Abstract
Aim
To assess the prevalence of retrodots and vacuoles and their associations with the prevalence and long-term incidence of age-related cataract in an older Australian cohort.
Methods
Of 3654 baseline participants of the Blue Mountains Eye Study aged 49+ years (1992–1994), 2335 and 1952 were re-examined after 5 and 10 years, respectively. Lens photographs were graded for cataract, retrodots, and vacuoles. Eye-specific data were used to assess the associations between retrodots or vacuoles at baseline and the prevalence and 10-year incidence of nuclear, cortical, and posterior subcapsular (PSC) cataract and cataract surgery.
Results
At baseline, retrodots were present in 142 persons (4%) and vacuoles in 1333 persons (40%). Prevalence of both lens features increased with increasing age (Pfor trend <0.0001). After adjusting for age and gender, vacuoles were associated with prevalent PSC cataract at baseline (odds ratio (OR), 1.60, 95% confidence interval (CI), 1.25–2.05). After adjusting for age, gender, smoking, hypertension, diabetes, education, and use of inhaled/oral steroids, baseline retrodots were associated with an increased incidence of cataract surgery (OR 2.90, 95% CI 1.71–4.91), while 3+ vacuoles at baseline were associated with an increased risk of PSC cataract (OR 3.56, 95% CI 2.13–5.95) and cataract surgery (OR 1.84, 95% CI 1.22–2.77).
Discussion
Lens retrodots and vacuoles were found to be positively associated with 10-year incidence of cataract surgery, and vacuoles associated with PSC cataract, a finding suggestive of shared risk factors or pathogenesis between these two lens features and the development of PSC cataract.
Similar content being viewed by others
Introduction
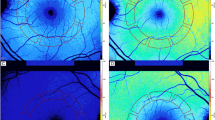
Retrodots and vacuoles (Figure 1) are non-opaque lens changes that appeared, initially, to have little apparent impact on visual function.1, 2 Retrodots3 are also known as spheroliths,4 cystoid spaces,2 calcium-containing opacities,5 or white anterior cortical opacities.6 They were first reported in the 1910s and described as ‘a relief pattern of bumps and knobs’.7 Later, retrodots were more accurately described as small, discrete, birefringent, rounded, or lobular objects (Figure 1a), typically found in the cortical regions of the lens with a higher refractive index than the surrounding lens material.2 More recently, retrodots have been found to be associated with visual impairment.8, 9
Vacuoles, in contrast, have not been extensively studied. They are clear, spherical, and fluid-filled spaces within the lens cortex (Figure 1b). The illumination of vacuoles suggests that they contain fluid of lower refractive index than the surrounding lens material.10 They typically occur in isolation, although they can also be a component of posterior subcapsular (PSC) cataract, and are thought to be transient in nature.1, 11, 12 They vary in size (∼10 μm–1.3 mm in diameter1) and appear to have minimal effect on vision.1, 8, 9
The prevalence of retrodots varies from 3.4 to 39% (Table 1).5, 7, 8, 9, 13, 14 Risk factors identified to be associated with retrodots include alcohol consumption, high serum levels of high-density lipoprotein cholesterol,15 and smoking.9 Retrodots have previously been documented to be associated with nuclear cataract.16, 17 Both retrodots and vacuoles are considered to be oxidative stress related.16 The prevalence of vacuoles varies from 5 to 59% (Table 1).8, 12, 13, 14 Reports of risk factors associated with lens vacuoles are unavailable in the literature.
Although these features have previously been suggested as indicators of early cataractous changes,17 only one longitudinal study9 had investigated their associations with subsequent development of age-related cataract or cataract surgery. We therefore aimed in this study to investigate the longitudinal associations between baseline retrodots and vacuoles (documented using lens photography) and subsequent development of age-related cataract and incident cataract surgery over 10 years.
Materials and methods
Study population
The Blue Mountains Eye Study is a population-based cohort study of vision and other common eye diseases in a population aged 49 years and older. During 1992–1994, 3654 persons (82.4% of those eligible) living in two postcode areas of the Blue Mountains region, west of Sydney, participated in the baseline survey and examinations. Approximately 75% of surviving participants were followed at each of the 5 year (1997–1999, n=2335, 63.9% of the original cohort) and 10 year (2002–2004, n=1952, 53.4% of the original cohort) examinations.18 Participants who were lost to follow-up were younger, more likely to be current smokers, to have diabetes and a lower health-related quality of life, but were less likely to own their home than those followed at each of the follow-up examinations.18
Written informed consent was obtained from all participants at each visit. The study adhered to the recommendations of the Declaration of Helsinki, and approval from the Western Sydney Area Health Service Human Research Ethics Committee was obtained. The same procedures were used for all three examinations.
Examination methods and procedures have been described previously.19, 20 Briefly, participants underwent a comprehensive eye examination including lens photography, subjective refraction using a logarithm of the minimum angle of resolution (LogMAR) chart and interviewer-administered questionnaires to collect medical histories and demographic information.
Cataract grading
Retroillumination (Neitz CT-R, Neitz Instruments, Tokyo, Japan) and slit-lamp (Topcon SL-7e, Topcon Optical, Tokyo, Japan) lens photographs taken during the examinations were graded for cataract. Details of photographic and grading procedures used at all three examinations have been described.20 Retrodots, vacuoles, cortical, and PSC cataract were assessed from anterior and posterior retroillumination photographs (as shown in Figure 1), by laying a grid over the lens photographs to determine the location of opacities. The grid consists of eight wedge-shaped segments and a central circle. The presence of retrodots was assessed for each segment of the grid. Vacuoles were enumerated.
The total area of involvement by cortical or PSC opacity was calculated. Cortical cataract was defined as cortical opacity ≥5% of the total lens area. PSC cataract was defined if any such opacity was present. Nuclear cataract was evaluated by comparing participant slit-lamp photos to a set of standards representing various degrees of nuclear opacity. Nuclear opacity denser than Wisconsin Standard Photo #3 was graded as nuclear cataract present. Cataract surgery was confirmed by the presence of pseudophakia or aphakia on retroillumination or slit-lamp lens photographs. If participants did not have gradable lens photographs, self-reported history of cataract surgery, confirmed during the eye examinations, was used instead.
Statistical analysis
Analyses were performed using SAS version 9.1. 3 (SAS Institute, Cary, NC, USA). Subject-specific data were used for the baseline characteristics, and refractive status was defined using the worse eye. Baseline age and gender distribution of retrodots and vacuoles for both right and left eyes were examined, but only results from right eyes were reported, because findings were similar between the two eyes. To investigate associations with increasing severity of retrodots and vacuoles, they were each divided into three groups (retrodots: absence, presence in 1–3 subfields or 4+ subfields; vacuoles: absence, presence of 1–2 vacuoles or 3+ vacuoles). The mean number of letters read correctly on the LogMAR chart was an indicator of visual acuity (VA). Comparisons of mean VA were made among the three groups of retrodots and the three groups of vacuoles, after adjusting for age, gender, and any cataract. Mild visual impairment was defined as VA <20/40 to 20/80, moderate to severe visual impairment was defined as VA <20/80. Visual impairment refers to mild or worse levels of visual impairment.
Eye-specific data were used to determine the associations between retrodots or vacuoles (independent variables) at baseline and the prevalence (cross-sectional analysis) or subsequent development of nuclear, cortical, or PSC cataract or cataract surgery (dependent variables), either at the 5- or 10-year follow-up visits (longitudinal analysis). Only eyes with no cataract at baseline (at risk of cataract) were included in the longitudinal analyses. We excluded eyes with vacuoles from the analyses of associations with retrodots and excluded eyes with retrodots in the analyses of associations with vacuoles.
Generalised linear model was used to investigate eye-specific associations between baseline retrodots, vacuoles, visual impairment, and cataract (eye as the study unit) while accounting for correlation between the two eyes by generalised estimating equations.21, 22 We adjusted for age and gender in the cross-sectional analysis involving retrodots, vacuoles, and cataract. In the cross-sectional analysis involving visual impairment, we adjusted for age, gender, and presence of cataract. Discrete logistic regression23 was used to assess the association between baseline retrodots and vacuoles and incidence of each cataract type incorporating discrete time information from both follow-up visits. The following potential confounders were adjusted for in the longitudinal analyses: age, gender, smoking, diabetes, hypertension, education, and use of inhaled or oral steroids. For incident cataract surgery, we additionally adjusted for the presence of cataract at baseline. Odds ratios (OR) and 95% confidence intervals (CI) are presented.
Results
Retrodots
At baseline, retrodots were found in 142 persons (4%) or in 178 eyes (3%). The baseline characteristics of participants with and without retrodots, and with and without vacuoles, are shown in Table 2. Participants with retrodots were older, more likely to be past or never smokers and to have a history of hypertension than those without retrodots.
Prevalence of retrodots in right eyes increased from 0.4% in people aged <60 years to 15.2% in those aged 80+ years (Figure 2, P for trend <0.0001), with no gender difference. Retrodots were more frequent in eyes with cataract, particularly cortical and nuclear cataract, observed from baseline data. However, after adjusting for age and gender, retrodots were only associated with the prevalence of cortical cataract (any retrodots: OR 1.46, 95% CI, 1.01–2.10; retrodots in 4+ subfields: OR 2.04, 95% CI 1.27–3.28; Table 3).
In cross-sectional analyses using baseline data, we found that mean VA of the three retrodot groups decreased with increasing severity of retrodots before adjusting for age, gender, and cataract at baseline (52.6 vs 48.9 vs 43.9 for no retrodots, retrodots involving 1–3 subfields and retrodots involving 4+ subfields, respectively, P for trend<0.0001). After this adjustment, there was little difference in mean VA between the three groups (52.5 vs 53.0 vs 50.8 for the three severity levels, respectively, P for trend=0.30). Retrodots were associated with the presence of visual impairment: 18.0% of eyes with retrodots while only 6.1% of eyes without retrodots were visually impaired. Further to this, 22.6% of eyes with retrodots involving 4+ subfields had mild visual impairment (VA <20/40 to 20/80); while only 3.5% of eyes with retrodots involving 1–3 subfields and 3.4% of eyes without retrodots had mild visual impairment. The association between retrodots involving 4+ subfields and visual impairment remained significant after adjusting for age, gender, and cataract at baseline (OR 1.96, 95% CI 1.18–3.24; Table 3).
After excluding those lost to follow-up and eyes with vacuoles at baseline, 45.2, 23.2, and 4.6% of eyes with retrodots at baseline developed nuclear, cortical, and PSC cataract, respectively, over 10 years, while 37.7% underwent cataract surgery during this period, compared with 23.4%, 16.4%, 3.6%, and 10.5%, respectively, for eyes without retrodots at baseline (Table 4). The presence of any retrodots at baseline was associated with nearly threefold higher likelihood of having incident cataract surgery (OR 2.90, 95% CI 1.70–4.91), after adjusting for age, gender, smoking, diabetes, hypertension, education, use of inhaled and oral steroids, and presence of baseline cataract. There was an increasing risk of incident cataract surgery associated with increase in the number of subfields with retrodots (1–3 subfields: OR 2.15, 95% CI 1.01–4.60; 4+ subfields: OR 4.40, 95% CI 2.06–9.40), after multivariable adjustment. There were no significant associations of baseline retrodots with incident nuclear, cortical, or PSC cataract (Table 4).
Vacuoles
Vacuoles were found in 1333 persons (40%) or in 1734 eyes (25%). Most eyes (74%) had 1–2 vacuoles present (Figure 3). Participants with vacuoles were more likely to be female, to have a history of diabetes or hypertension; they were also more likely to be either myopic or hyperopic than those without vacuoles (Table 2).
Prevalence of vacuoles in the right eyes also increased with increasing age (P for trend <0.0001), occurring in 32% of persons aged <60 years and 51% of those aged 80+ years (Figure 2). Vacuoles were more frequent in women (26.3%) than men (23.2%, P=0.04). Vacuoles were also more frequent in eyes with cataract, observed from baseline data (Table 3). After adjusting for age, and gender, increased odds for PSC cataract was found for eyes with vacuoles present (any: OR 1.60, 95% CI 1.25–2.05; 3+ vacuoles: OR 2.75, 95% CI 1.89–4.01; Table 3).
The mean VA of the three vacuole groups decreased with increasing severity of vacuoles before adjusting for age, gender, and cataract at baseline (52.6 vs 52.0 vs 48.7 letters for eyes with no vacuoles, 1–2 vacuoles and 3+ vacuoles, respectively, P for trend <0.0001) and after adjustment (52.4 vs 52.7 vs 50.8 letters for eyes with no vacuoles, 1–2 vacuoles and 3+ vacuoles, respectively, P for trend=0.038). In all, 8.3% of eyes with vacuoles and 6.1% of eyes without vacuoles were visually impaired at baseline. Further, 9.1% of eyes with 3+ vacuoles had mild visual impairment while 3.4 and 4.1% of eyes with 1–2 vacuoles or no vacuoles, respectively, had mild visual impairment at baseline. Eyes with 3+ vacuoles had a 50% increase in the odds of visual impairment, after adjusting for age, gender, and cataract at baseline (OR 1.52, 95% CI 1.11–2.08; Table 3).
After excluding persons lost to follow-up and eyes with retrodots at baseline, 25.7%, 17.5%, and 7.2% of eyes with any vacuoles at baseline developed nuclear, cortical, and PSC cataract, respectively, over 10 years compared with 23.7%, 16.4%, and 3.6%, respectively, for eyes without vacuoles at baseline. Furthermore, 15.2% of eyes with vacuoles and 10.5% of eyes without vacuoles at baseline required cataract surgery over the follow-up period (Table 4). After multivariable adjustment, the presence of any vacuoles at baseline was associated with nearly twofold risk of developing PSC cataract (any vacuoles: OR 1.94, 95% CI 1.41–2.69; Table 4). Increasing number of vacuoles was associated with greater risk of developing PSC cataract, compared with eyes with no vacuoles (1–2 vacuoles: OR 1.57, 95% CI 1.08–2.28; 3+ vacuoles: OR 3.56, 95% CI 2.13–5.95). The presence of 3+ vacuoles at baseline was also associated with a near twofold greater risk of having subsequent cataract surgery (OR 1.84, 95% CI 1.22–2.77), after adjusting for age, gender, smoking, diabetes, hypertension, education, use of inhaled or oral steroids, and the presence of any cataract at baseline (Table 4).
Discussion
In this population-based cohort of older Australians, we found that retrodots were relatively uncommon, whereas vacuoles were much more frequent than retrodots in the lenses of older persons. We observed longitudinal associations between retrodots at baseline and subsequent cataract surgery. Participants with vacuoles at baseline were more likely to have subsequent cataract surgery, as well as being at higher risk of developing PSC cataract, over the following 10 years.
Our finding of prevalence of retrodots in this sample of predominantly Caucasian participants aged 49+ years is comparable with that from some other population-based studies (Table 1). The Beaver Dam Eye Study (BDES), which used the same lens photographic grading protocol as our study, reported a 4.9% prevalence of retrodots in a sample of Caucasian adults aged 43+ years.9 Other studies of older populations, however, reported a substantially higher prevalence of retrodots, including the Melton Eye Study,13 the Somerset and Avon Eye Study,8 and the Monzen Eye Study14 (Table 1). The wide differences in prevalence estimates could have been due to different study samples and different methods used across studies, particularly detection of retrodots by different observers. Consistent with other population-based and clinic-based studies,8, 12, 13, 14 we found that the prevalence of retrodots increased with increasing age.
Retrodots are often found with cataract and previous studies have reported cross-sectional associations between retrodots and nuclear cataract.9, 16, 17 Data from our study could not confirm this previously reported cross-sectional association. However, we did observe a cross-sectional association between cortical cataract and retrodots, particularly when retrodots were present in four or more subfields. As ours is the only population-based study to have documented this cross-sectional association, but did not show a longitudinal association of retrodots with incident cortical cataract, we cannot exclude the possibility of a chance finding.
The observed association of retrodots at baseline with a twofold greater risk of subsequent cataract surgery over 10 years, independent of any other type of cataract at baseline, suggests that this sign may be a marker of progressive lens opacity leading to cataract surgery, a finding consistent with the BDES observations.9 It is unclear as to what processes are involved in eyes that have both retrodots and more rapid development of cataract, and thus need for cataract surgery. However, an association between retrodots and visual impairment suggests that retrodots may be causing some visual disturbance. Also, we cannot exclude the possibility that retrodots may have an effect on other measures of visual function, such as glare or contrast sensitivity, as reported by other studies,6, 8, 9 which could in turn affect patients’ perception of vision and their vision-related daily activities. However, we did not measure glare or contrast sensitivity in the cohort, so were unable to investigate reasons behind this association.
Vacuoles were a common lens feature in this population, consistent with findings from other population-based and clinic-based studies.8, 12, 13, 14 However, contrary to those studies, the prevalence of vacuoles in our study sample increased with age. Eyes with 3+ vacuoles had significantly lower VA than those without vacuoles, which could be partly explained by their low refractive property.10 However, the two-letter reduction in mean VA may not be clinically significant, and so could not entirely account for its association with a near twofold greater long-term risk of cataract surgery. The link between vacuole presence and subsequent cataract surgery could be explained by the association between vacuoles and PSC cataract, as this type of cataract often needs surgery sooner than other types of cataract.
Vacuoles have previously been considered to be a component of PSC cataract,1 so that the association found between vacuoles at baseline and the prevalence and incidence of PSC cataract would be expected. A study documenting PSC cataract development over time suggested that vacuoles were transient in nature, and that their disappearance was sometimes replaced by PSC cataract.11 Whether vacuoles are consistent precursors of clinical PSC cataract remains to be clarified. In our study, we are not able to confirm this longitudinal observation, as we assessed these lens opacities from the baseline lens images only.
Strengths of our study include its long-term follow-up of a defined population-based sample and the use of a similar examination and lens photographic grading protocol across all three study visits. Possible unknown confounding factors that were not measured in our study could have biased the associations observed. Participants lost to follow-up differed from those who participated in age, smoking status, and diabetes.18 As these are risk factors for cataract, such differences could have led to an underestimation of cataract incidence. However, sensitivity analyses treating those lost to follow-up as either (1) all having cataract (or cataract surgery) developed over the follow-up period; or (2) all remaining free of cataract (or cataract surgery) during the follow-up period, both showed significant ORs with the same association direction, with only a slight attenuation of the risk magnitudes (data not shown). These findings support the robustness of our estimates.
In conclusion, we found that the prevalence of retrodots and vacuoles increased with age in an older Australian cohort. Vacuoles were associated with a higher risk of prevalent and incident PSC cataract, while the presence of three or more vacuoles or the presence of any retrodots at baseline was associated with an increased likelihood of subsequent cataract surgery. Confirmation of our study findings and understanding of the links between these lens features and PSC cataract warrants further study.

References
Brown NP, Shun-Shin GA . Morphological correlations of clinical lens changes: non-opaque lens defects. Prog Retin Eye Res 1995; 14: 453–472.
Reese AB, Wadsworth JA . The occurrence of cystoid spaces in the lens. Trans Am Ophthalmol Soc 1953; 51: 307–311.
Bron AJ, Matsuda K . Specular microscopy of the human lens. Trans Ophthalmol Soc UK 1981; 101: 163–169.
Pau H, Kaufmann R . Laser microprobe analysis (LAMMA) of spheroliths in human cataract lenses. Arch Ophthalmol 1983; 101: 1935–1937.
Harding CV, Chylack Jr LT, Susan SR, Lo WK, Bobrowski WF . Calcium-containing opacities in the human lens. Invest Ophthalmol Vis Sci 1983; 24: 1194–1202.
Klein BE, Klein R, Knudtson MD . Lens opacities associated with performance-based and self-assessed visual functions. Ophthalmology 2006; 113: 1257–1263.
Bron AJ, Brown NA . Perinuclear lens retrodots: a role for ascorbate in cataractogenesis. Br J Ophthalmol 1987; 71: 86–95.
Frost NA, Sparrow JM, Moore L . Associations of human crystalline lens retrodots and waterclefts with visual impairment: an observational study. Invest Ophthalmol Vis Sci 2002; 43: 2105–2109.
Klein BE, Meuer SM, Lee KE, Klein R . Retrodots in the lens in the Beaver Dam Eye Study cohort. Ophthalmology 2010; 117: 1889–1893.
Brown N . Visibility of transparent objects in the eye by retroillumination. Br J Ophthalmol 1971; 55: 517–524.
Adrien Shun Shin G, Brown NP, Bron AJ, Sparrow JM . Dynamic nature of posterior subcapsular cataract. Br J Ophthalmol 1989; 73: 522–527.
Palmquist BM, Fagerholm PP, Philipson BT . Nuclear vacuoles in nuclear cataract. Acta Ophthalmol (Copenh) 1986; 64: 63–66.
Deane JS, Hall AB, Thompson JR, Rosenthal AR . Prevalence of lenticular abnormalities in a population-based study: Oxford clinical cataract grading in the Melton Eye Study. Ophthalmic Epidemiol 1997; 4: 195–206.
Qu J, Sasaki H, Fujisawa A, Kaneda J, Nagai K, Shima I et al. [Prevalence of lens opacity types except three major ones in Monzen Eye Study]. Rinsho Ganka 2005; 59: 903–906.
Durant JS, Frost NA, Trivella M, Sparrow JM . Risk factors for cataract subtypes waterclefts and retrodots: two case-control studies. Eye 2006; 20: 1254–1267.
Shun Shin GA, Bron AJ, Brown NP, Sparrow JM . The relationship between central nuclear scatter and perinuclear retrodots in the human crystalline lens. Eye 1992; 6: 407–410.
Thompson JR, Deane JS, Hall AB, Rosenthal AR . Associations between lens features assessed in the Oxford Clinical Cataract Classification and Grading System. Ophthalmic Epidemiol 1997; 4: 207–212.
Kanthan GL, Wang JJ, Rochtchina E, Tan AG, Lee A, Chia EM et al. Ten-year incidence of age-related cataract and cataract surgery in an older Australian population: the Blue Mountains Eye Study. Ophthalmology 2007; 115: 808–814.
Mitchell P, Smith W, Attebo K, Wang JJ . Prevalence of age-related maculopathy in Australia. The Blue Mountains Eye Study. Ophthalmology 1995; 102: 1450–1460.
Mitchell P, Cumming RG, Attebo K, Panchapakesan J . Prevalence of cataract in Australia: the Blue Mountains eye study. Ophthalmology 1997; 104: 581–588.
Zeger SL, Liang KY, Albert PS . Models for longitudinal data: a generalized estimating equation approach [published erratum appears in Biometrics 1989; 45(1): 347]. Biometrics 1988; 44: 1049–1060.
Liang KY, Zeger SL . Longitudinal data analysis using generalized linear models. Biometrika 1986; 73: 13–22.
Hosmer DW, Lemeshow S . Applied Logistic Regression. John Wiley & Sons Inc: New York, NY, 1989, pp 238–245.
Acknowledgements
This study was supported by the National Health and Medical Research Council, Australia (Grant nos 974159 and 211069).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Rights and permissions
About this article
Cite this article
Tan, A., Mitchell, P., Rochtchina, E. et al. Lens retrodots and vacuoles and their associations with the prevalence and incidence of age-related cataract. Eye 26, 568–575 (2012). https://doi.org/10.1038/eye.2011.349
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/eye.2011.349