT parameters as the metric of choice.92 Conversely, visual acuity may improve despite absence of morphologic change. Thus, using it as a marker of treatment responsiveness can lead to erroneous classifications. VA improvement is maximal after three injections and pharmacogenetic studies that were statistically significant used this as a primary outcome in contrast to the CATT and IVAN trials.
Even if new therapeutics or diagnostics could be easily and efficiently constructed, based on the knowledge of disease-associated genetic variations, these therapeutics and diagnostics would still need to be tested for their safety and efficacy, and these often come at great expense and over long periods of time, thereby making it unclear what immediate clinical benefits genetic association study results might have. Simon and Maitournam have already proposed the use of genetic variations to restrict entry into clinical trials.132 Their motivation was to assess potential efficiency gains in clinical trials, limited to participants possessing a genetic profile that is known to respond better to the drug in question. Schork and Topol also showed, that the increase in the incidence of outcomes in trials restricted to individuals with specific genotypic profiles can result in substantial reductions in requisite sample sizes for such trials.133
If the results of the MAHALO study were confirmed in the phase III trials, they would highlight the potential of genotype-restricted sampling for trials in AMD. This would set an example of how such trials could be designed. This approach may lead to quicker development of novel treatments. It may also reduce the risk to patients by stratifying therapy more appropriately to those most likely to respond effectively. Such approaches are already being increasing adopted in other therapeutic areas such as oncology.134
In summary, the tremendous advancement of knowledge into the genetic basis of AMD is now starting to generate novel biomarkers for patients affected with AMD. These biomarkers are likely to become increasingly important in the management of patients in the future.
References
’Highlights of Prescribing Information (Macugen)’. Food and Drug Administration: 3–12. July 2007.
Rosenfeld PJ, Brown DM, Heier JS, Boyer DS, Kaiser PK, Chung CY et al. Ranibizumab for neovascular age-related macular degeneration. N Engl J Med 2006; 355: 1419–1431.
Rich RM, Rosenfeld PJ, Puliafito CA, Dubovy SR, Davis JL, Flynn HW Jr et al. Short-term safety and efficacy of intravitreal bevacizumab (Avastin) for neovascular age-related macular degeneration. Retina 2006; 26 (5): 495–511.
Ambati J, Ambati BK, Yoo SH, Ianchulev S, Adamis AP . Age-related macular degeneration:etiology, pathogenesis, and therapeutic strategies. Surv Ophthalmol 2003; 48 (3): 257–293.
van Leeuwen R, Klaver CC, Vingerling JR, Hofman A, de Jong PT . Epidemiology of age-related maculopathy: a review. Eur J Epidemiol 2003; 18 (9): 845–854.
Comparison of Age-related Macular Degeneration Treatments Trials (CATT) Research Group. Ranibizumab and bevacizumab for treatment of neovascular age-related macular degeneration: 2-year results. Ophthalmology 2012; 119 (7): 1388–1398.
Chakravarthy U, Harding SP, Rogers CA, Downes SM, Lotery AJ, Culliford LA et al. Alternative treatments to inhibit VEGF in age-related choroidal neovascularisation: 2-year findings of the IVAN randomised controlled trial. Lancet 2013; 382: 1258–1267.
Dunkelberger JR, Song WC . Complement and its role in innate and adaptive immune responses. Cell Research 2010; 20: 34–50.
Janeway Jr CA, Travers P, Walport M, Shlomchik M . Immunobiology: The Immune System in Health and Disease. Garland Publishing: NY, USA, 2005.
Volanakis JE, Frank MM . The Human Complement System in Health and Disease. Marcel Dekker Inc.: NY, USA, 1998.
Anderson DH, Radeke MJ, Gallo NB, Chapin EA, Johnson PT, Curletti CR et al. The pivotal role of the complement system in aging and age related macular degeneration: hypothesis re-visited. Prog Retin Eye Res 2010; 29 (2): 95–112.
Walport MJ . Complement. First of two parts. N Engl J Med 2001; 344: 1058–1066.
Walport MJ . Complement. Second of two parts. N Engl J Med 2001; 344: 1140–1144.
Ross RJ, Bojanowski CM, Wang JJ, Chew EY, Rochtchina E, Ferris FL III et al. The LOC387715 polymorphism and age-related macular degeneration: replication in three case-control samples. Invest Ophthalmol Vis Sci 2007; 48: 1128–1132.
Patel M, Chan C . Immunopathological aspects of age-related macular Degeneration. Semin Immunopathol 2008; 30 (2): 97–110.
The AMD Gene Consortium. Seven new loci associated with age-related macular degeneration. Nat Genet 2013; 45: 433–439e2.
Skol AD, Scott LJ, Abecasis GR, Boehnke M . Joint analysis is more efficient than replication based analysis for two-stage genome-wide association studies. Nat Genet 2006; 38: 209–213.
Mullins RF, Hageman GS . Histochemical comparison of ocular ’drusen’ in monkey and human. In MH LaVail JG, Anderson RE Degenerative Retinal Diseases. Plenum Press: NY, USA, 1997; 1–10.
Hageman GS, Mullins RF . Molecular composition of drusen as related to substructural phenotype. Mol Vis 1999; 5: 28.
Anderson DH, Mullins RF, Hageman GS, Johnson LV . A role for local inflammation in the formation of drusen in the aging eye. Am J Ophthalmol 2002; 134: 411–431.
Hageman GS, Luthert PJ, Victor Chong NH, Johnson LV, Anderson DH, Mullins RF . An integrated hypothesis that considers drusen as biomarkers of immune-mediated processes at the rpe-bruch's membrane interface in aging and age-related macular degeneration. Prog Retin Eye Res 2001; 20: 705–732.
Johnson LV, Leitner WP, Staples MK, Anderson DH . Complement activation and inflammatory processes in drusen formation and age related macular degeneration. Exp Eye Res 2001; 73: 887–896.
Dastgheib K, Green WR . Granulomatous reaction to Bruch's membrane in age-related macular degeneration. Arch Ophthalmol 1994; 112: 813–818.
Grossniklaus HE, Ling JX, Wallace TM, Dithmar S, Lawson DH, Cohen C et al. Macrophage and retinal pigment epithelium expression of angiogenic cytokines in choroidal neovascularization. Mol Vis 2002; 8: 119–126.
Penfold PL, Madigan MC, Gillies MC, Provis JM . Immunological and aetiological aspects of macular degeneration. Prog Retin Eye Res 2001; 20: 385–414.
Lopez PF, Grossniklaus HE, Lambert HM, Aaberg TM, Capone Jr A, Sternberg P Jr et al. Pathologic features of surgically excised subretinal neovascular membranes in age-related macular degeneration. Am J Ophthalmol 1991; 112: 647–656.
Kamei M, Yoneda K, Kume N, Suzuki M, Itabe H, Matsuda K et al. Scavenger receptors for oxidized lipoprotein in age-related macular degeneration. Invest Ophthalmol Vis Sci 2007; 48: 1801–1807.
Suzuki M, Kamei M, Itabe H, Yoneda K, Bando H, Kume N et al. Oxidized phospholipids in the macula increase with age and in eyes with age-related macular degeneration. Mol Vis 2007; 13: 772–778.
Klein RJ, Zeiss C, Chew EY, Tsai JY, Sackler RS, Haynes C et al. Complement factor H polymorphism in age-related macular degeneration. Science 2005; 308: 385–389.
Hageman GS, Anderson DH, Johnson LV, Hancox LS, Taiber AJ, Hardisty LI et al. A common haplotype in the complement regulatory gene factor H (HF1/CFH) predisposes individuals to age-related macular degeneration. Proc Natl Acad Sci USA 2005; 102: 7227–7232.
Haines JL, Hauser MA, Schmidt S, Scott WK, Olson LM, Gallins P et al. Complement factor H variant increases the risk of age-related macular degeneration. Science 2005; 308: 419–421.
Edwards AO, Ritter R III, Abel KJ, Manning A, Panhuysen C, Farrer LA . Complement factor H polymorphism and age-related macular degeneration. Science 2005; 308: 421–424.
Skerka C, Lauer N, Weinberger AA, Keilhauer CN, Suhnel J, Smith R et al. Defective complement control of factor H (Y402H) and FHL-1 in age-related macular degeneration. Mol Immunol 2007; 44: 3398–3406.
Laine M, Jarva H, Seitsonen S, Haapasalo K, Lehtinen MJ, Lindeman N et al. Y402H polymorphism of complement factor H affects binding affinity to C-reactive protein. J Immunol 2007; 178: 3831–3836.
Boekhoorn SS, Vingerling JR, Witteman JC, Hofman A, de Jong PT . C-reactive protein level and risk of aging macula disorder: the Rotterdam study. Arch Ophthalmol 2007; 125: 1396–1401.
Zhou J, Jang YP, Kim SR, Sparrow JR . Complement activation by photooxidation products of A2E, a lipofuscin constituent of the retinal pigment epithelium. Proc Natl Acad Sci USA 2006; 103: 16182–16187.
Nozaki M, Raisler BJ, Sakurai E, Sarma JV, Barnum SR, Lambris JD et al. Drusen complement components C3a and C5a promote choroidal neovascularization. Proc Natl Acad Sci USA 2006; 103: 2328–2333.
Bora PS, Sohn JH, Cruz JM, Jha P, Nishihori H, Wang Y et al. Role of complement and complement membrane attack complex in laser-induced choroidal neovascularization. J Immunol 2005; 174: 491–497.
Mantovani A, Sica A, Sozzani S, Allavena P, Vecchi A, Locati M . The chemokine system in diverse forms of macrophage activation and polarization. Trends Immunol 2004; 25: 677–686.
Giannakis E, Jokiranta TS, Male DA, Ranganathan S, Ormsby RJ, Fischetti VA et al. A common site within factor H SCR 7 responsible for binding heparin, C-reactive protein and streptococcal M protein. Eur J Immunol 2003; 33: 962–969.
Clark SJ, Perveen R, Hakobyan S, Morgan BP, Sim RB, Bishop PN et al. Impaired Binding of the Age-related Macular Degeneration-associated Complement Factor H 402H Allotype to Bruch's Membrane in Human Retina. J Biol Chem 2010; 285 (39): 30192–30202.
Johnson PT, Betts KE, Radeke MJ, Hageman GS, Anderson DH, Johnson LV . Individuals homozygous for the age-related macular degeneration risk-conferring variant of complement factor H have elevated levels of CRP in the choroid. Proc Natl Acad Sci USA 2006; 103: 17456–17461.
Seddon JM, Gensler G, Milton RC, Klein ML, Rifai N . Association between C-reactive protein and age-related macular degeneration. JAMA 2004; 291: 704–710.
Thakkinstian A, Han P, McEvoy M, Smith W, Hoh J, Magnusson K et al. Systematic review and meta-analysis of the association between complement H Y402H polymorphisms and age-related macular degeneration. Hum Mol Genet 2006; 15: 2784–2790.
Gold B, Merriam JE, Zernant J, Hancox LS, Taiber AJ, Gehrs K et al. Variation in factor B (BF) and complement component 2 (C2) genes is associated with age-related macular degeneration. Nat Genet 2006; 38: 458–462.
Jakobsdottir J, Conley YP, Weeks DE, Ferrell RE, Gorin MB . C2 and CFB genes in age-related maculopathy and joint action with CFH and LOC387715 genes. PLoS One 2008; 3: e2199.
Despriet DD, van Duijn CM, Oostra BA, Uitterlinden AG, Hofman A, Wright AF et al. Complement component C3 and risk of age-related macular degeneration. Ophthalmology 2009; 116: 474–480.
Maller JB, Fagerness JA, Reynolds RC, Neale BM, Daly MJ, Seddon JM . Variation in complement factor 3 is associated with risk of age-related macular degeneration. Nat Genet 2007; 39: 1200–1201.
Park KH, Fridley BL, Ryu E, Tosakulwong N, Edwards AO . Complement component 3 (C3) haplotypes and risk of advanced age-related macular degeneration. Invest Ophthalmol Vis Sci 2009a; 50: 3386–3393.
Yates JR, Sepp T, Matharu BK, Khan JC, Thurlby DA, Shahid H et al. Complement C3 variant and the risk of age-related macular degeneration. N Engl J Med 2007; 357: 553–561.
Rogers J, Cooper NR, Webster S, Schultz J, McGeer PL, Styren SD et al. Complement activation by beta-amyloid in Alzheimer disease. Proc Natl Acad Sci USA 1992; 89: 10016–10020.
Johnson LV, Leitner WP, Rivest AJ, Staples MK, Radeke MJ, Anderson DH . The Alzheimer's A beta-peptide is deposited at sites of complement activation in pathologic deposits associated with aging and age-related macular degeneration. Proc Natl Acad Sci USA 2002; 99: 11830–11835.
Fett AL, Hermann MM, Muether PS, Kirchhof B, Fauser S . ‘Immunohistochemical localization of complement regulatory proteins in the human retina’. Histol Histopathol 2012; 27: 357–364.
Sivaprasad S, Adewoyin T, Bailey TA, Dandekar SS, Jenkins S, Webster AR et al. ‘Estimation of systemic complement C3 activity in age-related macular degeneration’. Arch Ophthalmol 2007; 125: 515–519.
Scholl HP, Charbel IP, Walier M, Janzer S, Pollok-Kopp B, Börncke F et al. Systemic complement activation in age-related macular degeneration. PLoS One 2008; 3: e2593.
MacHali'nska A, Dziedziejko V, Mozolewska-Piotrowska K, Karczewicz D, Wiszniewska B, MacHali'nski B . Elevated plasma levels of c3a complement compound in the exudative form of age-related macular degeneration. Ophthalmic Res 2009; 42: 54–59.
Liu B, Wei L, Meyerle C, Tuo J, Sen HN, Li Z et al. Complement component C5a promotes expression of IL-22 and IL-17 from human T cells and its implication in age-related macular degeneration. J Transl Med 2011; 9: 1–12.
Ennis S, Gibson J, Cree AJ, Collins A, Lotery AJ . Support for the involvement of complement factor I in age-related macular degeneration. Eur J Hum Genet 2010; 18: 15–16.
Fagerness JA, Maller JB, Neale BM, Reynolds RC, Daly MJ, Seddon JM . Variation near complement factor I is associated with risk of advanced AMD. Eur J Hum Genet 2009; 17: 100–104.
Parmeggiani F, Sorrentino FS, Romano MR, Costagliola C, Semeraro F, Incorvaia C et al. Mechanism of inflammation in age-related macular degeneration: an up-to-date on genetic landmarks. Mediators Inflamm 2013; 2013: 435607.
Ennis S, Jomary C, Mullins R, Cree A, Chen X, Macleod A et al. Association between the SERPING1 gene and age-related macular degeneration: a two-stage case control study. Lancet 2008; 372: 1828–1834.
Allikmets R, Dean M, Hageman GS, Baird PN, Klaver CC, Bergen AA et al. The SERPING1 gene and age-related macular degeneration. Lancet 2009; 374: 875–876.
Park KH, Ryu E, Tosakulwong N, Wu Y, Edwards AO . Common variation in the SERPING1 gene is not associated with age-related macular degeneration in two independent groups of subjects. Mol Vis 2009b; 15: 200–207.
Lee AY, Kulkarni M, Fang AM, Edelstein S, Osborn MP, Brantley MA Jr . Association between SERPING1 rs2511989 polymorphism and age-related macular degeneration: meta-analysis. Br J Ophthalmol 2010; 94: 915–917.
Liu K, Lai TY, Ma L, Lai FH, Young AL, Brelen ME et al. Ethnic differences in the association of SERPING1 with age related macular degeneration and polypoidal choroidal vasculopathy. Sci Rep 2015; 5: 9424.
Edwards AO, Ritter R 3rd, Abel KJ, Manning A, Panhuysen C, Farrer LA . Complement factor H polymorphism and age-related macular degeneration. Science 2005; 308: 421–424.
Hageman GS, Anderson DH, Johnson LV, Hancox LS, Taiber AJ, Hardisty LI et al. A common haplotype in the complement regulatory gene factor H (HF1/CFH) predisposes individuals to age-related macular degeneration. Proc Natl Acad Sci USA 2005; 102: 7227–7232.
Li M, Atmaca-Sonmez P, Othman M, Branham KEH, Khanna R, Wade MS et al. CFH haplotypes without the Y402H coding variant show strong association with susceptibility to age-related macular degeneration. Nat Genet 2006; 38: 1049–1054.
Zareparsi S, Branham KEH, Li M, Shah S, Klein RJ, Ott J et al. Strong association of the Y402H variant in complement factor H at 1q32 with susceptibility to age-related macular degeneration. Am J Hum Genet 2005; 77: 149–153.
Clark SJ, Higman VA, Mulloy B, Perkins SJ, Lea SM, Sim RB et al. His-384 allotypic variant of factor H associated with age-related macular degeneration has different heparin binding properties from the non-disease-associated form. J Biol Chem 2006; 281: 24713–24720.
Lauer N, Mihlan M, Hartmann A, Schlotzer-Schrehardt U, Keilhauer C, Scholl HP et al. Complement regulation at necrotic cell lesions is impaired by the age-related macular degeneration-associated factor-H His402 risk allele. J Immun 2011; 187: 4374–4383.
Wegscheider BJ, Weger M, Renner W, Steinbrugger I, Marz W, Mossbock G et al. Association of complement factor H Y402H gene polymorphism with different subtypes of exudative age-related macular degeneration. Ophthalmology 2007; 114: 738–742.
Grassi MA, Folk JC, Scheetz TE, Taylor CM, Sheffield VC, Stone EM . Complement factor H polymorphism p.tyr402-to-his and cuticular drusen. Arch Ophthal 2007; 125: 93–97.
Scott WK, Schmidt S, Hauser MA, Gallins P, Schnetz-Boutaud N, Spencer KL et al. Independent effects of complement factor H Y402H polymorphism and cigarette smoking on risk of age-related macular degeneration. Ophthalmology 2007; 114: 1151–1156.
Bergeron-Sawitzke J, Gold B, Olsh A, Schlotterbeck S, Lemon K, Visvanathan K et al. Multilocus analysis of age-related macular degeneration. Eur J Hum Genet 2009; 17: 1190–1199.
Ho L, van Leeuwen R, Witteman JCM, van Duijn CM, Uitterlinden AG, Hofman A et al. Reducing the genetic risk of age-related macular degeneration with dietary antioxidants, zinc, and omega-3 fatty acids: the Rotterdam Study. Arch Ophthal 2011; 129: 758–766.
Weismann D, Hartvigsen K, Lauer N, Bennett KL, Scholl HPN, Issa PC et al. Complement factor H binds malondialdehyde epitopes and protects from oxidative stress. Nature 2011; 478: 76–81.
Gotoh N, Yamada R, Hiratani H, Renault V, Kuroiwa S, Monet M et al. No association between complement factor H gene polymorphism and exudative age-related macular degeneration in Japanese. Hum Genet 2006; 120: 139–143.
Tedeschi-Blok N, Buckley J, Varma R, Triche TJ, Hinton DR . Population-based study of early age-related macular degeneration: role of the complement factor H Y402H polymorphism in bilateral but not unilateral disease. Ophthalmology 2007; 114: 99–103.
Maller J, George S, Purcell S, Fagerness J, Altshuler D, Daly MJ et al. Common variation in three genes, including a noncoding variant in CFH, strongly influences risk of age-related macular degeneration. Nat Genet 2006; 38: 1055–1059.
Francis PJ, Hamon SC, Ott J, Weleber RG, Klein ML . ‘Polymorphisms in C2, CFB and C3 are associated with progression to advanced age related macular degeneration associated with visual loss’. J Med Genet 2009; 46: 300–307.
Heurich M, Martínez-Barricarte R, Francis NJ, Roberts DL, Rodríguez de Córdoba S, Morgan BP et al. ‘Common polymorphisms in C3, factor B, and factor H collaborate to determine systemic complement activity and disease risk’. Proc Natl Acad Sci USA 2011; 108: 8761–8766.
Wu L, Tao Q, Chen W, Wang Z, Song Y, Sheng S et al. ‘Association between polymorphisms of complement pathway genes and age-related macular degeneration in a Chinese population’. Invest Ophthalmol Vis Sci 2013; 54: 170–174.
Gasque P, Fontaine M, Morgan BP . Complement expression in human brain. Biosynthesis of terminal pathway components and regulators in human glial cells and cell lines. J Immunol 1995; 154: 4726–4733.
Johnson SA, Lampert-Etchells M, Pasinetti GM, Rozovsky I, Finch CE . Complement mRNA in the mammalian brain: responses to Alzheimer's disease and experimental brain lesioning. Neurobiol Aging 1992; 13: 641–648.
Walker DG, McGeer PL . Complement gene expression in human brain: comparison between normal and Alzheimer disease cases. Brain Res Mol Brain Res 1992; 14: 109–116.
Tang S, Zhou W, Sheerin NS, Vaughan RW, Sacks SH . Contribution of renal secreted complement C3 to the circulating pool in humans. J Immunol 1999; 162: 4336–4341.
Khandhadia S, Hakobyan S, Heng LZ, Gibson J, Adams DH, Alexander GJ et al. Age-related macular degeneration and modification of systemic complement factor H production through liver transplantation. Ophthalmology 2013; 120: 1612–1618.
Bomback AS, Smith RJ, Barile GR, Zhang Y, Heher EC, Herlitz L et al. Eculizumab for dense deposit disease and C3 glomerulonephritis. Clin J Am Soc Nephrol 2012; 7: 748–756.
Scholl HP, Charbel Issa P, Walier M, Janzer S, Pollok-Kopp B, Börncke F et al. Systemic complement activation in age-related macular degeneration. PLoS One 2008; 3 (7): e2593.
Hagstrom SA, Ying G, Pauer GJ, Sturgill-Short GM, Huang J, Callanan DG et al. Pharmacogenetics for genes associated with age-related macular degeneration (AMD) in the comparison of AMD treatments trials (CATT). Ophthalmology 2013; 120 (3): 593–599.
Lotery AJ, Gibson J, Cree AJ, Downes SM, Harding SP, Rogers CA et al. Pharmacogenetic associations with vascular endothelial growth factor inhibition in participants with neovascular age-related macular degeneration in the IVAN Study. Ophthalmology 2013; 120 (12): 2637–2643.
Kloeckener-Gruissem B, Barthelmes D, Labs S, Schindler C, Kurz-Levin M, Michels S et al. Genetic association with response to intravitreal ranibizumab in patients with neovascular AMD. Invest Ophthalmol Vis Sci 2011; 52: 4694–4702.
Teper SJ, Nowinska A, Pilat J, Palucha A, Wylegala E . Involvement of genetic factors in the response to a variable-dosing ranibizumab treatment regimen for age-related macular degeneration. Mol Vis 2010; 16: 2598–2604.
Chen H, Yu KD, Xu GZ . Association between variant Y402H in age-related macular degeneration (AMD) susceptibility gene CFH and treatment response of AMD. A meta-analysis. PLoS One 2012; 7: e42464.
Lee AY, Raya AK, Kymes SM, Shiels A, Brantley MA Jr . Pharmacogenetics of complement factor H (Y402H) and treatment of exudative age-related macular degeneration with ranibizumab. Br J Ophthalmol 2009; 93: 610–613.
McKibbin M, Ali M, Bansal S, Baxter D, West K, Williams G et al. CFH, VEGF and HTRA1 promoter genotype may influence the response to intravitreal ranibizumab therapy for neovascular age-related macular degeneration. Br J Ophthalmol 2012; 96: 208–212.
Smailhodzic D, Muether PS, Chen J, Kwestro A, Zhang AY, Omar A et al. Cumulative effect of risk alleles in CFH, ARMS2, and VEGFA on the response to ranibizumab treatment in age-related macular degeneration. Ophthalmology 2012; 119: 2304–2311.
Brantley Jr MA, Fang AM, King JM, Tewari A, Kymes SM, Shiels A . Association of complement factor H and LOC387715 genotypes with response of exudative age-related macular degeneration to intravitreal bevacizumab. Ophthalmology 2007; 114: 2168–2173.
Nischler C, Oberkofler H, Ortner C, Paikl D, Riha W, Lang N et al. Complement factor H Y402H gene polymorphism and response to intravitreal bevacizumab in exudative age-related macular degeneration. Acta Ophthalmol 2011; 89: e344–e349.
Klein ML, Francis PJ, Rosner B, Reynolds R, Hamon SC, Schultz DW et al. CFH and LOC387715/ARMS2 genotypes and treatment with antioxidants and zinc for age-related macular degeneration. Ophthalmology 2008; 115: 1019–1025.
Age-Related Eye Disease Study Research Group. A randomized, placebo-controlled, clinical trial of high-dose supplementation with vitamins C and E, beta carotene, and zinc for age-related macular degeneration and vision loss: AREDS report no. 8. Arch Ophthalmol 2001; 119: 1417–1436.
Awh CC, Lane AM, Hawken S, Zanken B, Kim IK . CFH and ARMS2 genetic polymorphisms predict response to antioxidants and zinc in patients with age-related macular degeneration. Ophthalmology 2013; 120: 2317–2323.
Nan R, Farabella I, Schumacher FF, Miller A, Gor J, Martin AC et al. Zinc binding to the Tyr402 and His402 allotypes of complement factor H: possible implications for age-related macular degeneration. J Mol Biol 2011; 408 (4): 714–735.
Okemefuna AI, Nan R, Miller A, Gor J, Perkins SJ . Complement factor H binds at two independent sites to C-reactive protein in acute phase concentrations. J Biol Chem 2010; 285: 1053–1065.
Bao B, Prasad AS, Beck FW, Fitzgerald JT, Snell D, Bao GW . Zinc decreases C-reactive protein, lipid peroxidation, and inflammatory cytokines in elderly subjects: a potential implication of zinc as an atheroprotective agent. Am J Clin Nutr 2010; 91: 1634–1641.
Chew EY, Klein ML, Clemons TE, Agrón E, Ratnapriya R, Edwards AO et al. No clinically significant association between CFH and ARMS2 genotypes and response to nutritional supplements: AREDS report number 38. Ophthalmology 2014; 121: 2173–2180.
Damico FM, Gasparin F, Scolari MR, Pedral LS, Takahashi BS . New approaches and potential treatments for dry age-related macular degeneration. Arq Bras Oftalmol 2012; 75: 71–76.
Leung E, Landa G . Update on current and future novel therapies for dry age-related macular degeneration. Expert Rev Clin Pharmacol 2013; 6 (5): 565–579.
Age-Related Eye Disease Study 2 Research Group. Lutein+zeaxanthin and omega-3 fatty acids for age-related macular degeneration: the Age-Related Eye DiseaseStudy 2 (AREDS2) randomized clinical trial. JAMA 2013; 309: 2005–2015.
Zhang K, Hopkins JJ, Heier JS, Birch DG, Halperin LS, Albini TA et al. Ciliary Neurotrophic factor delivered by encapsulated cell intraocular implants for treatment of geographic atrophy in age-related macular degeneration. Proc Natl Acad Sci USA 2011; 108: 6241–6245.
Woldemussie E, Wijono M, Pow D . Localization of alpha 2 receptors in ocular tissues. Vis Neurosci 2007; 24: 745–756.
Collier RJ, Wang Y, Smith SS, Martin E, Ornberg R, Rhoades K et al. Complement deposition and microglial activation in the outer retina in light-induced retinopathy: inhibition by a 5-HT1A agonist. Invest Ophthalmol Vis Sci 2011; 52 (11): 8108–8116.
Landa G, Rosen RB, Patel A, Lima VC, Tai KW, Perez VR et al. Qualitative spectral OCT/SLO analysis of drusen change in dry age-related macular degeneration patients treated with Copaxone. J Ocul Pharmacol Ther 2011; 27: 77–82.
Ding JD, Johnson LV, Herrmann R, Farsiu S, Smith SG, Groelle M et al. Anti-Amyloid therapy protects against retinal pigmented epithelium damage and vision loss in a model of age-related macular degeneration. Proc Natl Acad Sci USA 2011; 108: E279–E287.
Stieger K, Mendes-Madeira A, Meur GL, Weber M, Deschamps JY, Nivard D et al. Oral administration of doxycycline allows tight control of transgene expression: a key step towards gene therapy of retinal diseases. Gene Ther 2007; 14: 1668–1673.
Kubota R, Boman NL, David R, Mallikaarjun S, Patil S, Birch D . Safety and effect on rod function of ACU-4429, a novel small-molecule visual cycle modulator. Retina 2012; 32: 183–188.
Mata NL, Lichter JB, Vogel R, Han Y, Bui TV, Singerman LJ . Investigation of oral fenretinide for treatment of geographic atrophy in age-related macular degeneration. Retina 2013; 33: 498–507.
Dobri N, Qin Q, Kong J, Yamamoto K, Liu Z, Moiseyev G et al. A1120, a nonretinoid RBP4 antagonist, inhibits formation of cytotoxic bisretinoids in the animal model of enhanced retinal lipofuscinogenesis. Invest Ophthalmol Vis Sci 2013; 54: 85–95.
Pulido J, Sanders D, Winters JL, Klingel R . Clinical outcomes and mechanism of action for rheopheresis treatment of age-related macular degeneration. J Clin Apher 2005; 20: 185–194.
Pulido JS, Winters JL, Boyer D . Preliminary analysis of the final multicenter investigation of rheopheresis for age related macular degeneration (AMD) trial (MIRA-1) results. Trans Am Ophthalmol Soc 2006; 104: 221–231.
Koss MJ, Kurz P, Tsobanelis T, Lehmacher W, Fassbender C, Klingel R et al. Prospective, randomized, controlled clinical study evaluating the efficacy of Rheopheresis for dry age-relatedmacular degeneration. Dry AMD treatment with Rheopheresis Trial-ART. Graefes Arch Clin Exp Ophthalmol 2009; 247: 1297–1306.
Borrelli E, Diadori A, Zalaffi A, Bocci V . Effects of major ozonated autohemotherapy in the treatment of dry age related macular degeneration: a randomized controlled clinical study. Int J Ophthalmol 2012; 5: 708–713.
Birch DG, Toler SM, Swanson WH, Fish GE, Laties AM . A double-blind placebo-controlled evaluation of the acute effects of sildenafil citrate (Viagra) on visual function in subjects with early-stage age-related macular degeneration. Am J Ophthalmol 2002; 133: 665–672.
Pemp B, Garhofer G, Lasta M, Schmidl D, Wolzt M, Schmetterer L . The effects of moxaverine on ocular blood flow in patients with age-related macular degeneration or primary open angle glaucoma and in healthy control subjects. Acta Ophthalmol 2012; 90: 139–145.
Troutbeck R, Al-Qureshi S, Guymer RH . Therapeutic targeting of the complement system in age-related macular degeneration: a review. Clin Experiment Ophthalmol 2012; 40 (1): 18–26.
Schnatbaum K, Locardi E, Scharn D, Richter U, Hawlisch H, Knolle J et al. Peptidomimetic C5a receptor antagonists with hydrophobic substitutions at the C-terminus: increased receptor specificity and in vivo activity. Bioorg Med Chem Lett 2006; 16: 5088–5092.
Regillo CD Lampalizumab (anti-factor D) in patients with geography atrophy: the MAHALO phase 2 results. Paper presented at: the 2013 Annual Meeting of the American Academy of Ophthalmology; 2013; New Orleans, LA.
The AMD Gene Consortium. Seven new loci associated with age-related macular degeneration. Nat Genet 2013; 45 (4): 433–439 439e1-2.
Lazzeri S, Nardi M, Bocci G . Pharmacogenetic labyrinth of neovascular age-related macular degeneration therapy: how to escape and move forward? Pharmacogenomics 2013; 14: 1239–1242.
Tolentino MJ, Dennrick A, John E, Tolentino MS . Drugs in Phase II clinical trials for the treatment of age-related macular degeneration. Expert Opin Investig Drugs 2015; 24 (2): 183–199.
Maitournam A, Simon R . On the efficiency of targeted clinical trials. Stat Med 2005; 24 (3): 329–339.
Schork NJ, Topol EJ . Genotype-based risk and pharmacogenetic sampling in clinical trials. J Biopharm Stat 2010; 20: 315–333.
Berns K, Horlings HM, Hennessy BT, Madiredjo M, Marielle Hijmans E, Beelen K et al. A functional genetic approach identifies the PI3K Pathway as a major determinant of Trastuzumab resistance in Breast Cancer. Cancer Cell 2007; 12: 395–402.
Acknowledgements
We searched the NCBI databases for ‘complement factor pathway and age related macular degeneration’ and we found results in 17 of them for the term above. We focused on results found in PubMed (142 medical abstracts/citations) and OMIM (On line Mendelian Inheritance in Men, 19 results). Headlines used to locate related articles and restrict our search were ‘the role of complement pathway in the pathogenesis of age related macular degeneration’, ‘genetic variation and age related macular degeneration’, ‘CFH gene in age related macular degeneration’, ‘inflammation and neurodegenerative disease’, ‘pharmagenomics in AMD’. A manual search was also based on references from articles on the subjects above as well as review articles.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Rights and permissions
About this article
Cite this article
Gemenetzi, M., Lotery, A. Complement pathway biomarkers and age-related macular degeneration. Eye 30, 1–14 (2016). https://doi.org/10.1038/eye.2015.203
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/eye.2015.203
This article is cited by
-
A new era for giant cell arteritis
Eye (2020)
-
The role of hypoxia-inducible factors in neovascular age-related macular degeneration: a gene therapy perspective
Cellular and Molecular Life Sciences (2020)
-
Proteome and Secretome Dynamics of Human Retinal Pigment Epithelium in Response to Reactive Oxygen Species
Scientific Reports (2019)
-
Real-world Case Series of iStent or iStent inject Trabecular Micro-Bypass Stents Combined with Cataract Surgery
Ophthalmology and Therapy (2019)
-
Fluorescent silver nanoclusters as antibody label in a competitive immunoassay for the complement factor H
Microchimica Acta (2019)