Abstract
Purpose
To assess the effects of idiopathic epimacular membrane (IEMM) on retinal pigment epithelium (RPE), photoreceptor inner segment/outer segment (IS/OS) junction, and external limiting membrane (ELM) reflectivities to determine functional alterations in these layers using optical coherence tomography (OCT) image analysis.
Methods
Fifty eyes of 50 patients with untreated IEMM and 41 eyes of 41 age- and sex-matched healthy controls with normal OCT scans were retrospectively reviewed. A single masked physician analyzed OCT images randomly. Reflectivity values of RPE, IS/OS junction, and ELM were obtained using ‘plot profile’ mode of a medical image processing computer software.
Results
The study comprised 50 patients with untreated IEMM and age- and sex-matched 41 control subjects (P>0.05). Image analysis demonstrated that IS/OS junction and ELM had significantly lower reflectivity in patients with IEMM compared with those of the control eyes (P=0.008, P=0.009, respectively). However, RPE reflectivity did not differ between two groups (P=0.100). Correlation analyses showed no significant associations between reflectivity values and corrected visual acuity (P>0.05).
Conclusion
In patients with IEMM, photoreceptor IS/OS junction and ELM seem to have lower reflectivity, which might indicate impaired functionality even though these layers are not apparently damaged on OCT imaging.
Similar content being viewed by others
Introduction
Idiopathic epimacular membranes (IEMM) are avascular fibrocellular tissues characterized by distortion of macular surface, and history of predisposing ocular pathologies such as uveitis, retinal tear, retinal detachment, diabetic retinopathy, and retinal vascular occlusions are absent.1, 2, 3
Although pathogenesis of IEMM is still being investigated, studies have indicated that posterior vitreous detachment (PVD) has a critical role in the development of IEMM.3, 4 It was suggested that PVD causes breaks in internal limiting membrane (ILM) that lead to migration and proliferation of glial cells on retinal surface.3, 4 However, histopathologic specimens revealed complex nature of IEMM, which comprises glial cells, macrophages, retinal pigment epithelium (RPE) cells, fibrocytes, and myofibroblasts.2, 3
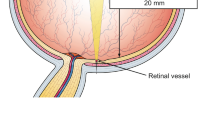
Clinical presentation of IEMM varies on the degree of deterioration in macular microarchitecture.5, 6 In clinical practice, dilated fundoscopic examination and optical coherence tomography (OCT) imaging are usually sufficient for the diagnosis. Furthermore, OCT allows the physician to follow-up changes in retinal microstructure, particularly integrity of photoreceptor inner segment/outer segment (IS/OS) junction, which was found associated with postoperative visual improvement.7, 8 Most of the studies concluded that an interrupted or absent IS/OS junction on OCT was significantly correlated with poor preoperative and postoperative visual acuity in patients with EMM.9, 10
In clinical practice, physicians are generally unable to detect functional loss in photoreceptors on OCT until IS/OS junction is obviously damaged. However, epimacular membrane might cause subclinical deteriorations in photoreceptor layer, and hence in IS/OS junction. In the current study, we aimed to assess the effects of IEMM on RPE, IS/OS junction, and external limiting membrane (ELM) reflectivities using a medical image processing computer software (ImageJ v. 1.47)11 to determine functional alterations in these layers, while there was no evident damage on OCT scans.
Materials and methods
Study group
Fifty eyes of 50 patients with untreated IEMM (patient group) and 41 eyes of 41 age- and sex-matched healthy subjects (control group) were included in this retrospective comparative study. Local ethics committee approved the study and tenets of the Declaration of Helsinki were followed. Inclusion criteria for the patient group were fundoscopic examination and OCT imaging consistent with IEMM. Eyes with disrupted or absent IS/OS junction on OCT images were not included into the study. Control group comprised subjects with normal ophthalmologic examination and OCT scan. Anterior segment features and intraocular pressure measurements were similar in the two groups. Patients with history of prior intraocular surgery other than uncomplicated cataract surgery, ocular trauma, inflammatory ocular diseases, retinal vascular occlusions, diabetic retinopathy, and retinal tear or detachment were excluded from the study.
Examinations
All patients underwent a complete ophthalmologic examination, including corrected distance visual acuity (CDVA) measurement with Snellen charts, slit-lamp biomicroscopic examination, applanation tonometry, and dilated fundoscopic examination (with +90 D lens). Log of the minimum angle of resolution (logMAR) equivalents were used to analyze visual acuity as offered by Holladay and Prager.12
Analysis of OCT images using ImageJ
OCT (Zeiss Cirrus HD-OCT 400; Carl Zeiss Meditec, Dublin, CA, USA) images were captured with proper quality using 6 mm × 6 mm macular cube 512 × 128 scanning mode by a single experienced technician (MA).
A total of 91 OCT images of 91 subjects (patient and control groups) and ophthalmologic examination records were retrospectively reviewed. Spectral domain OCT images were exported to ImageJ computer software.11, 13 The ImageJ is a Java-based image processing and analysis freeware developed under National Institutes of Health (NIH, Bethesda, MD, USA).11 It can calculate distances, angles, areas, intensity, and pixel value statistics on an image. This software is widely used in basic and clinical research for many years.11, 12, 13, 14 In recent years, increasing number of studies showed that ImageJ is a reliable tool and it has high inter- and intraobserver reproducibility in the field of ophthalmology.15, 16, 17
A single masked physician (IT) analyzed randomly selected OCT images using ‘plot profile’ function of ImageJ (Figure 1).11, 13 A vertical straight line was drawn from vitreous cavity to choroid passing through the center of fovea (Figure 1).13 The software gave reflectivity values along this line and a reflectivity graph was created (Figure 1). In a normal OCT image, RPE layer has the highest reflectivity followed by IS/OS junction and ELM in histologic order. Based on these data, on the reflectivity graph, highest value was accepted as the reflectivity of RPE layer. Furthermore, locations of RPE layer, IS/OS junction, and ELM on OCT image were confirmed simultaneously on the reflectivity graph using ‘live’ plot profile function of the software. Reflectivity values of each retinal layer were noted and converted to ‘relative reflectivity’ according to the following formula.
Gray-scale OCT images (left) of a control subject (a) and IEMM patient (b), and peaks of RPE, photoreceptor IS/OS junction, and ELM on reflectivity graph (right) obtained from image processing program (ImageJ) are shown. ImageJ gives reflectivity values along a line (vertical white arrow) and creates reflectivity graph.
Relative reflectivity (arbitrary unit)=(reflectivity of IS/OS or ELM)/(reflectivity of RPE) × 100.
Based on the current literature, lower reflectivity was considered as functional or structural impairment in related retinal layers.18, 19
Statistical analysis
The Statistical Package for Social Sciences software version 16.0 (SPSS Inc., Chicago, IL, USA) was used for statistical analysis. Results were expressed as mean±standard deviation (SD). χ2 Test was used to compare two groups in terms of gender. Comparison of the quantitative data (age, reflectivity) between two groups was performed by independent sample t-test. Pearson’s correlation coefficients were used to determine associations among visual acuity, age, and reflectivity values. A P-value <0.05 was considered statistically significant at 95% confidence interval.
Results
The study group comprised 50 eyes of 50 patients with untreated IEMM (patient group) and 41 eyes of 41 healthy subjects with normal OCT (control group). Comparing two groups, there were no significant difference in terms of age and gender (P>0.05). Table 1 shows sociodemographic characteristics of the study population. In the patient group, mean CDVA was 0.43±0.23 logMAR (20/53 Snellen equivalent).
We retrospectively reviewed OCT data of all subjects, and image analysis was performed randomly to determine reflectivities of RPE, IS/OS junction, and ELM.
In the patient group, IS/OS junction and ELM reflectivities (absolute and relative) were significantly lower when compared with those of the control group (Table 2). However, RPE reflectivity did not show significant difference between two groups (Table 2).
In patients with IEMM, correlation analysis revealed a significant relation between CDVA (logMAR) and age (r=0.386, P=0.009), although correlations between CDVA and reflectivity measurements were not statistically significant (P>0.05).
Discussion
IEMM is a relatively common ocular entity, and it is characterized by collagenous proliferation on inner retinal surface without a secondary cause.1, 2 Contractile nature of these membranes causes disturbance on macular microarchitecture and patients experience metamorphopsia or decrease in visual acuity.3
Since the introduction of high-resolution OCT devices, physicians have chance to obtain detailed images of retinal layers before and after treatment. In recent years, most of the studies focused on photoreceptor IS/OS junction on OCT scans and integrity of this layer was reported as a prognostic factor for postoperative visual improvement in many retinal diseases.7, 8, 9, 10, 20, 21 Michalewski et al6 sought correlations between macular morphology and visual acuity in patients with EMM using OCT. They reported that macular morphology and photoreceptor defects seemed to be prognostic factors in patients with EMM. Similarly, many studies concluded that disruption in IS/OS junction was an important predictor of poor visual outcome in eyes with IEMM.5, 10, 22, 23
In the current literature, studies identified two main pathologic patterns in IS/OS junction (disruption and absence), which were suggested to be irreversible.5, 22, 23 Thus, it can be valuable to detect subclinical deteriorations even if photoreceptor IS/OS junction appears to be intact on OCT image. In the present study, we analyzed reflectivities of RPE, IS/OS junction, and ELM on OCT scans using a medical image processing software to determine functional status of these retinal layers in patients with IEMM. We found significant decreases in IS/OS junction and ELM reflectivities (both absolute and relative) compared with those of the healthy eyes, whereas RPE reflectivity did not show a significant difference between the patient and control groups. In a healthy macula, IS/OS junction can be seen as a continuous hyper-reflective band on OCT image, and recent studies demonstrated that decreased reflectivity of this layer is associated with diminished photoreceptor function.18, 19 Based on this knowledge, loss of reflectivity in IS/OS junction and ELM might indicate that EMM leads to subclinical functional or structural impairment in these layers. However, correlation analysis did not show a significant association between reflectivity values and CDVA.
In patients with IEMM, clinical symptoms vary on distortionary effect of membrane on macular microstructure. Although recent studies agreed that disrupted or absent IS/OS junction on OCT scan (which could be irreversible) was an important predictor of poor visual acuity.9, 10, 22, 23 Early effects of IEMM on functions of retinal layers were not reported previously to the best of our knowledge.
In conclusion, our study revealed that IEMM might lead to subclinical deteriorations in IS/OS junction and ELM even though patient has a continuous IS/OS junction and ELM on OCT scan.

References
Fraser-Bell S, Guzowski M, Rochtchina E, Wang JJ, Mitchell P . Five-year cumulative incidence and progression of epiretinal membranes: the Blue Mountains Eye Study. Ophthalmology 2003; 110: 34–40.
Smiddy WE, Maguire AM, Green WR, Michels RG, de la Cruz Z, Enger C et al. Idiopathic epiretinal membranes: ultrastructural characteristics and clinicopathologic correlations. Ophthalmology 1989; 96: 811–820.
Seidel G, Weger M, Stadlmüller L, Pichler T, Haas A . Association of preoperative optical coherence tomography markers with residual inner limiting membrane in epiretinal membrane peeling. PLoS One 2013; 8: e66217.
Oh HN, Lee JE, Kim HW, Yun IH . Clinical outcomes of double staining and additional ILM peeling during ERM surgery. Korean J Ophthalmol 2013; 27: 256–260.
Suh MH, Seo JM, Park KH, Yu HG . Associations between macular findings by optical coherence tomography and visual outcomes after epiretinal membrane removal. Am J Ophthalmol 2009; 147: 473–480.
Michalewski J, Michalewska Z, Cisiecki S, Nawrocki J . Morphologically functional correlations of macular pathology connected with epiretinal membrane formation in spectral optical coherence tomography (SOCT). Graefes Arch Clin Exp Ophthalmol 2007; 245: 123–131.
Inoue M, Watanabe Y, Arakawa A, Sato S, Kobayashi S, Kadonosono K . Spectral-domain optical coherence tomography images of inner/outer segment junctions and macular hole surgery outcomes. Graefes Arch Clin Exp Ophthalmol 2009; 247: 325–330.
Oh J, Smiddy WE, Flynn HW Jr, Gregori G, Lujan B . Photoreceptor inner/outer segment defect imaging by spectral domain OCT and visual prognosis after macular hole surgery. Invest Ophthalmol Vis Sci 2010; 51: 1651–1658.
Kunikata H, Abe T, Kinukawa J, Nishida K . Preoperative factors predictive of postoperative decimal visual acuity ≥1.0 following surgical treatment for idiopathic epiretinal membrane. Clin Ophthalmol 2011; 5: 147–154.
Oster SF, Mojana F, Brar M, Yuson RM, Cheng L, Freeman WR . Disruption of the photoreceptor inner segment/outer segment layer on spectral domain-optical coherence tomography is a predictor of poor visual acuity in patients with epiretinal membranes. Retina 2010; 30: 713–718.
Rasband W . Image J Medical Imaging Software. National Institutes of Health: Bethesda, MD, USA, Available at http://rsb.info.nih.gov/ij/. Last accessed 10 November 2013.
Holladay JT, Prager TC . Mean visual acuity. Am J Ophthalmol 1991; 111: 372–374.
Murakami T, Nishijima K, Akagi T, Uji A, Horii T, Ueda-Arakawa N . Optical coherence tomographic reflectivity of photoreceptors beneath cystoid spaces in diabetic macular edema. Invest Ophthalmol Vis Sci 2012; 53: 1506–1511.
Collins TJ . ImageJ for microscopy. Biotechniques 2007; 43: 25–30.
Kim US, Kim SJ, Baek SH, Kim HK, Sohn YH . Quantitative analysis of optic disc color. Korean J Ophthalmol 2011; 25: 174–177.
Zhao WJ, Duan F, Li ZT, Yang HJ, Huang Q, Wu KL . Evaluation of regional bulbar redness using an image-based objective method. Int J Ophthalmol 2014; 7: 71–76.
Nadler Z, Wang B, Wollstein G, Nevins JE, Ishikawa H, Bilonick R et al. Repeatability of in vivo 3D lamina cribrosa microarchitecture using adaptive optics spectral domain optical coherence tomography. Biomed Opt Express 2014; 5: 1114–1123.
Bizheva K, Pflug R, Hermann B, Povazay B, Sattmann H, Qiu P . Optophysiology: depth-resolved probing of retinal physiology with functional ultrahigh-resolution optical coherence tomography. Proc Natl Acad Sci USA 2006; 103: 5066–5071.
Hood DC, Zhang X, Ramachandran R, Talamini CL, Raza A, Greenberg JP . The inner segment/outer segment border seen on optical coherence tomography is less intense in patients with diminished cone function. Invest Ophthalmol Vis Sci 2011; 52: 9703–9709.
Wakabayashi T, Oshima Y, Fujimoto H, Murakami Y, Sakaguchi H, Kusaka S . Foveal microstructure and visual acuity after retinal detachment repair. Ophthalmology 2009; 116: 519–528.
Sakamoto A, Nishijima K, Kita M, Suzuma K, Watanabe D, Oh H . Association between foveal photoreceptor status and visual acuity. after resolution of diabetic macular edema by pars plana vitrectomy. Graefes Arch Clin Exp Ophthalmol 2009; 247: 1325–1330.
Inoue M, Morita S, Watanabe Y, Kaneko T, Yamane S, Kobayashi S . Preoperative inner segment/outer segment junction in spectral-domain optical coherence tomography as a prognostic factor in epiretinal membrane surgery. Retina 2011; 31: 1366–1372.
Cobos E, Arias L, Ruiz-Moreno J, Rubio M, Garcia-Bru P, Caminal J . Preoperative study of the inner segment/outer segment junction of photoreceptors by spectral-domain optical coherence tomography as a prognostic factor in patients with epiretinal membranes. Clin Ophthalmol 2013; 7: 1467–1470.
Acknowledgements
This study was performed in adherence to the tenets of the Declaration of Helsinki and Local Ethics Committee approved the study.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Rights and permissions
About this article
Cite this article
Toprak, I., Yaylalı, V. & Yildirim, C. Decreased photoreceptor inner segment/outer segment junction reflectivity in patients with idiopathic epimacular membrane. Eye 28, 1126–1130 (2014). https://doi.org/10.1038/eye.2014.147
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/eye.2014.147
This article is cited by
-
Early deterioration in ellipsoid zone in eyes with non-neovascular age-related macular degeneration
International Ophthalmology (2017)